Maxillary sinus grafting
![]() Additional illustrations can be found on the companion website at www.blockdentalimplantsurgery.com
Additional illustrations can be found on the companion website at www.blockdentalimplantsurgery.com
Background, general principles, and techniques
Bone availability is the key to successful placement of endosseous implants in the posterior maxilla. When the thickness of the bone between the maxillary sinus and the alveolar crest is less than 9 mm, increasing the thickness of the alveolar sinus floor by bone grafting is one option that will support implants and prosthetic restoration. The graft material chosen must provide adequate viable bone to stabilize the implant initially and encourage osseointegration. Materials used for sinus floor grafting include autogenous bone, allogeneic bone, sintered xenograft, and recombinant bone morphogenetic protein (BMP).1
Long-term assessment of the amount of grafted bone in the sinus, remaining adjacent to implants placed into the grafts, has been reported within case reports, small case series, and limited retrospective reports.2–24 One report examined the use of tomography to assess the bone level relative to the apical portion of the implant and the height of alveolar ridge.25 This report indicated that after 5 to 10 years of function, bone formed in autogenous bone–grafted sinuses, was retained; this was confirmed by others.25–33 The population in this study had simultaneous placement of hydroxylapatite (HA)–coated implants (e.g., cylinders, screw shapes) with autogenous bone grafts. After 5 to 10 years of function, bone was present. A total of 90% had bone covering the apical portion of the implant. This study supports the use of autogenous bone for sinus grafting. The techniques described in this chapter are similar to those mentioned in the long-term tomography study.25
In the tomography study, no attempt was made to differentiate prosthesis design, length and diameter of implants, or small variations in surgical technique (e.g., antibiotic coverage, flap design, type of implants used). Nevertheless, failure of the implants and grafts was rare. The prostheses fabricated for these patients followed well-known techniques. The effects of specific prostheses on graft maintenance and implant survival were not evaluated.25
Combinations of bone materials have been suggested to lower the necessary volume of harvested autogenous bone and to extend the graft’s volume. The addition of demineralized, freeze-dried bone (DFDB) to iliac cancellous bone grafts slightly lowered the eventual bone level.25 Although this difference was statistically significant compared with autogenous bone alone, the clinical difference was small because the implants were still covered with bone. In some clinical situations, the amount of bone harvested from the donor site is less than required. In these cases, DFDB was added to increase the volume of the graft. The addition of DFDB did not increase the eventual graft volume over the long term.
An autogenous cancellous bone graft contains endosteal osteoblasts that can survive the transplantation process when handled appropriately, and this graft subsequently forms bone.34–37 A corticocancellous block graft provides transplanted osteoblasts and growth factors, as well as structural rigidity, which frequently is required when implants are placed simultaneously.38 However, the cortical portion of the graft is slow to revascularize. The structural rigidity of the graft allows accurate implant placement independent of the thickness of the sinus floor. The healing of these bone grafts follows a course that starts with basic wound healing and proceeds with bone remodeling.39–42
What alternatives might be used instead of autogenous bone and demineralized bone? Evidence-based clinical data supports the use of sintered xenograft (bovine or equine) combined with autogenous bone or used by itself to induce or conduct bone formation within the graft and support implants.43–45 To control the graft’s position and decrease particle migration, fibrin glue can be added to create cohesion of the composite graft particles, which limits their migration after placement of the graft in the sinus. Another alternative for the primary graft material is the use of BMP.46,47 BMP can be placed within the sinus under an elevated membrane and forms bone within the sinus without the use of other materials. Recombinant BMP is expensive and when used by itself can result in increased swelling in the patient. To decrease the amount or dose of BMP used and to decrease cost to the patient, BMP has been combined with mineralized bone allograft. Long-term evidence-based clinical data on the incidence of bone formation in the sinus have been minimally reported. It is expected that other combinations of materials that promote bone formation with the use of a scaffold will prove effective at solving the problem of vertical height deficiency in the future.48–55
In the past, the amount of bone available on the alveolar crest dictated the source of bone graft material, whether it was an autogenous block or particulate cancellous bone, and whether implants were placed simultaneously or delayed regarding graft placement. Clinical evidence indicates that less morbid alternatives are bioequivalent to autogenous bone with less morbidity and less need for general anesthetics for bone harvesting.56,57
The consensus conference sponsored by the Academy of Osseointegration57 and other studies indicate that xenografts used by themselves or combined with autogenous bone worked as well as autogenous bone alone.44 Demineralized bone alone did not result in predictable bone formation. This opened the spectrum of using a less morbid approach by avoiding hip or tibia bone harvesting to grow bone within the sinus to support dental implants.
The clinical use of iliac crest or tibia cancellous bone harvesting has decreased and has been substituted by the use of BMP with mineralized bone allograft, BMP used alone or xenografts with or without the addition of autogenous bone, fibrin glue, or both. There is excellent evidence for the use of BMP alone or xenograft with autogenous bone or with a fibrin glue cohesive product. Clinical data are limited using the combination of BMP and allograft. However, its use in cervical spine fusion and in basic science publications indicates that the combination of BMP and mineralized bone is an obvious choice.58
Early clinical data and animal studies indicate that sintered xenograft and nonresorbable alloplastic materials do not allow for bone formation in the scaffolds compared with mineralized bone. 58,59 When recombinant human BMP (rhBMP) is combined with sintered xenograft, there is a negative effect on bone formation in the maxillary sinus. This may be the result of more scar formation and less vascular infiltration for cellular recruitment in the graft.59 There is less bone formation using demineralized bone with BMP than when BMP is used alone.60 rhBMP has been used with mineralized bone allograft for continuity repair on the mandible.61 When used alone in the sinus, rhBMP forms bone that is adequate for implant placement and function.62
Presurgical screening
Exclusion criteria that should be considered include the following:
1. Smoking. Cessation of smoking must occur a minimum of 4 weeks before sinus surgery and continue until bone has formed and matured.
2. Uncontrolled systemic diseases. Patients with uncontrolled diabetes or other uncontrolled systemic diseases involving bleeding or the immune system are not candidates for the procedure. Bone formation in patients with diabetes with blood sugar levels that fluctuate over 120 mg/dL during the day heal adversely compared with those with well-controlled diabetes.
3. Active pathologic conditions. Endoscopic sinus surgery may be necessary to remove polyps, mucocoeles, or purulent exudate. If the patient maintains a healthy sinus after removal, sinus graft surgery can be performed.
4. Excessive nasal pathologic conditions. Conditions that obturate the drainage os of the maxillary sinus may require intranasal surgery before the sinus graft procedure.
5. Radiation therapy. Patients with a history of radiation therapy to the maxilla are not candidates for routine sinus augmentation procedures.
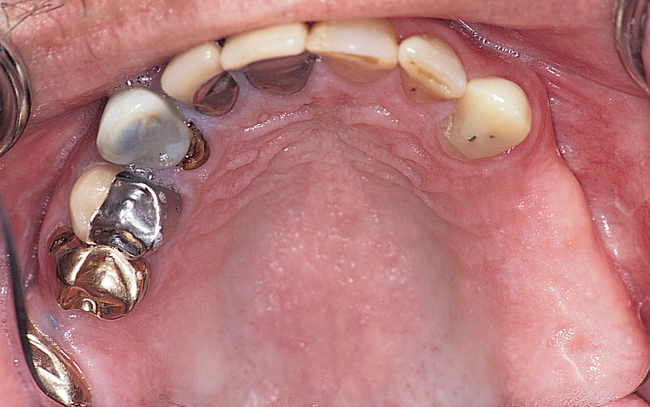
6. Adjacent dental disease needs to be corrected with endodontic therapy, periodontal therapy, or tooth removal before sinus augmentation.
Preoperative radiographic screening
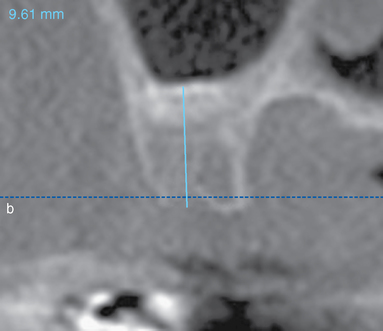
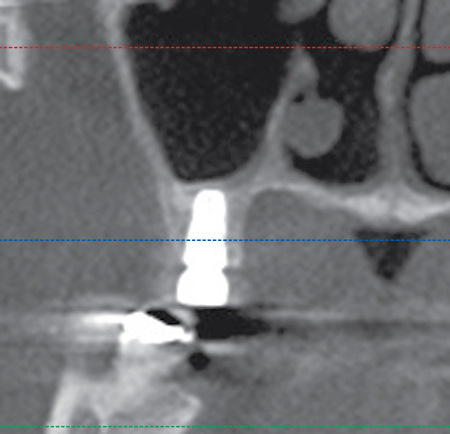
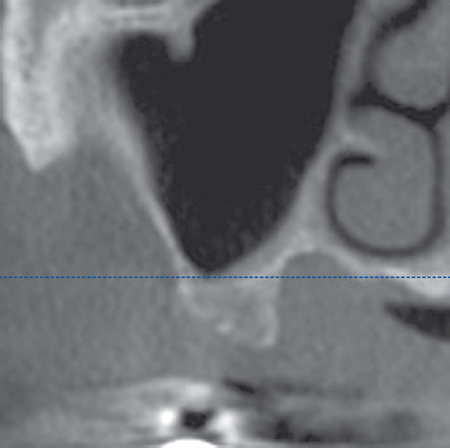
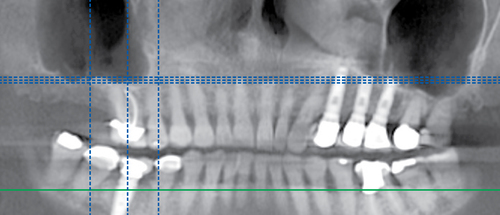
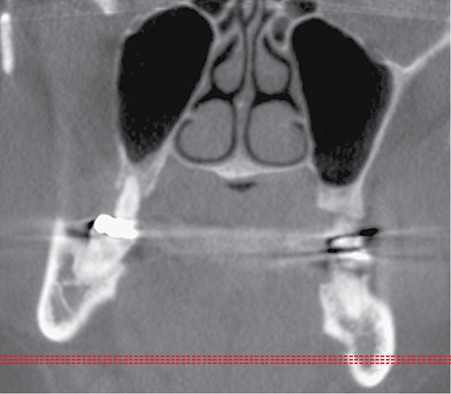
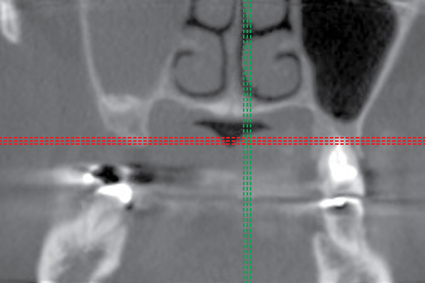
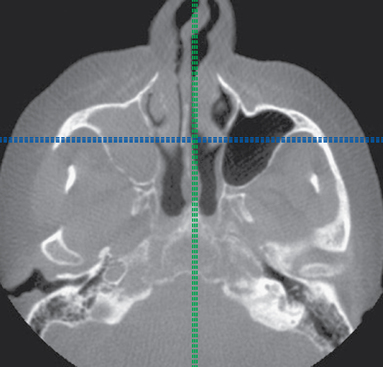
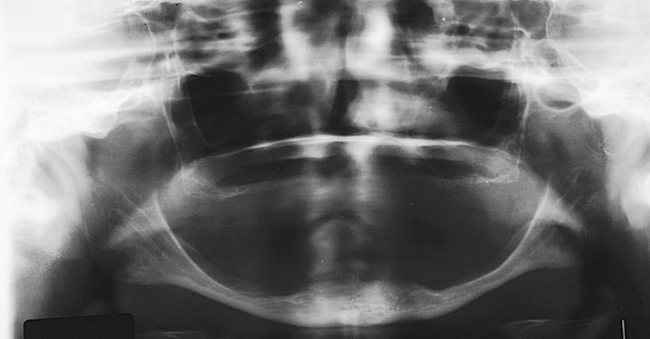
The clarity of the maxillary sinus, the presence of septa in the proposed surgical site, and an approximation of the thickness of the alveolar bone are visualized. Some patients have large aerated sinuses. Some patients have smaller sinus cavities with the lateral nasal wall more laterally positioned than others. Some of these sites have a well-defined concave site with the surrounding walls creating a well-defined space for an anatomically driven graft. Periapical radiographs do not usually contribute to the screening of the patient for sinus grafts. Therefore, a cone-beam scan is absolutely indicated for patients who are candidates for implants in the posterior maxilla (Figure 6-1). These observations help determine the ideal material for each patient.
Anatomic considerations for material and method for sinus augmentation
1. Bone thickness. Two approaches are generally considered for sinus floor augmentation. One includes development of a lateral window with elevation of the sinus membrane along the floor and medial wall. The second is sinus floor elevation through the alveolar crest during implant site preparation.
When removing a posterior maxillary tooth, alveolar bone height can be developed in two stages using intrasocket osteotomies to elevate the sinus floor. When a posterior maxillary tooth is to be removed and there is less than 7 mm of residual bone available at the time of tooth removal, the bone within the socket can elevated 3 to 4 mm to increase the alveolar height close to 7 or 8 mm.63 Implant placement, after the bone has formed within the extraction socket, is performed usually 4 months after tooth removal. If needed, additional bone height is developed by osteotome methods through the implant site, which avoids a lateral window approach. This is discussed later in this chapter.
2. Presence of tooth roots along the sinus floor or septi. Sinus membrane elevation through a lateral window has the potential complication of perforation. Recent presentations by multiple clinicians vary in their perforation rate, but all agree that if there is a perforation, the patient has a greater chance for poorer bone formation and sinusitis due to migration of graft material. The cone-beam scan allows the surgeon to see the intimate relationship of the tooth roots to the sinus floor. Often these teeth are removed and the sockets grafted before the sinus augmentation because of infection of these teeth. The question is how long the surgeon should wait before elevation of the sinus membrane for augmentation. The membrane seems to become “glued” to the previous root site and may have bone irregularities around it. These sites are often potential perforation locations. When this is anticipated, the use of rhBMP with allograft is chosen to avoid particle migration into the sinus. A piece of rhBMP-impregnated collagen can be placed against the perforation when performing the augmentation. Another option is a sheet of collagen. It is unclear if a short-or long-lasting collagen sheet or membrane is optimal.
Surgical technique
Lateral window approach
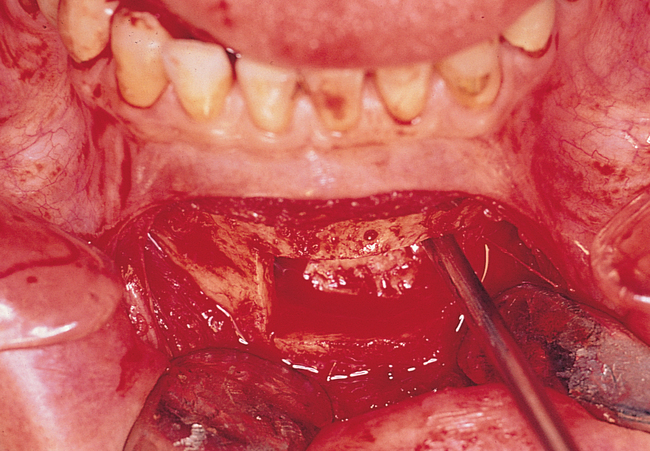
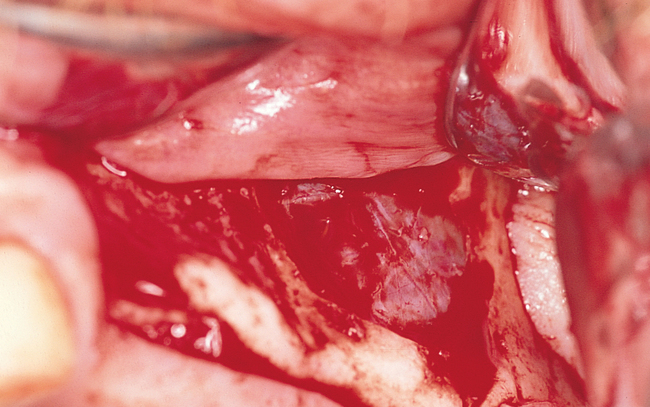
The inferior horizontal ostectomy should be made as close to the floor of the sinus as possible to facilitate membrane dissection. The vertical ostectomies should be made close to the maxillary buttress and lateral nasal wall, again to facilitate membrane elevation (Figure 6-2). The superior horizontal cut should be made at the level of the planned augmentation height, which should allow placement of implants at least 11 mm long. After the window has been created, the lateral bone still adherent to the sinus membrane can be either rotated medially (see Figure 6-2) or removed.
After the periosteum has been reflected superiorly, exposing the lateral wall of the maxilla, the planned ostectomy is visualized to start at the level of the maxillary sinus floor. The vertical osteotomies are parallel to both the lateral nasal wall and the anterior border of the maxillary tuberosity, where the maxilla curves posteriorly. The superior horizontal ostectomy is located where the vertical position of the augmentation is planned. A light source can be placed toward the palate without touching the tissues to avoid heat damage, and the lighting is decreased. The light will transilluminate the sinus, and the walls of the sinus can be identified. A sterile pencil is used to mark the bone as an outline of where to make the ostectomies close to the borders of the sinus (Figure 6-3).

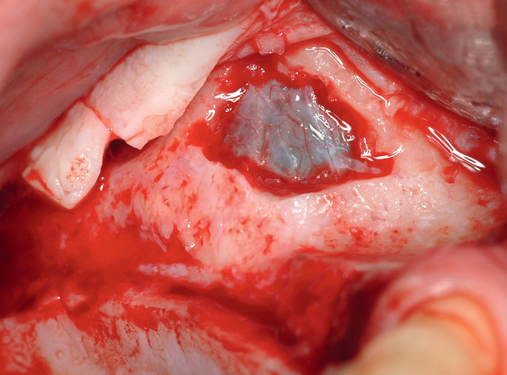
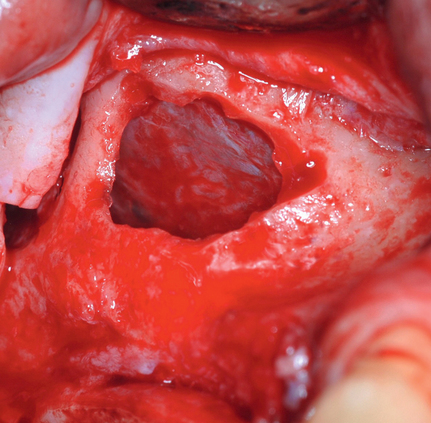



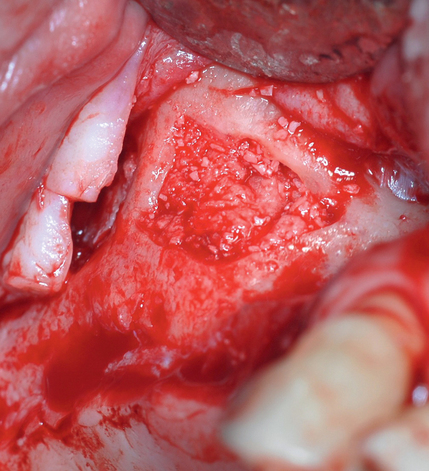
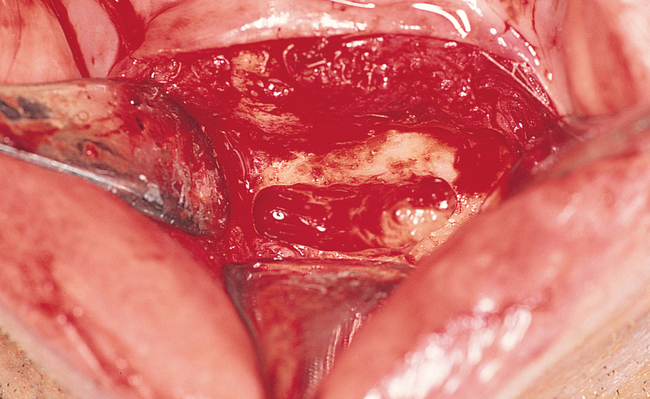
A round bur with irrigation is used to remove cortical bone and expose the gray, glistening sinus membrane (see Figure 6-2). The lateral maxillary wall can be left intact and rotated inward as the new floor of the maxillary sinus, or it can be removed, depending on the clinician’s preference. A smooth, relatively new elevator is used to peel the sinus membrane from the floor of the maxillary sinus and lateral nasal wall (see Figure 6-2). The membrane is elevated to the height of the desired augmentation. The edges of the sinus membrane are elevated initially, gradually increasing the distance of membrane elevation. Excessive elevation of one isolated portion of the membrane is avoided because this would result in tension on the nonelevated membrane. The membrane must be sufficiently elevated to avoid excessive pressure when the sinus graft material is placed.
Perforations of the sinus membrane may occur, depending on the experience of the operator, location of the horizontal ostectomy, presence of septa, and thickness of the sinus membrane (see Figure 6-2). Small perforations are left untreated. If large perforations are present, the procedure is aborted and attempted at a minimum of 4 months later. Use of a patch, such as a collagen membrane or other resorbable membrane, is at the discretion of the operator, with the understanding that the addition of such materials may increase the chances of postoperative infection. If solid blocks of bone are to be used, an intact sinus membrane may be less important. After the membrane has been elevated, the bone harvest procedure is performed.
Bone-harvesting techniques
Autogenous intraoral grafts
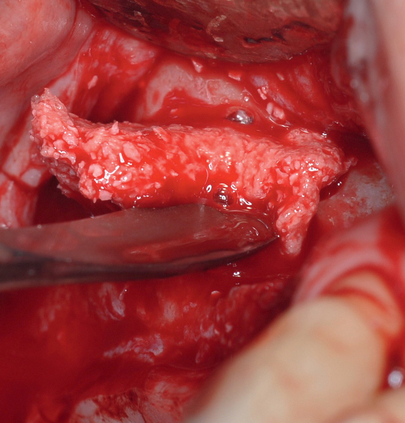
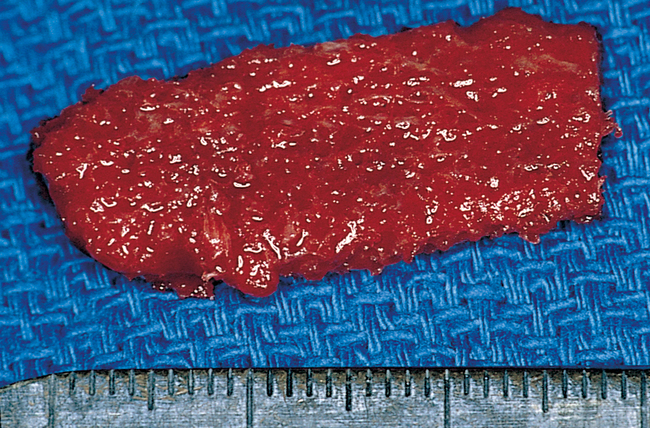
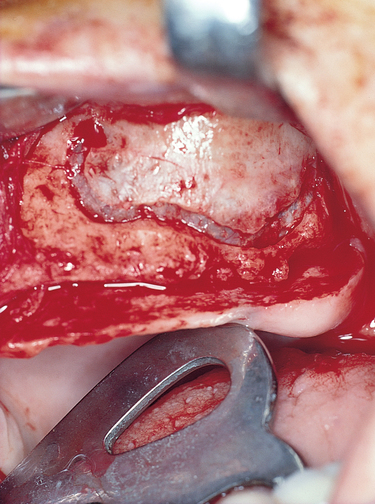
For a patient undergoing unilateral sinus graft surgery, with the plan to combine autogenous bone with sintered xenograft, the surgeon usually can harvest the needed bone from the posterior maxilla, the mandibular third molar site, or the chin to obtain sufficient autogenous bone, mixed with an equal amount of sintered xenograft, to augment one sinus (Figure 6-4).

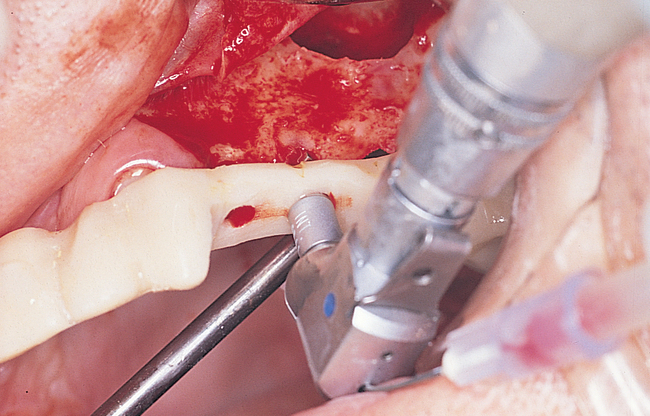
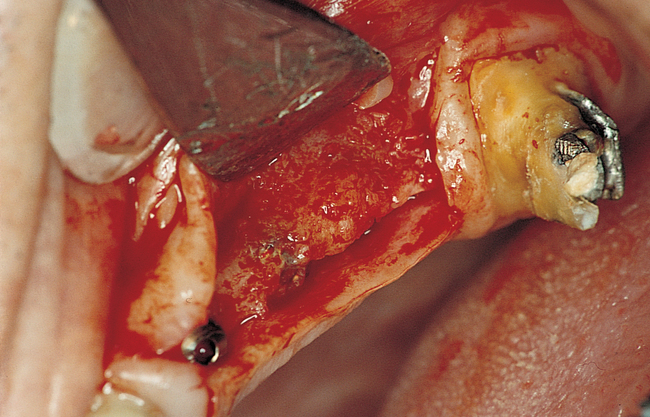
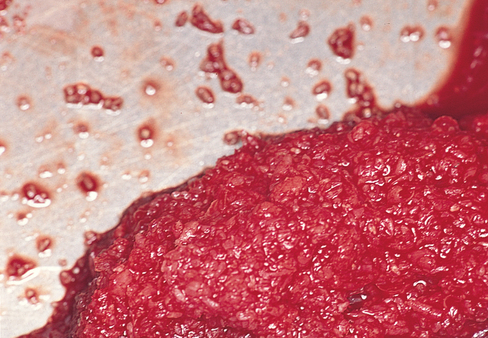
Another intraoral option is to use a scraping device on the mandibular third molar ramus site to harvest cortical bone and a small amount of cancellous bone (Figure 6-5). The cortical portion of the mandible has very few viable osteoblasts. If is now rare to use the chin to harvest bone for sinus augmentation, with the modern advent of using rhBMP or sintered xenograft combined with smaller volumes of autogenous bone.
Iliac crest grafts
Multiple approaches can be used to reach and harvest bone from the iliac crest. For sinus grafting, the anterior approach usually is performed because it does not require turning the patient after the sinus elevation has been completed. In addition, a satisfactory amount of bone usually can be harvested from the anterior approach. To limit blood loss and minimize gait disturbances, the technique most often used involves a relatively avascular approach, with great care taken to avoid the sensory nerves that traverse the iliac crest region. After a sterile preparation and draping of the anterior iliac crest, a local anesthetic is administered. Blunt dissection with hemostatic control using electrocautery is used to approach the anterior iliac crest. The approach should be performed from the lateral anterior aspect to prevent reflection of the insertion of the tensor fasciae latae muscle, which will minimize long-term gait disturbances. The muscles are separated rather than incised, with the dissection medial to the gluteus medius muscle and lateral to the iliacus muscle. In the area of the iliac tubercle, fibers from the external oblique and other muscles may need to be elevated when large pieces of bone are harvested, but these fibers should be left intact if possible. The sensory nerves usually pass over the anterior and posterior spines and are encountered in fewer than 2% of patients. Usually they can be retracted, and sensory loss thus is a rare complication from iliac crest bone harvest.64
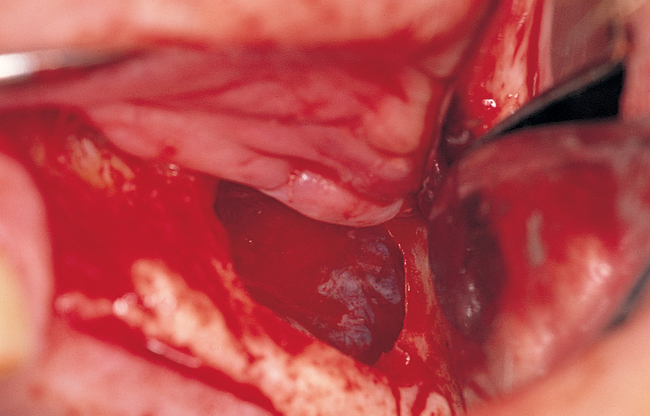
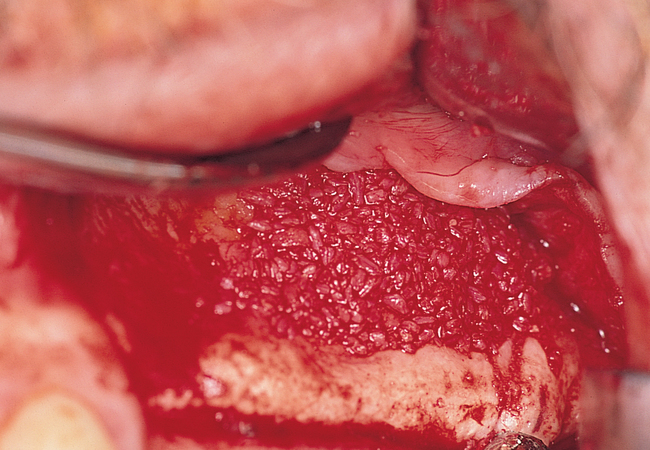
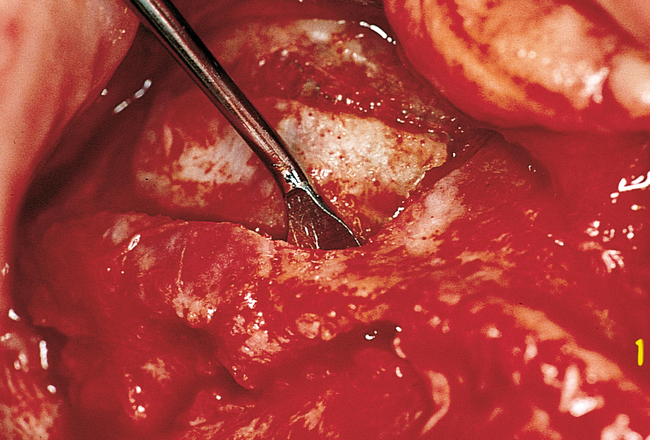
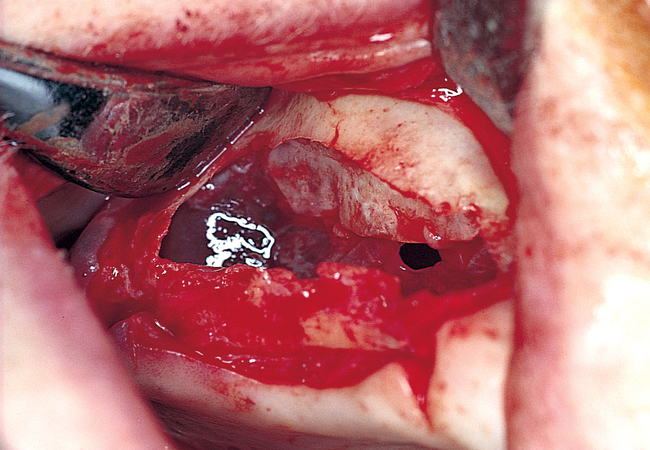
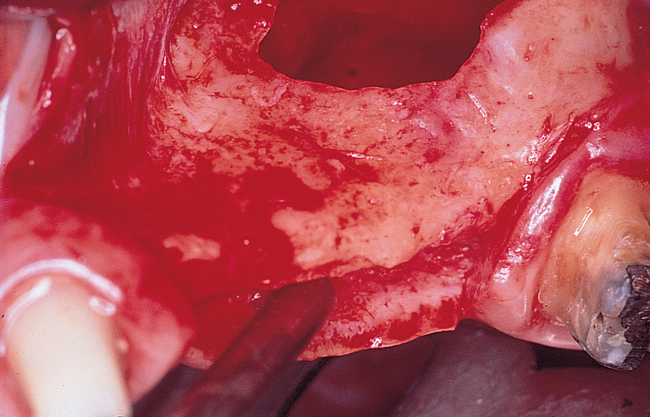
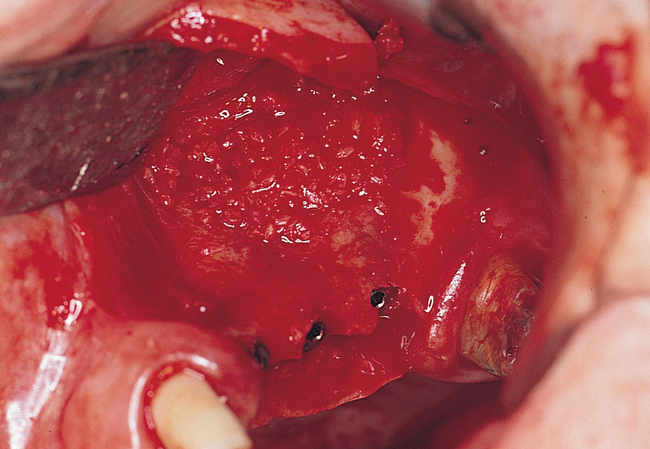
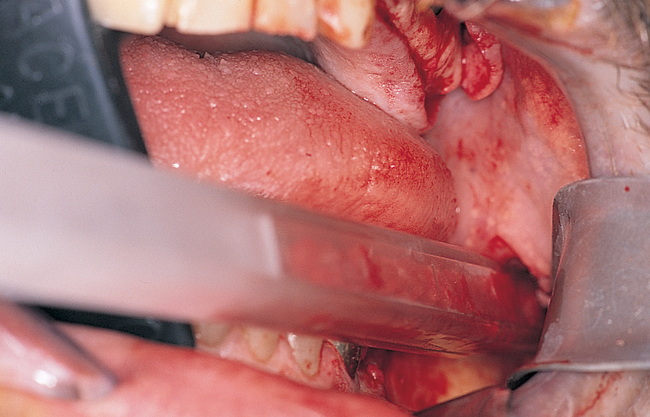
For the harvesting of blocks of corticocancellous bone, either the lateral or the medial cortical plates of the iliac bone are stripped of periosteum (Figures 6-6 and 6-7). A saw with copious irrigation or sharp osteotomes are used to outline and remove a piece of bone. Additional cancellous bone can then be collected, after which the wound is closed in layers.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses