6 Oral Microbiological Changes, Long-Term Enamel Alterations Due to Decalcification, and Caries Prophylactic Aspects
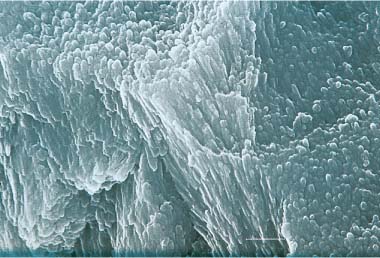
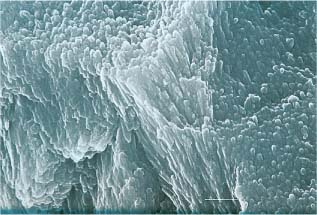
SEM micrograph of an initial caries lesion about 50 μm beneath the surface. Scale bar length = 1 μm
Long-Term Enamel Alterations Due to Decalcification
The Early Enamel Caries Process – the White Spot Lesion
Orthodontic Treatment and Caries Development
Caries-Prophylactic Aspects of Orthodontic Treatment
Importance of Fluoride for Decline of Caries
Cariostatic Mechanism of Fluoride
Rational Caries Prophylactic Measures for Orthodontic Patients
Prevention of Caries Lesion Development during Orthodontic Treatment
Prevention of Caries Lesions Developed during Orthodontic Treatment
Conclusions and Clinical Recommendations
Introduction
Advances in diagnostic methods and treatment techniques during the past decades have provided orthodontists with tools capable of giving their patients improved aesthetic facial appearance, well-functioning occlusion, and knowledge to maintain their dentition in good condition. Modern appliance design and techniques transmit light forces to teeth and the surrounding structures that minimize the potential risk of adverse effects during treatment. Nevertheless, side effects do occur as a result of orthodontic therapy. Some of these effects are caused by the appliance (e.g., caries, gingival inflammation, marginal bone loss, and allergic reactions) and others by the forces applied (e.g., pulp necroses and root resorption). Clearly, it is the responsibility of the orthodontist to be aware of these risks and take precautions to avoid or limit their development.
Enamel decalcification and lesion formation are major clinical problems for patients treated with fixed orthodontic appliances (Fig. 6.1). To be able to diagnose and prevent caries during fixed appliance therapy, the orthodontist must be familiar with all aspects of the caries process and topical fluoride application. The present chapter reviews the most recent findings in caries and fluoride research, and relates these findings to orthodontic treatment with fixed appliances.
Fig. 6.1 Severe decalcifications on the upper anterior teeth after treatment with fixed orthodontic appliances
Oral Microbiological Changes
Individuals with malocclusions often have many retention sites owing to the irregularities of their teeth. More retention sites are introduced when orthodontic appliances are bonded or banded to the teeth. Oral hygiene is thus markedly more difficult to carry out for orthodontic patients than for individuals with normal dentition. Gwinnett and Ceen showed that fixed orthodontic appliances induce a rapid increase in the volume of dental plaque. Chatterjee and Kleinberg subsequently reported that the plaque in orthodontic patients had a resting pH lower than that in nonorthodontic subjects. The plaque-retentive properties of the appliance thus result in a severe cariogenic challenge on the labial surfaces where caries usually does not develop. This may explain the much stronger relationship between oral hygiene and caries incidence in orthodontic patients than in non-treated individuals. The increased amount of plaque in association with orthodontic appliances also rapidly induces gingival inflammation, especially in relation to bands (Fig. 6.2). This gingival inflammation is thought to be due to unspecific bacteria in plaque and is usually reversed after debonding and debanding.
Fig. 6.2 Plaque accumulation and gingivitis in a patient under treatment with fixed orthodontic appliances
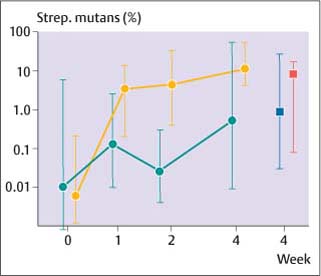
There is a rapid shift in the bacterial flora of plaque after introduction of orthodontic appliances. Unlike gingival inflammation, caries is associated with acidogenic bacteria. Experiments using specially designed orthodontic bands showed an exponential increase in the number of Streptococcus mutans (S. mutans) and lactobacilli in the plaque behind the bands (Fig. 6.3). Scheie and co-workers observed significantly elevated plaque and salivary levels of S. mutans after insertion of orthodontic appliances. Both S. mutans and lactobacilli are often associated with caries development. They are aciduric bacteria and produce organic acids in the presence of fermentable carbohydrates. Sucrose plays a particular role in plaque formation, inducing the formation of a cariogenic plaque. Lactobacilli are generally associated with progression of caries lesions. High levels of S. mutans and lactobacilli in plaque indicate an increased risk of caries. Table 6.1 shows the long-term development of S. mutans (logarithm to base 10 of total numbers) and the percentage of S. mutans in plaque during orthodontic treatment with fixed appliances. The data demonstrate a rapid increase of the total number and the percentage of S. mutans in plaque of orthodontic patients during the entire treatment period, and thus the maintenance of a potentially highly cariogenic environment in the plaque around the appliances. However, the association between caries and bacteria is not a simple one. Several recent studies have shown that prediction of caries development based on bacterial counts is uncertain and of little clinical significance.
Fig. 6.3 Median changes in S. mutans in plaque behind specially designed orthodontic bands (gold circles) and on non-banded surfaces (green circles). Note the logarithmic scale. (Modified from Arneberg et al, 1984)
Arneberg et al studied the pH of plaque in orthodontic patients following a sucrose challenge. By using a microtouch electrode, it was possible to monitor pH changes at different individual sites of the dentition rather than use pooled plaque samples. The lowest pH during resting and fermenting conditions was observed in the plaque of the bonded upper incisors. In these sites, the pH could fall as low as 4. The low pH in the upper anterior region is most likely due to the slow salivary clearance at this location, allowing prolonged retention of acids in the plaque. Interestingly, total plaque fluoride levels were also lowest at these sites, suggesting a direct relationship between plaque pH and total plaque fluoride. It is speculated that the low fluoride concentration in plaque of the bonded anterior teeth is due to increased release of fluoride at low pH.
Eliades et al have studied the wettability and early pellicle formation on different bracket materials, as described in Chapter 1. The bracket materials are discussed at length in Chapter 7. Stainless steel presented the highest critical surface tension, and poly-carbonate and alumina materials the lowest. It was speculated that this could result in reduced plaque-retaining capacity of polycarbonate and alumina brackets relative to stainless steel appliances. Fournier et al reached the opposite conclusion from an in vitro study, where metal brackets presented a lower potential for bacterial accumulation than plastic and ceramic brackets. The presence of saliva, however, lowered the adherence of S. mutans to brackets of all the materials. The clinical significance of these observations is unclear, and additional research under in vivo conditions is necessary.
| Condition Period | log10 S. mutans in Plaquea | Percent S. mutans in Plaque |
| Bonding | 2.4 | 0.1 |
| 12 weeks | 3.5 | 1.5 |
| 24 weeks | 3.8 | 1.1 |
| 72 weeks | 4.1 | 2.0 |
|
Debonding |
4.2 |
1.7 |
Long-Term Enamel Alterations Due to Decalcification
Dental caries involves dissolution of tooth mineral due to organic acids produced by plaque bacteria. To understand the dynamics in the caries process, it is necessary to know the characteristics of sound enamel and the biological and physiochemical events taking place during enamel dissolution. Knowledge about the caries rate in general and for orthodontic patients in particular, and of the mechanism of action of fluoride, is essential to design a caries prophylactic program suitable for the individual orthodontic patient.
Sound Enamel
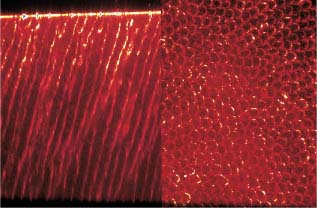
Enamel is characterized by a high mineral content (96 wt%) and by a low content of organic matter (0.4–0.8 wt%) and water (3.2–3.6 wt%). The mineral phase is generally described as calcium hydroxyapatite, which belongs to an isomorphous series of compounds known as apatites. The tightly packed, hexagonal, needle-shaped crystallites of the hydroxyapatite are the real units of enamel and are arranged into prisms. The appearance of the “keyhole”-shaped prisms radiating from the dentin-enamel junction toward the outer surface is due to differences in the orientation of the crystallites (Fig. 6.4). In the inter-prismatic area, the crystallites are more randomly oriented and loosely packed, and consequently this area contains more water and organic matter than within the prisms. Firmly bound water is mainly present as hydration shells around the crystallites.
Fig. 6.4 Confocal laser scanning microscopic image of sound enamel. The interprismatic enamel appears as light colors, and the prism centers as dark colors. Note the typical keyhole or honeycomb structure of the prisms. Left: Optical section perpendicular to the surface. Right: Optical section parallel to the surface. (Courtesy of Professor Heinz Duschner, University of Mainz, Germany)
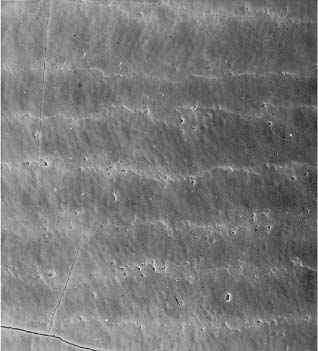
Fig. 6.5 Scanning electron microscope (SEM) micro-graph of sound enamel from a newly erupted premolar. Note the typical perikymata pattern
The enamel is extremely heterogeneous from a chemical point of view, and it has been shown that a large number of impurities are present in enamel, particularly in the caries-susceptible areas. Sodium, carbonate, and fluoride ions may exchange for calcium, phosphate, and hydroxyl ions, respectively. The apatite in enamel is non-stoichiometric, probably owing to calcium deficiencies and the presence of the sodium and carbonate ions. More carbonate ions are found in deciduous enamel than in permanent enamel, which may be one factor why lesion progression in deciduous enamel is faster than in permanent enamel. Surface enamel is harder, and tends to have higher mineral content and lower water content than subsurface enamel. In addition, several ionic species with high affinity for the mineral phase (e.g., fluoride, zinc and lead) are present in higher concentration in surface enamel.
Fig. 6.6 Initial caries development along the perikymata lines. Note the opening of the prism endings. Scale bar length = 20 μm. (From Arends et al, 1987)
In the scanning electron microscope (SEM), surface enamel exhibits large variation, probably due to age and site in the oral cavity. Macroscopically, and in the SEM, surface enamel of newly erupted teeth exhibits the so-called perikymata or imbrication lines (Fig. 6.5). It has been found that perikymata geometrically represent closed circles. Subsequent to tooth eruption, the perikymata are progressively worn away over the years as a result of normal function and toothbrushing. Perikymata are thus rare in adults. Also, the bonding and de-bonding procedures of orthodontic brackets contribute to loss of the perikymata. Studies using orthodontic bands to induce plaque on premolars to be extracted for orthodontic treatment have shown that the initial caries process starts along the perikymata lines by exposing the prism endings (Fig. 6.6) and then progressing along the interprismatic areas (Fig. 6.7).
Fig. 6.7 SEM micrograph of an initial caries lesion about 50 μm beneath the surface. Note the increased porosity along the interprismatic areas and the dissolution of single crystals. Scale bar length = 1 μm. (From Arends et al, 1987)
The Early Enamel Caries Process – the White Spot Lesion
It is the tight packing of the crystals that makes enamel translucent. Increase in the porosity of the enamel leads to changes in the optical properties, as light is scattered. The white appearance of early caries lesions is thus an optical phenomenon. The whiteness increases when the white spots are dried by air, since water is replaced by air, and air has a lower refractive index than hydroxyapatite and water. The lesion area is slightly softer than the surrounding sound enamel.
Fig. 6.8 Schematic drawing of the three types of lesions that may develop in enamel depending on the pH in plaque fluid: A, subsurface lesion; B, surface softened lesion; C, erosion. (SL = surface layer; L = lesion body; SO = surface softening)
Three types of enamel lesions may develop, depending upon pH and fluoride concentration in the plaque fluid (Fig. 6.8). When pH drops below the critical pH of enamel (~ 5.5), plaque fluid becomes undersaturated with respect to hydroxyapatite, and the enamel starts to dissolve. Using orthodontic bands on a pair of premolars to be extracted as part of fixed appliance therapy, it was possible to monitor the caries process from week to week. Clearly, the initial enamel lesion causes softening of the surface. This softening is characterized by a gradual decrease of the mineral content in the surface enamel, caused by preferential dissolution of interprismatic mineral. On microradiographs, these lesions lack a surface layer. The typical subsurface lesion with a porous surface layer is formed later in the caries process and requires that plaque fluid becomes supersaturated with respect to fluorapatite. Thus, in the presence of fluoride, the critical pH of enamel is lowered from 5.5. to 4.5. When the pH of plaque fluid is lower than ~ 4.5, plaque is still undersatu-rated with respect to hydroxyapatite and also to fluorapatite, and an erosion is formed. This is also where there is a limitation for the cario-static effect of fluoride (see below).
The General Caries Situation
During recent decades, the prevalence of dental caries in school children has decreased by more than 70% in Western Europe and in the United States. In the United States and the Nordic countries, 50% of 12-year-old and more than 70% of the 5-year-old children are caries-free. Very few 18 to 19-year-old adults are caries-free, but the average DMFT (decayed/missing/filled teeth) index is less than 6, with mainly posterior lesions and fillings. In those countries where caries has declined, it is interesting to note that not only has the prevalence of caries changed but also the distribution of lesions in the dentition; lesions on smooth surfaces occur less often. Caries is increasingly becoming a pit and fissure phenomenon. Furthermore, already established lesions progress more slowly than earlier.
It is important to note that caries is not a disease limited to children. As many as 95% of adults have experienced caries, showing that people are at risk of caries throughout life. In Eastern Europe dental caries is still a significant problem, and caries prevalence is reported to increase in some developing countries, presumably owing to increased sucrose consumption.
Average data do not necessarily give a true picture of the caries distribution in the population. While almost all individuals had a high caries rate in the past, in some countries 20% of the 12-year-olds now account for 80% of all clinical caries lesions. In the Nordic countries, only those lesions that require restorative therapy are formally recorded as caries; i.e., the DMFT/S indices are mainly applicable to caries that has progressed into dentin. A significant number of initial enamel lesions in the proximal surfaces have been observed in 18-year-olds, but these are not included in the statistics. It has been speculated that these lesions may in time develop into dentinal lesions. In this way the actual caries prevalence in the population could be masked, and a more favorable picture would be presented than was justified. However, cross-sectional studies in 35-year-olds in Oslo in 1973, 1984, and 1993 have clearly shown a reduced caries prevalence in the adult population, also. The caries reduction observed among children and adolescents thus seems to be maintained as a permanent reduction in caries prevalence into adulthood.
Orthodontic Treatment and Caries Development
Orthodontic treatment is generally carried out during childhood and adolescence. This is a period when caries incidence is relatively high. Because of visual obstruction by the appliance, development and progression of lesions in the proximal surfaces may be difficult to diagnose. Bands protect the proximal surfaces (Fig. 6.9). The appliance may also make X-ray examination more difficult.
A number of studies have investigated the relationship between orthodontic treatment with fixed appliances and caries development. Some previous studies showed increased caries frequency in subjects receiving orthodontic treatment, whereas more recent investigations did not confirm such correlation. Zachrisson and Zachrisson reported that orthodontic treatment with banded appliances did not increase the prevalence of dental caries. However, in orthodontically treated individuals, they observed a shift in the distribution of lesions from posterior to anterior teeth and from inter-proximal to facial/lingual surfaces. The bands obviously protected the proximal surfaces from dissolution. The gap between the band and the gingival margin on the labial surface of the anterior teeth, on the other hand, resulted in plaque accumulation and the development of lesions.
Fig. 6.9 Large caries lesion on upper first molar detectable only after debanding. Note that the archwire in the lower dentition masks the proximal surfaces
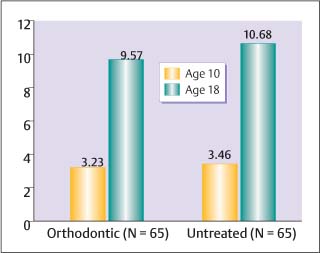
During recent decades, along with the marked decline in caries in the population, orthodontic treatment techniques have changed from banded to mainly bonded appliances. Today bands are used mainly on the molars. The protection given by bands on proximal surfaces of the incisors and premolars is no longer present. The incidence of filled teeth from 10 to 18 years of age has been evaluated in individuals treated with mainly bonded orthodontic appliances. The mean age at the start of treatment was 12 years, and the mean treatment time was two years. A group who had not received orthodontic treatment served as the control. The study showed no significant differences in filled surfaces between the orthodontic group and the untreated group at the age of 10 years, approximately two years prior to treatment, and no significant difference several years after treatment at the age of 18 years (Fig. 6.10).
Fig. 6.10 Mean number of filled surfaces (FS) at the ages of 10 and 18 in orthodontically treated patients and non-treated individuals. (From Øgaard, 1989a)
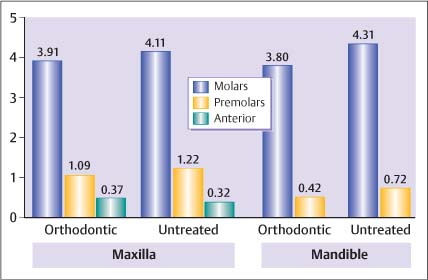
Fig. 6.11 Distribution of restorations in molars, premolars and anterior teeth at the age of 18 in orthodontically treated and non-treated individuals. (From Øgaard, 1989a)
The distribution of restorations in the dentition did not show any significant difference at the age of 18 years (Fig. 6.11). It has been argued that a substantial number of incipient enamel lesions could have formed during orthodontic treatment and that these subsequently become deep lesions after treatment was concluded. However, this study recorded filled surfaces about five years after treatment, which is probably more than the average time for progression of caries in the enamel. From the previous discussion, it seems that a caries lesion developed during orthodontic treatment would be restricted to the outer enamel surface and would not necessarily progress when fluoride toothpaste was used regularly.
Fig. 6.12 Severe white spot lesions developed along the gingival margin during treatment with fixed orthodontic appliances
Several reports have shown an increased incidence of early enamel caries (white spot lesions) on the labial enamel surface during orthodontic treatment (Figure 6.12). These white spot lesions rarely progress into becoming significant cavities and are generally not registered as caries requiring filling therapy in the DMFT/S indices. Gorelick and co-workers observed that as many as 50% of subjects experienced an increase in the number of white spot lesions with fixed orthodontic appliances when no preventive fluoride programs were used. Usually the first molars and upper lateral incisors are most affected (Fig. 6.13). Even with regular use of a fluoride dentifrice, enamel dissolution may occur around orthodontic brackets. Using specially designed orthodontic bands, visible white spot lesions could be induced within four weeks, i.e., within the period between one clinical appointment and the next Initial caries developed in the cariogenic environment of an orthodontic appli/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses