Interdisciplinary orthodontics
Orthodontic treatment of adults has been the fastest growing area in orthodontics in recent years. Many orthodontic practises today include 45% of patients as adults. This is probably because of an increased awareness of malocclusion and functional benefits of orthodontic treatment. In addition to aesthetics, recent advances in orthodontic materials, aesthetically pleasing and biomechanically sound appliances, and interdisciplinary treatment philosophy have all played an important role in making orthodontic treatment popular in adult population. This chapter presents the philosophy and treatment approach needed to bring together a diverse group of professionals into a cohesive team to provide treatment strategies for adult patient. It explains existing and new orthodontic, periodontic, surgical and restorative techniques that provide the best possible solution to complex dentofacial problems.
In clinical practise, orthodontic treatment of adults may be somewhat different from that of most adolescents.1 Adult patients are usually motivated for improved oral hygiene, and they are cooperative. Compared with adolescents, adults are more likely to have dentitions that have undergone some degree of mutilation over a period of time. In addition to the malaligned teeth and jaws, adult orthodontic patients may have other problems that demand some alterations in treatment strategy. These include excessive tooth wear, missing teeth, restored teeth, periodontally compromised teeth, endodontically involved teeth etc., which make the treatment more challenging. In such clinical situations, orthodontist needs to coordinate treatment with other specialist or multiple specialists in order to optimize the treatment results.2,3
This involvement of various specialists like orthodontist, prosthodontist, periodontist and endodontist should be maintained with active communication among themselves throughout treatment, from the diagnosis and treatment planning stages through to the completion of active treatment and into the retention phase. In adult patients having periodontally compromised dentition with significant bone and attachment loss, conventional approach to orthodontic tooth movement does not produce the desired results, as this may lead to increased tipping of teeth.4 Therefore, in such clinical situations, entirely different bio-mechanical strategies are required for efficient and desired tooth movement.5 Absence of growth potential in adults as opposed to growing patients is another factor that influences the orthodontic treatment strategy to resolve adult malocclusions.
Interdisciplinary Philosophy
An interdisciplinary dentofacial therapy is the effective and efficient utilization of the expertise and skills in the various disciplines of dentistry.6 Its key is the combination of diagnostic, treatment planning and therapeutic procedures with extensive communication among the team members. An interdisciplinary approach to the management of complex dentofacial problems produces consistent optimal results. By providing solutions to variety of problems, an interdisciplinary treatment simplifies and idealizes the treatment plan that improves the overall treatment prognosis and enhances the treatment results.
Diagnostic and treatment planning process
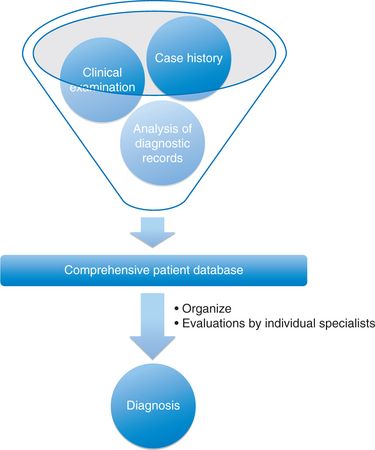
Establishing proper diagnosis is the most important step to formulate the treatment plan and to prevent any complications and confusion in the final treatment. The goal of the diagnostic process in an interdisciplinary treatment is to produce a comprehensive but concise list of patient’s problems and to synthesize the various treatment options into a plan that gives maximum benefit to the patient. In diagnosis and treatment planning, the orthodontist should
This database is then well structured and organized in such a way that it gives a systematic description of the patient’s problems that can be easily referred to during the treatment planning process. This leads to a development of a problem list. While arranging the database of a complex dentofacial problem in a systematic manner, if the problem list becomes very extensive, it is advisable to classify the problem list into various areas like orthodontic problem list, restorative problem list and periodontal problem list (Fig 11.2).
Defining treatment goals
Since the problem list of the complex dentofacial abnormalities is multifaceted and involves multiple disciplines of dentistry, it is extremely important to address the patient’s main concern, i.e. chief complaint, whether the patient is seeking treatment for functional or aesthetic improvement or both, while formulating the treatment plan. The treatment planning process in an interdisciplinary therapy involves finding a solution to each individual problem that leads to the formulation of a definitive treatment plan.7 The key here is to follow a logical sequence to develop an interdisciplinary problem list, which can be synthesized to establish a final treatment plan. The entire process of treatment planning is focused on arriving at an unbiased treatment plan that promotes optimal overall treatment results. This may involve a compromise of individual concerns of different members of an interdisciplinary team like prosthodontist, periodontist and orthodontist according to their relative importance to the overall treatment.8 A well-structured and organized list of problems makes sure that all areas have been evaluated in the diagnostic phase and also serves as a valuable reference tool during the course of treatment. All specialists involved in formulating the treatment plan for the patients should provide possible solutions to individual problems based on their own areas of expertise, and no problem should be treated as less important. These problems are then prioritized in order of importance, related to one another, and overall effects are carefully studied to establish alternate tentative treatment plans. Provisional treatment plans are then compared with respect to their overall effects, and the plan that enhances the treatment and provides maximum benefit to the patient, considering the patient’s chief complaint, is then regarded as final and definitive treatment plan.
Orthodontists should be able to visualize or foresee the final treatment outcome before implementing the definitive treatment plan. This requires that the treatment goals are clearly defined, which set the direction to the proposed treatment plan. In an adult patient with restorative and periodontal treatment needs, it should be remembered that the established treatment objectives are realistic, as opposed to idealistic treatment objectives in nonrestored adolescent patient. Economics also plays an important role in the patient’s selection of treatment plan. If the treatment goals are not economically viable, the patient may not even proceed with the restorative or periodontal treatment after orthodontic therapy. Therefore, in interdisciplinary treatment, the ideal treatment plan would be the plan that addresses maximum number of highest priority problems including the chief complaint and optimizes the treatment results with maximum benefit to the patient and with less risk involved.
Case presentation
Once the potential risks and benefits to the patient and all other factors that contribute to the optimal treatment plan have been openly and honestly discussed among the team members, it is time to schedule an appointment for case presentation. This is the most critical element of interdisciplinary therapy, as the outcome of this meeting determines whether the patient is willing to accept the proposed treatment plan or not. This meeting is aimed at making patient fully aware of his or her existing problems and possible solutions by presenting the detailed diagnostic findings, the alternative treatment plans with potential risks and benefits and the cost involved. This should be done thoroughly by using actual diagnostic records and visual aids and presentation of similar cases with pretreatment and posttreatment photographs. This definitely helps to establish the patient’s trust and confidence in the treatment providers and enhances the patient’s perceived value of therapy.7 Ideally, the multispecialist consultation with the patient is very effective; however, it may not be realistic if it is not a group practise setup.
The goal of this meeting is to make patient fully aware of his or her dentofacial problems and needs by presenting the detailed diagnostic findings and the proposed tentative treatment plans to help the patient to decide on what is important to him or her. Since the interdisciplinary treatment involves services from multiple specialists, it is important for the patient to understand the financial matters, which should be best handled by individual team members. After the patient has accepted the proposed treatment plan, it should be fine-tuned based on the outcome of the case presentation with the patient. This should be followed by a detailed outline of treatment sequence, listing the various specialists involved and making them responsible for their respective areas.
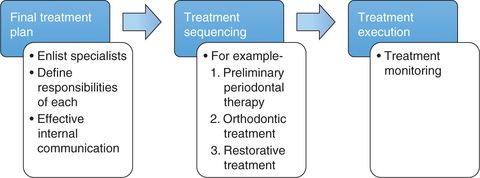
Treatment sequencing
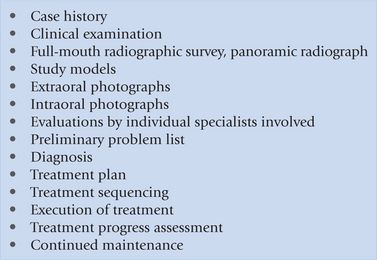
After the finalization of a definitive treatment plan, it is an important step in interdisciplinary therapy to establish the sequence of treatment. All specialists involved in providing services should meet and discuss the definitive treatment plan before it is implemented. During this meeting, it is essential that the team members understand their responsibilities and are fully aware of the planned sequence of therapy. This should be recorded, and a copy should be given to each of the team member and to the patient.7,9 This helps to make sure that the proposed plan is proceeding properly, any team specialist can review the sequence at any stage of treatment and the patient is aware of the direction and the stage of treatment completion. The treatment planning process almost always follows the same events; however, the sequence of treatment varies significantly from patient to patient based on the treatment priority. Here, the main goal is to organize the sequence of various treatment procedures into a logical order so that each intervention performed by one of the specialists from the interdisciplinary team facilitates the next in order10 (Fig 11.3). Figure 11.4 illustrates a 14-point treatment protocol for interdisciplinary cases.
Periodontally Compromised Patient
One of the most important aspects of orthodontic treatment while treating adult population is the proper assessment of their periodontal health. This should be done before the placement of fixed orthodontic appliances in order to avoid adverse iatrogenic effects on the periodontium. Adequate maintenance of dental and periodontal health is an integral part of the treatment performed by every specialist who is a part of the interdisciplinary team. Many adult patients who are the candidates for restorative treatment often have abnormal tooth positions. This compromises their ability to adequately clean their dentitions and maintain the oral hygiene, leading to periodontal breakdown. Orthodontic tooth movement plays an important role in improving the prognosis of periodontally compromised teeth.
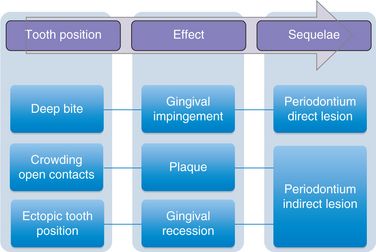
Tooth position and periodontal condition
There are several studies that show pathogenic correlation between tooth position in the dental arch and periodontal condition (Fig 11.5). An ectopically positioned tooth or a tooth that is labially placed is often associated with soft tissue breakdown, which is expressed clinically as gingival recession. Such teeth, when moved orthodontically into areas of better bone support, have been shown to partially gain attachment11–13 (Fig 11.6).
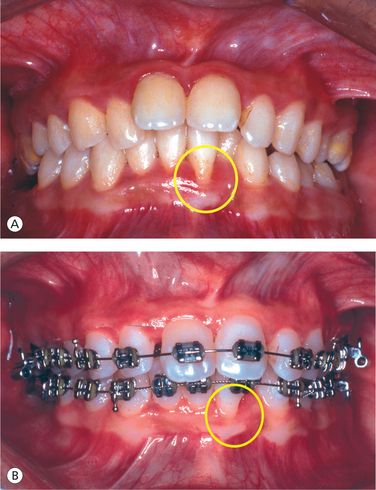
Figure 11.6 Tooth position and periodontal condition. (A) Labially positioned mandibular left central incisor associated with soft tissue breakdown. (B) Orthodontic positioning of teeth into areas of better bone support shows partial attachment gain.
Irregularity of teeth is a predisposing factor to plaque accumulation and also results in unfavourable topography of gingiva and interradicular bone. The pathologic levels of microorganisms are significantly higher in the crowded dentition than in the well-aligned teeth.14 Orthodontic correction of crowded dentition improves the topography of interdental gingiva and bone by establishing normal contact points, which in turn facilitates to adequately maintain the oral hygiene. It has been shown that the alveolar bone height is significantly reduced in regions of severe malocclusion (8 mm of overjet) as compared to the regions of normal occlusion.15
Preliminary periodontal therapy
Periodontal disease control, prior to the initiation of orthodontic treatment, contributes significantly to the success of treatment. It is extremely important to control periodontal inflammation, as the orthodontic treatment in presence of this inflammation can lead to rapid bone loss.16,17 Gingival bleeding on gentle probing is the most reliable indicator of clinically significant gingivitis.18 Excessive pocket probing depth should also be reduced with the preliminary periodontal therapy. A thorough scaling, root planing and sub-gingival curettage are often performed to keep the gingival tissues free from clinical signs of inflammation prior to and also during therapy (Fig 11.7I and J). Since the orthodontic treatment itself can often improve the topography of alveolar bone, more extensive periodontal procedures like flap and osseous surgery are contraindicated as a part of preliminary periodontal therapy.19 However, after the initial periodontal therapy, if signs of active periodontal disease or severe pocket probing depths of 5–6 mm or more are still present, flap surgical procedure may be required.20 The presence of significant bone loss and furcation involvement are also the indications for scaling and root planing with periodontal flap surgery. As far as possible, soft tissue periodontal surgical procedures should be scheduled after orthodontic treatment, since these procedures will allow periodontal fibres to get reorganized to the new tooth positions, thereby preventing the relapse.21


Figure 11.7 (A and B) Pretreatment facial features. Straight profile, acute nasiolabial angle, deep mentolabial groove, prominent chin, poor vermilion show and decreased lower facial height. (C–G) Pretreatment intraoral features. Maxillary anterior proclination with spacing, mandibular incisor supraeruption and crowding, periodontitis (severely periodontally compromised dentition), incisor mobility, mutilated teeth and deep overbite (traumatic). (H) Pretreatment radiograph. (I and J) Preliminary periodontal therapy involving thorough scaling and subgingival curettage shows improved tissue response. (K) Endodontic treatment of periapically infected teeth. (L–N) Placement of implants in the region of mandibular right first and second molars. (O and P) Implant–supported metal crowns with orthodontic attachments and compensatory archwire configuration. (Q) Orthodontic treatment to move teeth into areas of better bone support and to correct occlusal problems. (R) Orthodontic treatment progress showing partial attachment gain in the region of mandibular left central incisor, overall improvement in occlusal condition and improvement in the angulation of teeth. (S) Posttreatment occlusion. (T) Bonded flexible spiral wire mandibular retainer.
In addition to establishing the normal health of the periodontium, the goal of the preliminary periodontal therapy is to generate some useful diagnostic information to develop an optimal definitive treatment plan. This information includes the response of the tissues to the initial periodontal therapy, the level of patient compliance, the prognosis of periodontally involved teeth etc. It is focused at nonsurgically controlling the clinical signs and symptoms of inflammation and reducing the pocket probing depth to facilitate orthodontic therapy and later possible bony or soft tissue enhancements. If the patient requires periodontal osseous surgery, it would be appropriate to complete the orthodontic treatment first, establish a stable occlusion, evaluate the periodontal health after 6 months and then decide on definitive periodontal procedures.
After the preliminary periodontal therapy, supportive periodontal treatment that consists of periodontal and dental maintenance is necessary for the success of definitive therapy.22 During the interdisciplinary therapy, it is the responsibility of every specialist involved in the team to monitor the dental and periodontal status at each visit. It is of utmost importance to make sure that the supportive periodontal treatment is strictly instituted during active orthodontic therapy. This is because orthodontic fixed appliances often cause mechanical irritation to the soft tissues and interfere with oral hygiene and with the potential for occlusal trauma due to tooth movement. To prevent caries and periodontal damage, effective and efficient oral hygiene measures should be reinforced during orthodontic therapy.23,24
A typical oral hygiene maintenance protocol during the supportive periodontal treatment should include the use of effective toothbrushing with proper technique, the use of chlorhexidine mouth rinse, the use of fluoride and, above all, the use of plaque-control instructions. It is advisable to recommend the rotary electric toothbrushes since they are more effective in reducing plaque accumulations than manual toothbrushes during orthodontic treatment.25 Accumulation of plaque around the brackets and behind the archwire frequently leads to decalcified enamel white lesions that can be reduced by the prescribed use of fluoride.26 The use of chlorhexidine mouth wash can significantly control the periodontal inflammation.27 While the periodontal control program is being strictly adhered to, the entire dentition should be monitored and evaluated both clinically and radiographically for caries, decalcification, root resorption and endodontic involvement of teeth during orthodontic treatment.
Endodontic treatment
Adult patients undergoing interdisciplinary treatment often present with teeth with pulpal or periapical infections, which may require either endodontic treatment or extraction at some stage during the course of treatment. After thorough scaling and polishing of teeth, all carious lesions should be excavated and restored (Fig 11.7K). However, the deep carious lesions that may be a threat to the pulp should be thoroughly excavated and restored with a temporary sedative filling material. It is important to initiate endodontic treatment of teeth with symptomatic and asymptomatic necrotic pulps in order to control and resolve active pulpal pathology and assess the initial prognosis of the affected teeth.28,29 If the infected tooth cannot be restored and maintained due to its extensive involvement, its extraction should be considered prior to the orthodontic appliance placement. The decision to extract a tooth and its timing should be discussed among the members of the interdisciplinary team, as it affects the treatment plan. As a general rule, it works better for the orthodontist to maintain as many teeth in the dental arch as possible for adequate anchorage.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses