Chapter 6
Lip and Perioral Cosmetic Surgery
Introduction
The soft tissues of the perioral region provide the frame through which the smile is viewed. The importance of the smile in an individual’s ability to function socially has been well documented. Similarly, the significance of this soft tissue framework has also been recognized.1,2
In the young patient, improving the esthetics of the perioral region often involves optimizing the size, shape, and architecture of the lips. Underlying deficiencies of the bony substructure may also be addressed. In the mature patient, all these issues are also present, but in addition, numerous predictable changes occur with aging that also need to be recognized.
The process of aging can be easily recognized in this area and is influenced by both intrinsic and extrinsic factors.3–5 Intrinsic components include genetics and gender, while extrinsic elements include chronic ultraviolet (UV) light exposure, smoking, and repeated muscle movements. Volume changes and loss of architecture in the soft tissues along with loss of craniofacial support contribute to age-related facial reshaping.
Predictable changes that occur with increasing age are loss of lip volume and architecture, lengthening of the upper lip with inversion, and rhytid formation. Therefore, creation of a more attractive perioral soft tissue window is directed toward addressing these issues. This chapter discusses improving perioral esthetics and the rejuvenation of the soft tissues focusing on both conservative and invasive surgical techniques.
Initial Interview and Medical Review
Despite the deceptively simple treatment options that are often involved in improving the appearance of the perioral region, the initial patient interview and review of medical history is just as important for achieving success as is the case when treating the apparently more complicated esthetic units of the face.
The patient interview should always begin with open-ended questions that allow the surgeon an opportunity to assess patient desires, motivation, and likelihood of achieving a satisfied client. Once a clear understanding is gained of the patient’s interests, discussion should turn to any previous cosmetic surgeries or treatment the patient may have undergone. Current skin care regimen, history of ablative resurfacing (chemical or laser), use of botulinum toxin therapy or injectable fillers, and their timing are all salient to further treatment.
Cosmetic surgery to improve other esthetic units of the face may also impact treatment of the perioral region. Irregular skin color, hypopigmentation, loss of skin texture, scarring, gross deviation from facial proportionate norms, and asymmetry of muscle activity all may provide clues as to previous surgical and nonsurgical treatments to the region. A history of acne and its treatment, in particular isotretinoin oral therapy, may alter options available to the patient and should be elicited.
A history of hypertrophic or keloid scarring should be explored. If the patient has received previous facial cosmetic treatment, it is instructive to elicit if the patient had a subjectively good outcome. The clinician must recognize what constitutes success or failure in the patient’s eyes. Similarly, one of the most common complications of any cosmetic procedure is unmet expectations. The patient interview and the dialogue that ensues is perhaps the best resource the surgeon has to avoid this pitfall. Finally, the patient’s medical history should be thoroughly reviewed to assess the suitability of health to easily tolerate any proposed treatment.
Evaluation and Diagnosis
The anatomical area that encompasses the perioral region extends vertically from the subnasale to the menton and includes the upper and lower lips, labiomental fold, and chin. The region is bounded laterally by the nasolabial (NL) folds superior to the commissure of the mouth, and the “marionette” (M) lines inferiorly. As the perioral region is bounded by other esthetic units of the face, it is important to recognize that procedures that influence the surrounding regions—nose, midface, lateral face, and neck—may also have some effect on the perioral tissues (Table 6.1).
Table 6.1 Changes in the perioral region effected by cosmetic procedures on adjacent esthetic units
| Adjacent esthetic unit | Adjunctive cosmetic procedure | Effect on perioral region |
| Nose | Rhinoplasty/tip plasty | Increase or decrease of nasolabial angle Modification of facial profile and facial E plane |
| Midface | Midface-lifting techniques Midface soft tissue augmentation Ablative skin resurfacing or dermal tightening procedure |
Improvement of nasolabial fold |
| Lateral face and neck | Rhytidectomy Ablative skin resurfacing or dermal tightening procedure |
Mild improvement of nasolabial fold Mild elevation of oral commissure Flattening and improvement of prejowl sulcus Decreased jowling |
| Maxilla/mandible | Maxillary orthognathic surgery Mandibular orthognathic surgery Genioplasty |
Increased or decreased dental display Increased or decreased prominence of lips with change in lip height and/or volume Improved or deepened nasolabial folds Maximal ability for change in facial profile and E plane |
Initial assessment focuses on skin characteristics and pathology, lip function, volume and architecture, and the relationship of the lips to dental structures at repose and smile, and to other esthetic units of the face.
Assessment of the skin generally begins with documentation of pigmentation and tolerance to sunlight. Although numerous methods have been presented, familiarity with Fitzpatrick’s sun-reactive scoring is a useful and well-recognized method. In addition, the nature of rhytids and degree of photoaging should be quantified using a classification, such as Glogau’s scale.6,7 It is also important to note dyspigmentations, telangiectasias, sebaceous activity, and general atrophy of the fat and muscle tissue of the lips and chin. History of previous or current acne activity and its sequelae—ice-pick scars, depressions, waviness, nodularity, and the presence of cysts—should also be quantified. The patient should be questioned in regard to past acne treatments including, as mentioned earlier, their use of isotretinoin. The clinician should always scrutinize for evidence of pathological skin lesions such as actinic keratosis, squamous cell carcinoma, basal cell carcinoma, and melanoma.
Functional examination of the perioral region can often be accomplished during the initial verbal interview of the patient. The clinician should sit level, opposite the patient, paying particular attention to evidence of hyperactivity of the orbicularis oris during normal speech. In the mature patient, this often presents as prominent vertical mimetic lines along the vermillion border of the upper and/or lower lip. It should be noted if the vertical rhytids persist at rest and what is their relative depth to the surrounding skin. The patient should be evaluated at full smile, at repose and pucker. Evidence of asymmetry in movement of the lips should be noted as this may suggest a history of prior cosmetic surgery or trauma, and should be discussed with the patient. The relationship of the lip to display (or lack thereof) of both the upper and lower dentition is noted. Occasionally, a patient may present with a prominent horizontal furrow in the upper lip that is only present during smile function. This furrow strongly suggests a long upper lip relative to the maxillary height.
Attention is next turned to evaluation of the esthetic subunit of the lips. Two anatomical elements provide the basis for the structure of the normal lip. The first provides the framework architecture and the second relates to the volume of the lip. Framework elements provide sharp contrasts of lighting and demarcate the vermillion cutaneous junction. They project the shape of the lip.
In the upper lip this is evidenced by the pout of the white line of lip and the philtral columns (Figure 6.1). These anatomical elements are produced primarily by the interaction of muscle insertions of the levator labii superioris and the orbicularis oris. The orbicularis oris muscle inserts into the ipsilateral and contralateral philtral column, while the levator labii superioris muscle only inserts into the ipsilateral philtral column. The white line of the lip symbolizes dermal insertion points of these muscle groups.
Figure 6.1 Lip morphology.

In the lower lip, the white line of the lip and its protrusion is the main architectural element, with particular prominence in the central third. The white line of the lower lip is primarily a result of the dermal insertion points of the orbicularis oris muscle, although small contributions from adjacent muscles of facial expression also play a role. The volume elements of the lip are represented by the shape and size of the vermillion, or red, portion of the lip, and the thickness of the skin-covered portion of the upper and lower lips. Volume of the skin portion of the lip derives from epidermis, dermis, a relatively thin subcutaneous fat layer, and a muscular layer.
The perioral musculature is composed of a superficial and deep layer. The superficial muscular layer is mostly composed of dense fascia that is suspended from the melolabial fold. The deeper layer is the muscular obicularis oris proper. The fibrous melolabial fold is firmly attached to insertions of the levator labii superioris (and alaque nasi), zygomaticus major and minor, and risorius muscles.8,9 In the upper lip, the morphology of the vermillion is formed by the central tubercle and the paired lateral extensions. In the lower lip, two general morphologies are seen: a unilobed lip or a symmetric bilobed lip. The red aspect of the vermillion is formed as a result of a thick vascular lamina propria viewed through a thinly keratinized squamous epithelium.
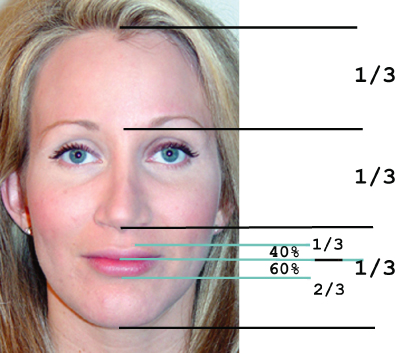
The volume and architecture of the lips must be viewed within the context of the surrounding facial features.10 The relative area of the volume component of the lip compared with the facial area has been shown to be a significant factor in whether a face should be considered to be youthful or attractive.11 A larger surface area of vermillion display to overall facial area is generally regarded as more youthful and attractive. In describing the proportions of the lower face, it is generally desirable for the ratio of subnasale-stomion to stomion-submentum to be 1:2. The surface area of vermillion display of the upper to lower lip comprises a ratio of 2:3 (Figure 6.2).
Figure 6.2 Facial ratios.
Maxillary incisor tooth display is an important aspect for a youthful appearance. Generally speaking, a young-looking incisal display at repose is regarded to be 3–4 mm for women and 2–3 mm for men, as viewed with the lips slightly parted.12 The clinician should note the arc of the inferior aspect of the upper lip as it crosses the maxillary anterior dentition. This inferior lip line is optimally almost horizontal or slightly elevated in the central portion of the lip with a gentle downward curve from the tubercle. An excessively elevated central portion of the lip may lead to the relative illusion of downturned commissures and premature aging of the region and a “sad” appearance to the mouth. This may prompt the clinician to explore options to elevate and support the commissures, while avoiding procedures that may raise the central portion of the lip.
Age-Related Changes to the Perioral Area
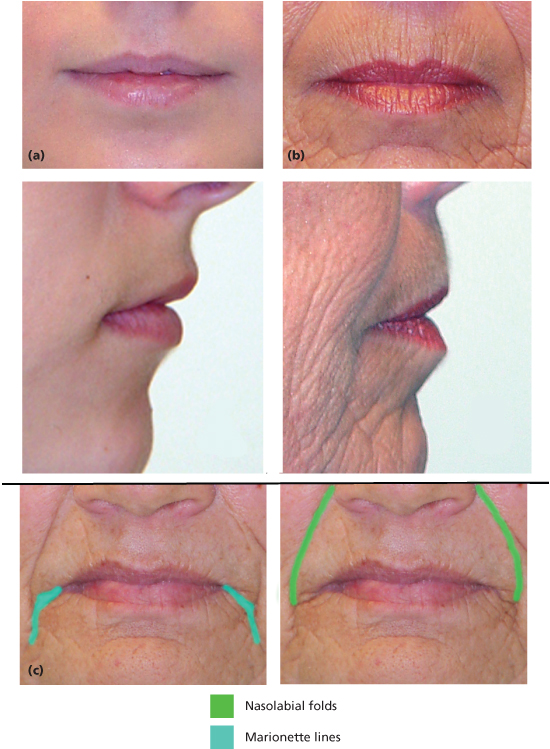
Aging of the perioral area is associated with many predictable changes, such as a loss of lip volume and architecture, lengthening of the upper lip with inversion, and rhytid formation. The loss in lip volume results primarily from soft tissue atrophy. During the process of normal aging, as the atrophy of fat, muscle, and connective tissue elements progresses, the framework elements become less pronounced. With increasing age, these elements flatten and eventually may become absent. In the upper lip, when there is atrophy of muscle, this is apparent where the muscle insertions form the philtral columns, white line of the lip, and Cupid’s bow. The philtral arches become flattened and the Cupid’s bow is less defined. This leads to a less than ideal and aged appearance. In the lower lip, atrophy is accompanied by a loss in muscle tone in the orbicularis oris, which results in the increasing display of the lower teeth at rest (Figure 6.3).
Figure 6.3 Age-related changes of the perioral region. (a) Patient under 21 years old. (b) Patient over 65 years old exhibiting loss of lip volume and architecture, lip lengthening and inversion, decreased dental display, and actinic changes. (c) A 67-year-old female with marked marionette lines and nasolabial folds.
Lengthening of the lip results from the synergistic interaction between the loss of lip volume and weakening of fascial attachments that suspend the soft tissue of the lip. Lip lengthening that occurs with decreased volume can be compared to the changes seen in a balloon as the air is removed. With decreasing amounts of air, the balloon becomes flaccid and elongated. Similarly, as soft tissue elements of the upper lip atrophy, a relative change is noted.
Additionally, fibrous attachments between the superficial muscular layer of the lip and the base of the nose and melolabial folds involute and weaken with increasing age and promote lip lengthening. As the upper lip lengthens, the visible portion of the red vermillion also tends to diminish and the lip appears to invert. This inversion of the inferior portion of the upper lip and a less visible vermillion causes a “thin-lipped” appearance. Ideally, the upper lip is 15–20 mm in length when measured from the NL junction to the white line of the lip at the height of the Cupid’s bow. An aged lip can be upward of 22–25 mm in length. The clinician should, however, be cautious of treating the lip to numbers, as the ideal length of the upper lip should be evaluated within the context of the entire facial proportions and the subjective preferences of the patient.
It is recommended that for purposes of evaluation and documentation, photographs should be taken of all patients prior to treatment. Photographic evaluation of the perioral region should focus on the frontal, profile, and three-quarter views of the face. The frontal views should include full smile, repose with lips closed, and repose with lips slightly parted to document tooth display. Photography provides a reference point for the clinician when discussing patient expectations. In the frontal evaluation, measurements of the upper lip, from the NL junction to the white line, and measurements of incisal display at repose and smiling should be documented. In addition, a measurement of the vermillion display at rest should be noted.
In terms of evaluating lip volume and architecture, the definition and prominence of the white line of the lip and philtral columns should be noted. General bulk and shape of the vermillion portion is evaluated. A prominent tubercle and lower lip pout are assessed.
Evaluation of the NL Folds and the M Lines
The NL folds and M lines effectively delineate the lateral extent of the perioral region (Figure 6.3). As discussed previously, the fibrous melolabial fold is formed by the firm attachment of the fascia of the superficial obicularis oris to insertions of the levator labii superioris (and alaque nasi), zygomaticus major and minor, and risorius muscles.8,9 The cheek mass superior to the fold is a result of contributions from the superficial fat layer, the fascia and the muscles of facial expression, known as the superficial muscular aponeurotic system (SMAS), and the discreet deeper fat pads (malar, suborbicularis oculi, and to a lesser extent, the buccal). In some patients, notable hypertrophy occurs in the superficial fat pad, leading to an excessive NL fold.
In the young patient, M lines are typically absent and the NL fold is evidenced as a slight depression extending from the ala of the nose laterally and inferiorly toward the commissure. A maxilla that exhibits anterior-posterior insufficiency may also contribute to a deeper NL fold in the young patient.
As the patient ages, the NL fold will typically become more evident as a result of attenuation of fascial structures and the descent of superficial and deep fat pads.1,2 Often a relative decrease in the deep fat pad volume is noted compared with the superficial layer. This contributes to the loss of support of the cheek mass and its descent. In addition, hormonal and actinic-related changes in the skin result in decreased skin elasticity and thickness that further accentuate the loss of support. M lines often begin to appear in the fourth decade of life and can be considered an inferior extension the same forces that cause the soft tissue descent of the cheek mass. In a subset portion of patients, atrophy of soft tissue is noted in the prejowl region that accentuates the M lines. In addition, it has been noted that bony resorption occurs in the anterior maxilla, nasal sill, and mandible that further deprojects the soft tissue of the perioral area. A significant loss of maxillary or mandibular dentition may augment this effect.
Effects of Sun Exposure to the Perioral Area
As a result of chronic UV exposure, surface changes occur in the skin and subcutaneous tissues along with histological alteration. With actinic damage, the number of epidermal Langerhans cells decrease. The epidermis can become atrophied as well as show irregular distribution of pigment and cellular atypia. The epithelium can show an accumulation of thick basophilic fibrous material in the superficial reticular dermis that results in elastosis. As this elastotic tissue accumulates, it pushes out collagen fibers and blood vessels, causing telangiectasias, erythema, decreased elasticity, coarse dry skin, and blotchy pigmentation. In addition, chronic actinic damage can cause vertical rhytids, which are initially fine and radially oriented. As actinic damage accumulates, the rhytids deepen and eventually become horizontally oriented.
A Problem Oriented Approach to Treatment
In deciding on a treatment plan to improve esthetics in the perioral region, it is useful to consider an outside-in, problem-based approach. In general terms, one should consider the following: (1) improving cosmesis of the skin; (2) optimizing volume and architectural elements in the lips, NL folds, and M lines; and (3) optimizing the display of the dentition and maxillary gingiva13–15 (Table 6.2).
Table 6.2 Problem-based treatment planning for the perioral region
| Perioral cosmetic deformity | Affected tissues | Recommended treatment |
| Rhytids at rest Dyspigmentations Telangectasias |
Epidermis and dermis of skin | Appropriate homecare regimen Ablative skin resurfacing Nonablative skin treatment |
| Vertical mimetic rhytids Mimetic downturned oral commissures |
Obicularis oris Depressor anguli oris |
Chemical denervation with botulinum toxin therapy |
| Deep vertical lip rhytids | Epidermis, dermis, subcuticular tissue | Injectable filling agent Ablative skin resurfacing |
| Flattened or absent lip architecture | White line of lip, Cupid’s bow, philtral columns | Injectable filling agent |
| Atrophic body of upper and/or lower lip | Body of lip | Injectable filling agent Surgically placed grafts or implants |
| Deep nasolabial folds | Ptotic midface, maxillary anterior deficiency, atrophic upper lip | Injectable filling agent Surgically placed grafts or implants Surgical excision of nasolabial fold Surgical augmentation of maxilla/nasal sill |
| Marionette lines, downturned oral commissures | Oral commissure Lower lip and lateral face |
Injectable filling agent Surgical commissuroplasty |
| Excessive gingival display at smile Excessive dental display at repose |
Body of upper lip | Injectable filling agent Surgically placed graft or implant |
Skin
Following assessment of the skin, the presence of fine lines and wrinkles suggest an appropriate use of skin tightening and ablative resurfacing options. These may include ablative laser or chemical resurfacing agents. Dyspigmentations and/or vascular telangiectasias are optimally treated with nonablative therapy such as intense pulsed light (IPL) or pulsed dye laser. Significant vertical mimetic lines suggest the use of a chemical denervation agent such as botulinum toxin. Deeper dermal-based rhytids seen at rest may benefit from an injectable filler. A patient with a combination of the above problems would be optimally treated with a amalgamation of all of the above treatments which will be discussed further in detail.
Volume and Architectural Elements of the Lips, NL Folds, and M Lines
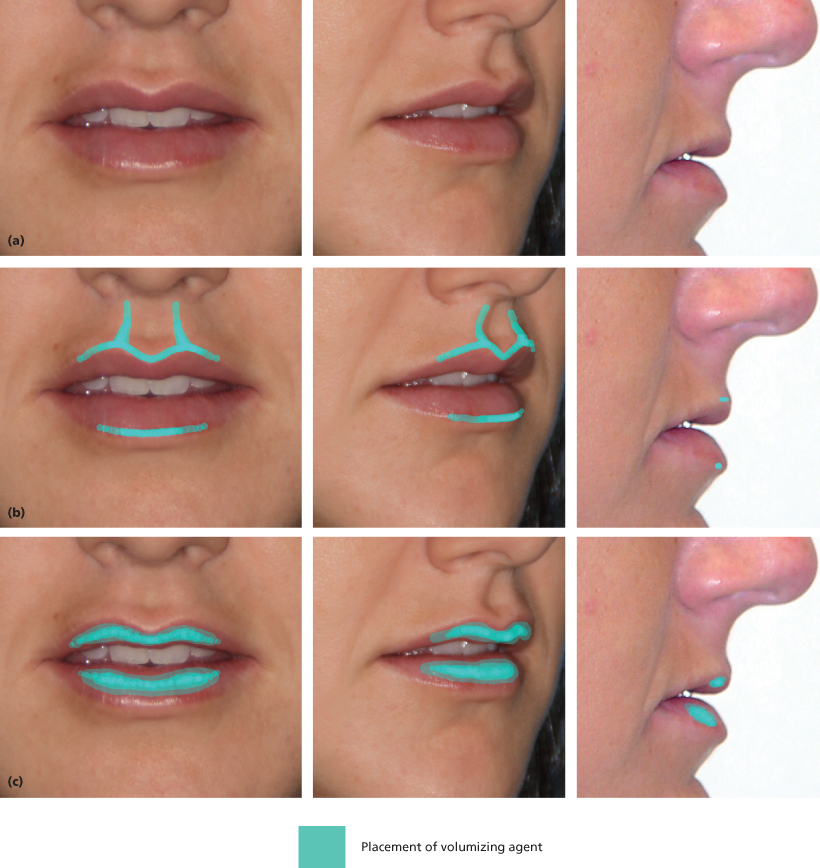
The creation of a sharply demarcated white line, philtral column, and Cupid’s bow is best accomplished with a volumizing agent that can be placed with a high degree of accuracy and a minimal amount of tissue distortion16–18 (Figure 6.4). Typically, this will involve the use of an injectable filling substance.
Figure 6.4 Ideal position of filler material in the lips: architecture and volume. (a) Patient’s normal anatomy. (b) Ideal placement of filler to improve architecture. (c) Ideal placement of filler to improve volume of body of the lip.
For gross addition of volume to the lips, in particular the vermillion, more treatment options are available. While injectable fillers continue to provide a very reliable method to augment the body of the lip, surgical placement of strips or tubes of autologous, alloplastic, or synthetic material is also possible.19,20 Minor improvement in lip volume can also be achieved utilizing classical V-Y mucosal rearrangement techniques. If vertical augmentation of the vermillion is desired in the thin-lipped patient, various lip-lifting techniques may be employed (either subnasal or vermillion border excision) that focus on the removal and closure of skin from the upper lip with focus on lip eversion. These techniques may also be used to improve dental display.
Management of the NL folds and M lines is somewhat more complicated as both morphological entities exist as a transition zone between esthetic units of the face. Midface-lifting and face-lifting techniques may be required for optimal correction and are beyond the scope of this chapter. Instead, this chapter will focus on techniques for adding volume to the lip as it transitions into the NL fold and M line. Injectable fillers as well as surgical placement of autogenous, allogenic, and synthetic materials can be useful (Figure 6.5). These agents can be used to augment the underlying bony base of the maxilla and nasal sill, or the overlying soft tissue. In patients with severe skin furrowing and rhytids, it may be advantageous to surgically excise a portion of the NL fold, allowing the scar to fall />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


