Surgery of the partially edentulous maxilla
![]() Additional illustrations can be found on the companion website at www.blockdentalimplantsurgery.com
Additional illustrations can be found on the companion website at www.blockdentalimplantsurgery.com
Surgery of the anterior maxilla for the partially edentulous patient
Anterior maxilla multiunit restorations: Preoperative planning and assessment
Implant-supported therapy for a patient missing or who will be losing anterior maxillary teeth requires the same attention to general considerations as described in Chapter 3. The goals of the patient will usually be restoration of a functional occlusion in an esthetic manner.
Placement of implants and onlay bone grafts for isolated defects
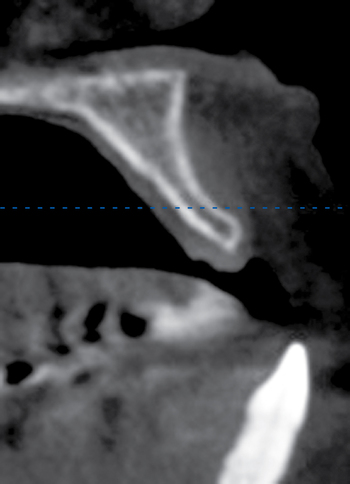
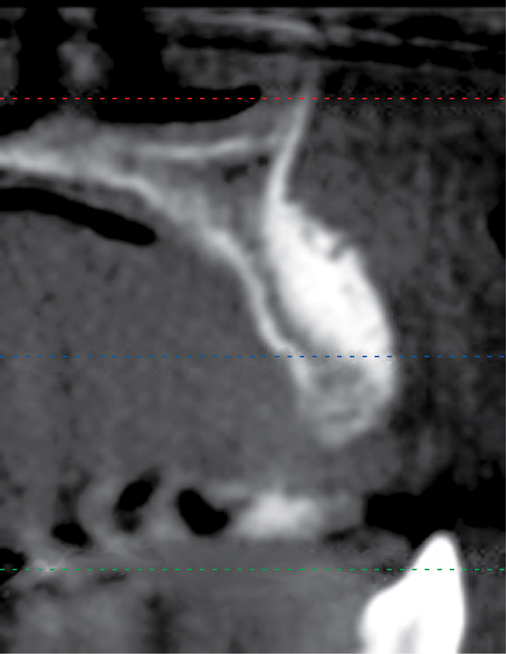
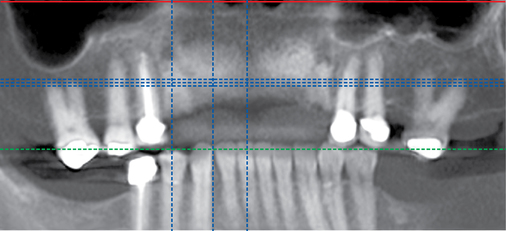
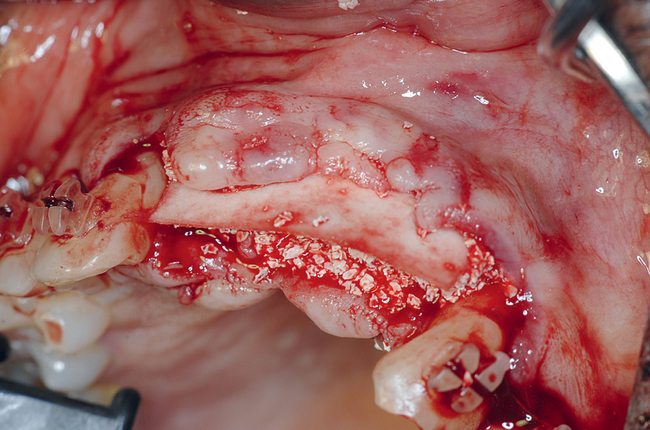
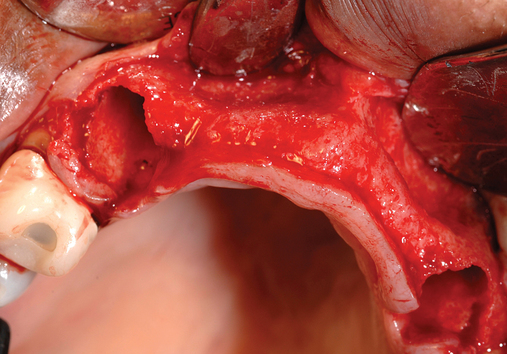
Patients with isolated bone defects caused by trauma or ablative tumor surgery who have retained a portion of the dentition often seek treatment for these defects. The missing bone results in a functional defect that is not amenable to placement of conventional removable prostheses. For these patients, the history of the problem and accurate treatment planning aid in the choice of a design that likely will include bone grafting and placement of implants to assist in prosthesis retention (Figure 4-1). Important information from the patient’s history includes smoking habits, radiation therapy, recurrent infection and scar formation, and malnutrition or other systemic factors that can affect wound healing.
Augmentation of the anterior maxilla using particulate graft material combined with fibrin glue and resorbable membrane





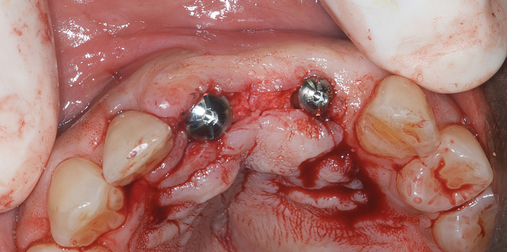

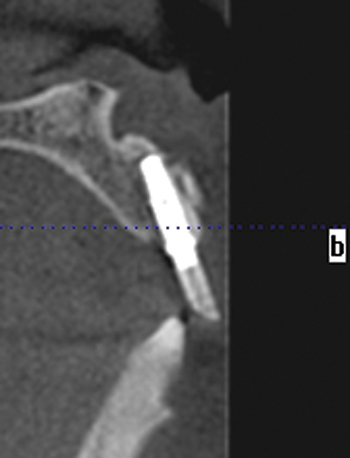
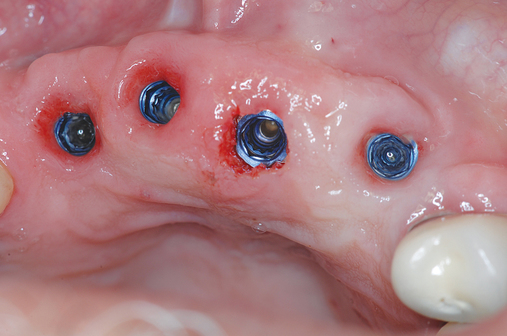
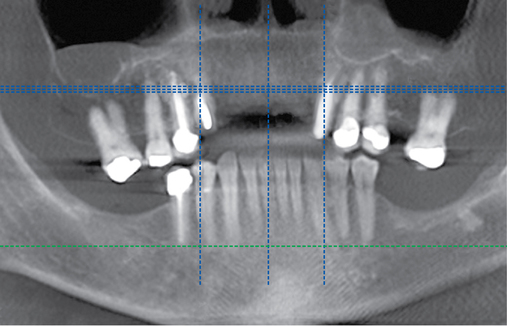
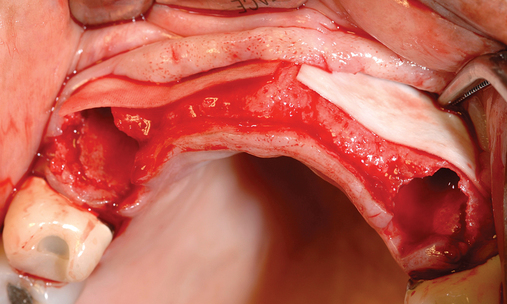
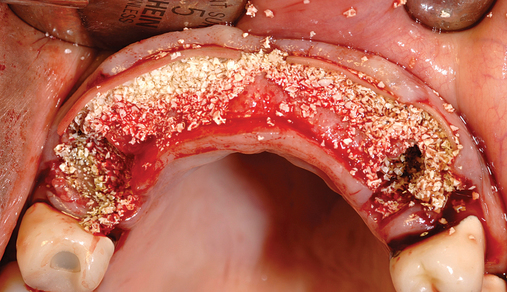
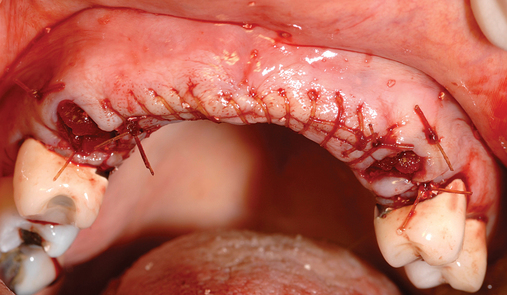
The patient had lost three anterior maxillary teeth. Diagnostic models showed that orthodontic treatment was indicated to realign the teeth that had been moved during healing of the patient’s complex alveolar fractures. After orthodontic realignment of the teeth, the extent of the necessary horizontal ridge augmentation was defined (see Figure 4-1). The treatment plan called for horizontal ridge augmentation and, after graft healing, the placement of implants for a three-unit, implant-borne restoration.
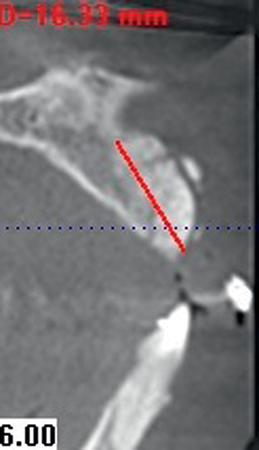
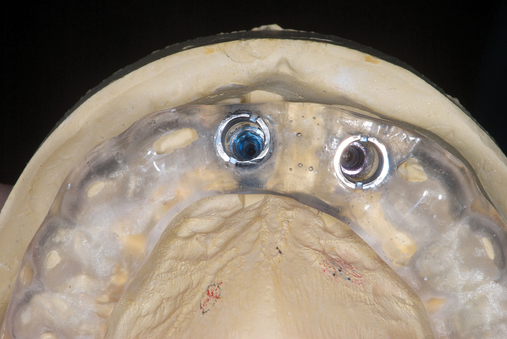
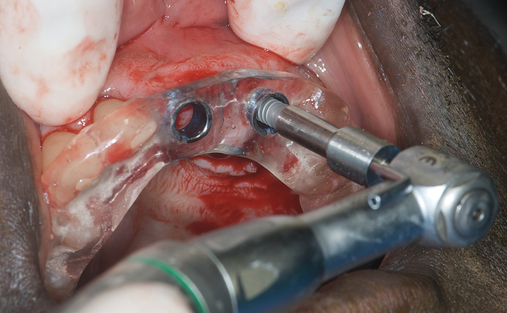
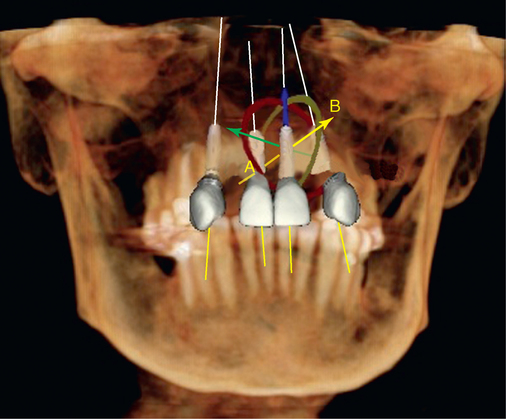
After the augmentation form and position were confirmed, a new ideal tooth setup was done, identifying the final implant positions. A model had implant analogs placed into a diagnostic model, and small radiopaque markers were placed into a guide stent. A new CT scan was taken to confirm that the implants could be positioned into bone as planned, using the small pins to evaluate angulation of the implants. The position was confirmed, and a model-based CT guide stent was made. The implants were positioned with their entry into bone confirmed by a small palatal flap for direct visualization. Healing abutments were placed. After 4 months, the final restoration was made. The augmentation using bovine particulate under a resorbable membrane resulted in thick, healthy gingiva that was easily formed by the restoration, without recession (see Figure 4-1).
Horizontal grafting the thin ridge at the time of tooth removal for restoration of anterior six maxillary teeth
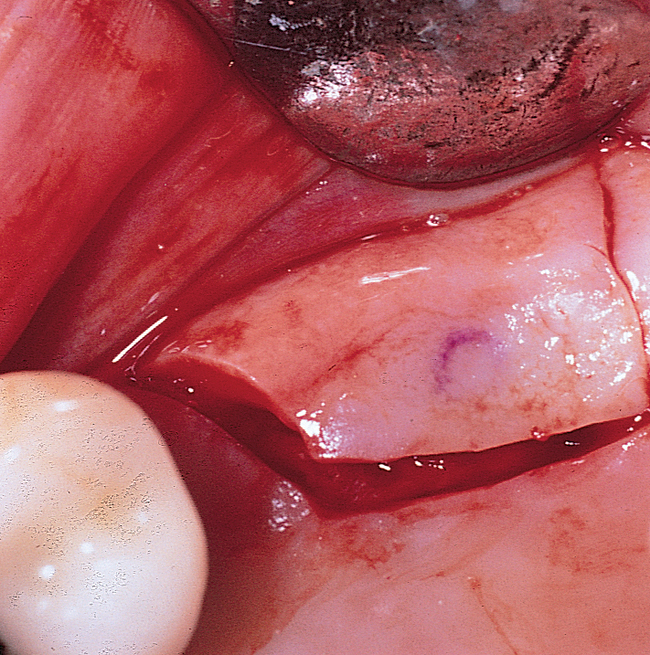
Several patients have long-span bridges in the anterior maxilla. Because of trauma from occlusion from lack of adequate posterior occlusal balance, the anterior bridges fail with accompanying tooth fractures. This patient (Figure 4-2) demonstrates the common dilemma of two canines in need of removal with the added need for mechanical bolstering from implant placement in the central incisor locations to avoid a similar problem from lack of a tripod mechanical situation.




Surgery for the posterior maxilla
Single-premolar or single-molar restorations
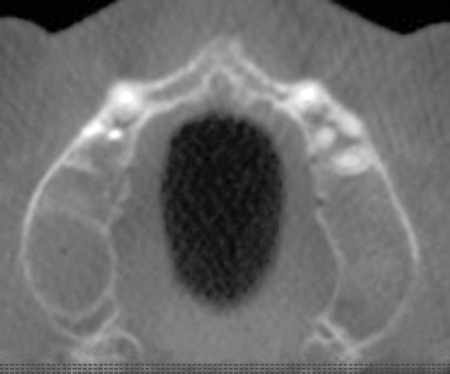
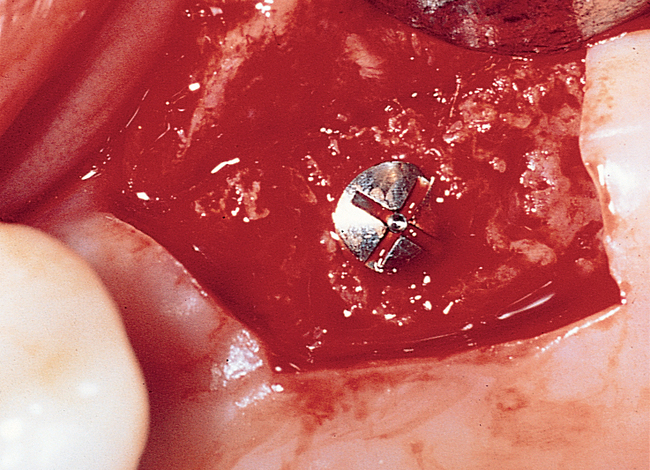
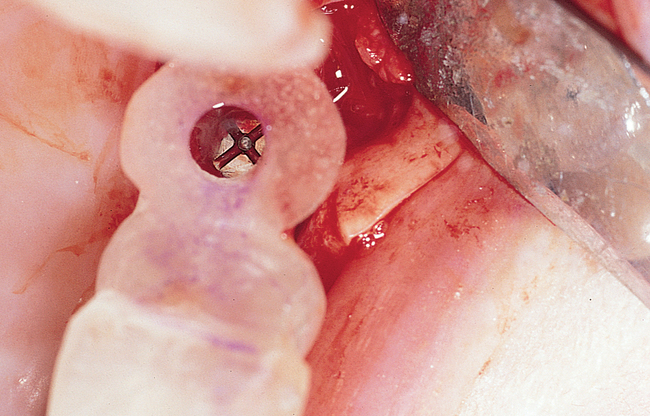
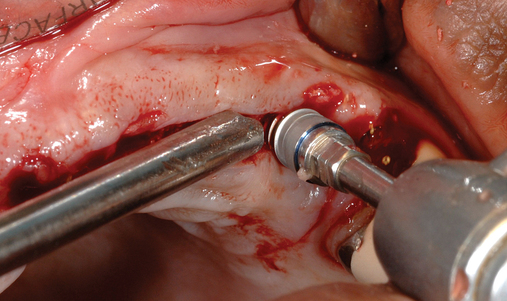
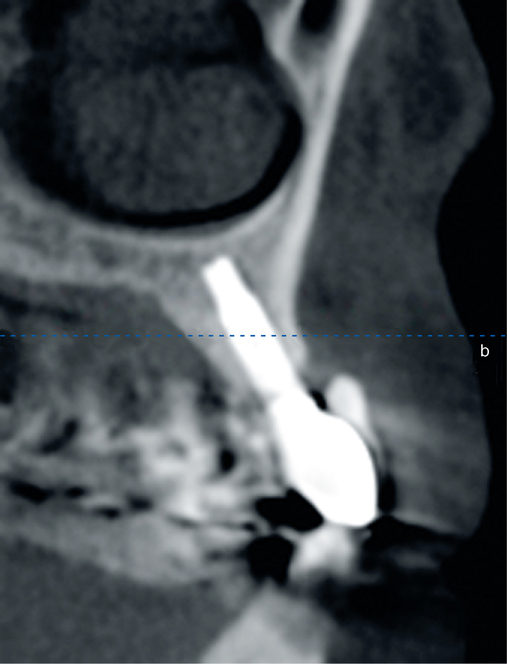
At the surgical visit, a local anesthetic is administered. The incision is made slightly palatal to the crest, with vertical release incisions flaring into the vestibule to keep the base of the flap wider than the crestal incision width (Figure 4-3). Full-thickness, subperiosteal labial and palatal flaps are reflected to expose the crest and allow visualization of the vertical cortices of bone. The implant should be placed with its axis parallel to the occlusal forces, and the emergence of the implant should be angled to meet the buccal cusps of the mandibular teeth. A surgical guide stent can be used; however, if the neighboring dentition is in good repair and the mandibular dentition is well aligned, the fossae of the teeth can be used to direct implant placement.
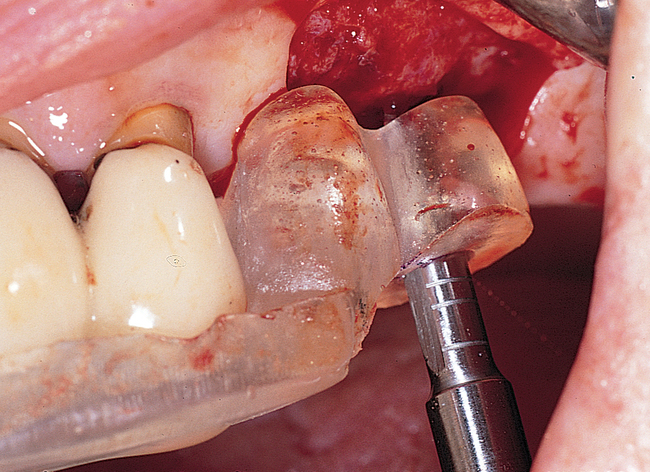

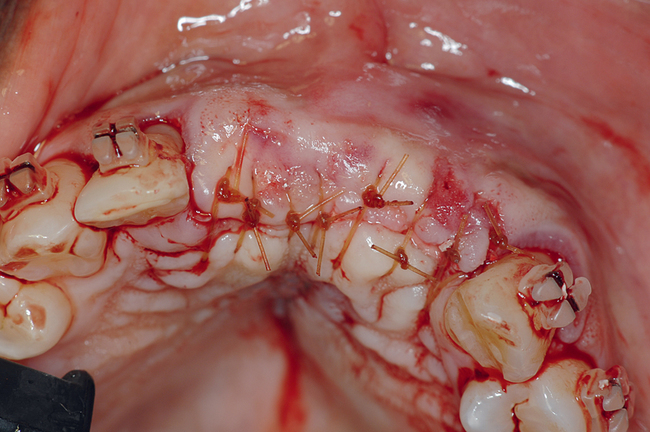
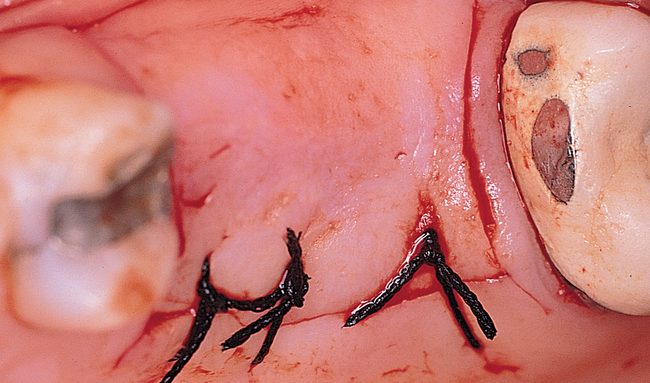
A round bur is used to mark the planned implant location. The graduating-sized drilling sequence is used, and the implant is placed. If extremely soft maxillary bone is felt, osteotomes may be used to compact the bone in the implant site, although minimal scientific information validates the assumption that compaction of bone with osteotomes helps the integration rate. If encountered in the labial bone, dehiscences are treated in a manner similar to that discussed previously for anterior maxillary implants. After the implant has been placed, the periosteum is released as necessary, and the incision is closed (Figure 4-4).
Multiple-teeth implant-borne restorations
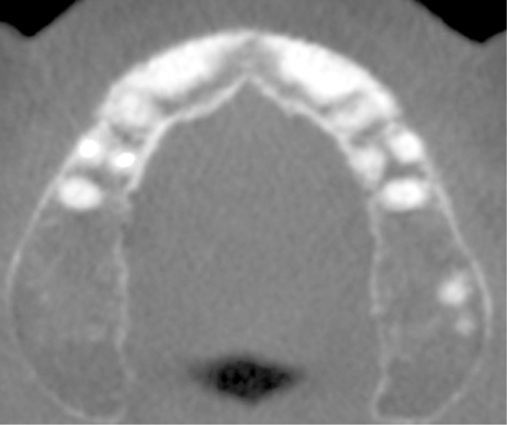
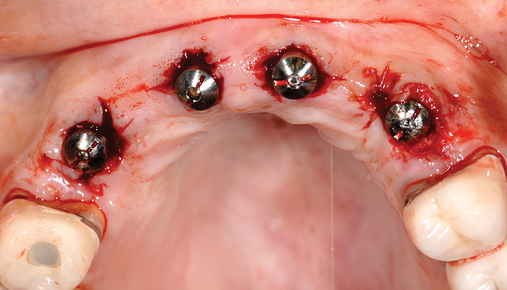
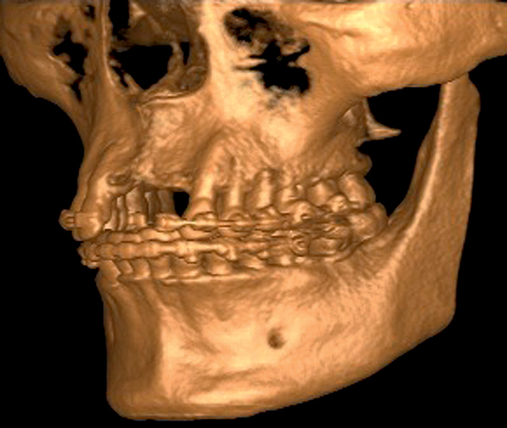
Patients may have sufficient vertical bone but may be deficient in the width projection of the bone, which is common after extraction of the maxillary teeth. The bone loss occurs especially after trauma or long-term loss of the teeth, leaving the palatal bone intact but the alveolus thin and deficient. The patient shown in Figure 4-5 lost his anterior maxillary teeth while in his college years, and he now desires a fixed prosthesis to replace his irritating partial denture.


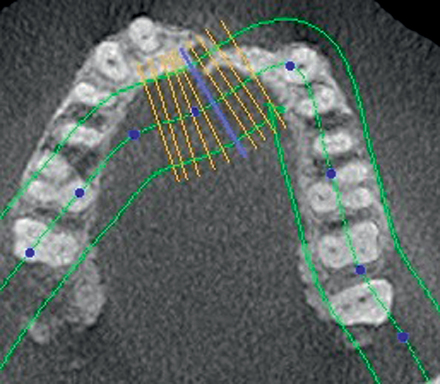
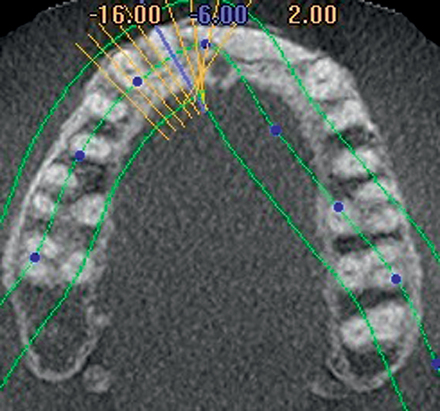
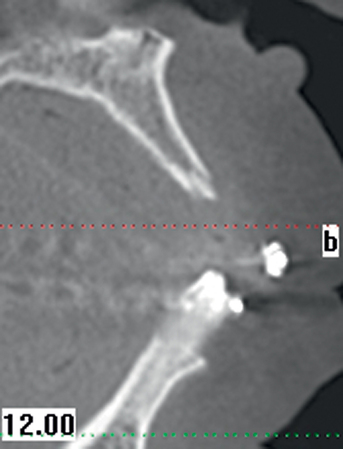
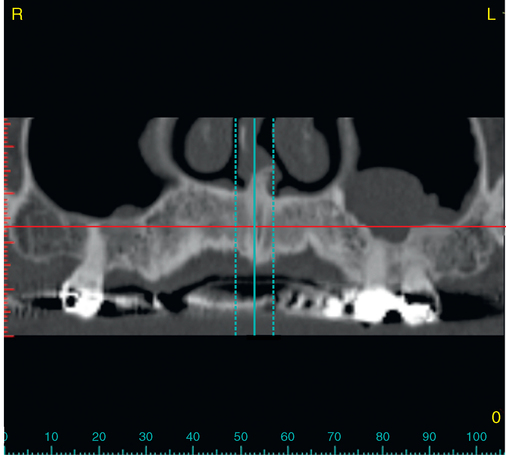
To assess the patient’s needs, a provisional restoration can be remade or modified. The patient shown in Figure 4-5 has a removable partial denture, which established his occlusion. It has a large flange. It can be used to provide a dual-scan prosthesis to plan the case treatment using virtual methods. The partial is duplicated in clear acrylic and fiduciary markers placed in the palatal portion. The cone-beam scan is taken with the duplicate in the patient’s mouth and by itself. The images are married on the software, and the implants can be placed on the computer demonstrating to the team the options available.
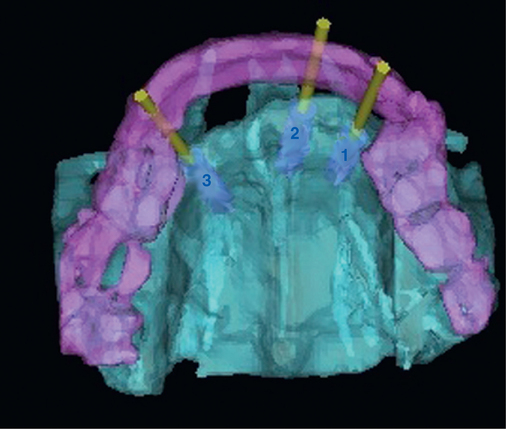
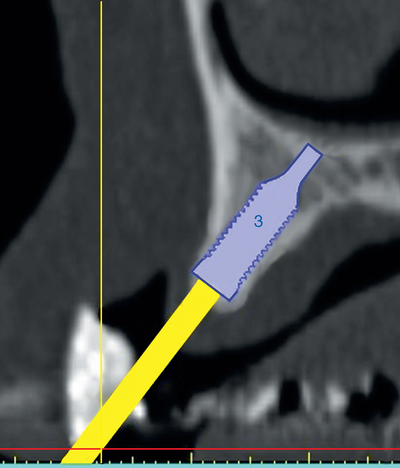
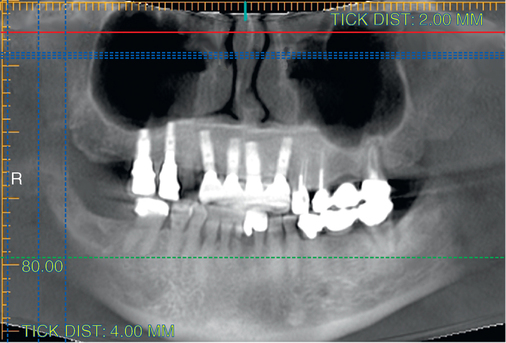


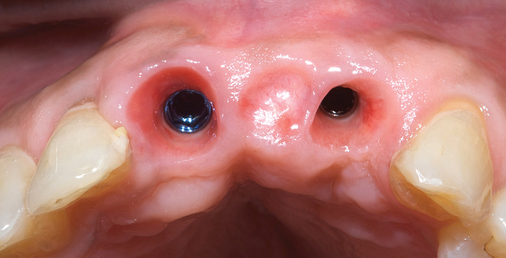
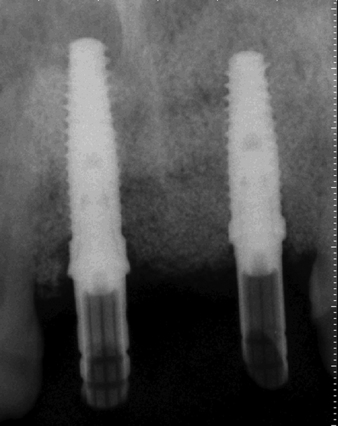
Combination of ridge augmentation with computed tomography–guided surgery and immediate provisionalization
Patients have had extensive dental work to save their teeth with root canal therapy, crown lengthening, and apicoectomies, which can result in fatigue, fracture of the posts and roots, or secondary deep caries. These patients desire fixed solutions with minimal time wearing removable provisional prostheses. As shown in Figure 4-6 (see the companion site for the complete case), the use of a fixed tooth–borne provisional prosthesis can help the patient through the process.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses