The Flap Technique for Pocket Therapy
Several techniques can be used for the treatment of periodontal pockets. The periodontal flap is one of the most frequently employed procedures, particularly for moderate and deep pockets in posterior areas (see Chapter 57).
Overview
Flaps are used for pocket therapy to accomplish the following:
1. Increase accessibility to root deposits for scaling and root planing
2. Eliminate or reduce pocket depth via resection of the pocket wall
3. Gain access for osseous resective surgery, if necessary
4. Expose the area for the performance of regenerative methods
To fulfill these purposes, several flap techniques are available and in current use.
Technique for Access and Pocket Depth Reduction or Elimination
The modified Widman flap has been described for exposing the root surfaces for meticulous instrumentation and for the removal of the pocket lining.6 Again, it is not intended to eliminate or reduce pocket depth, except for the reduction that occurs during healing as a result of tissue shrinkage.
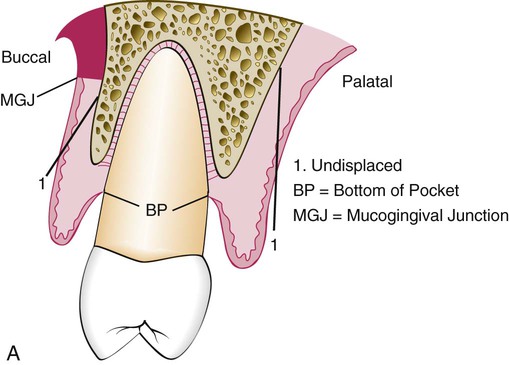
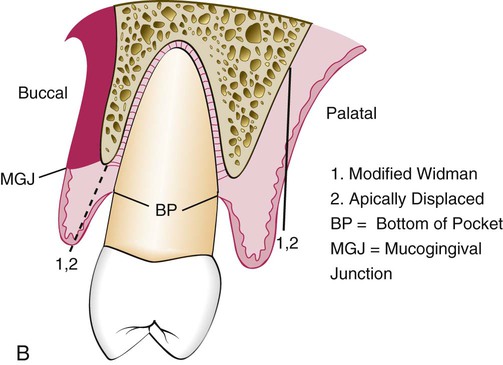
The apically displaced flap provides accessibility and eliminates the pocket, but it does the latter by apically positioning the soft-tissue wall of the pocket.2 Therefore, it preserves or increases the width of the attached gingiva by transforming the previously unattached keratinized pocket wall into attached tissue. This increase in the width of the attached gingiva is based on the apical shift of the mucogingival junction, which may include the apical displacement of the muscle attachments. A study made before and 18 years after the use of apically displaced flaps failed to show a permanent relocation of the mucogingival junction.1
Incisions
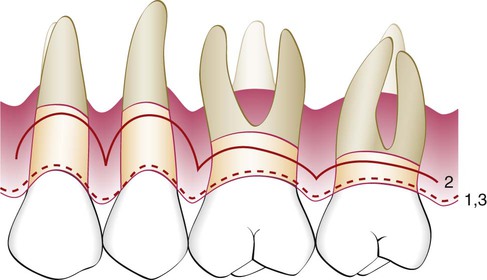
All three flap techniques that were just discussed involve the use of the basic incisions described in Chapter 57: the internal bevel incision, the crevicular incision, and the interdental incision. However, there are important variations in the way these incisions are performed for the different types of flaps (Figures 59-1 and 59-2). The internal beveled incision for the modified Widman flap closely follows the scalloped outline of the dentition to minimize the loss of the attached keratinized gingiva. This incision is made 1 mm to 2 mm from the teeth. The gingival margin is removed, and the flap is reflected to gain access for root therapy.
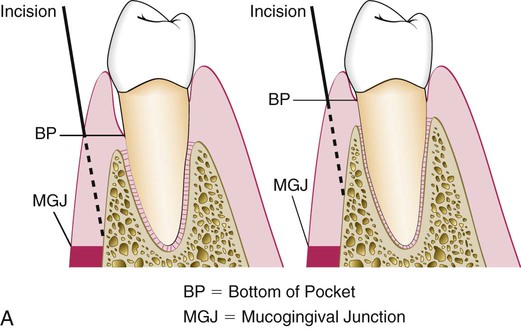
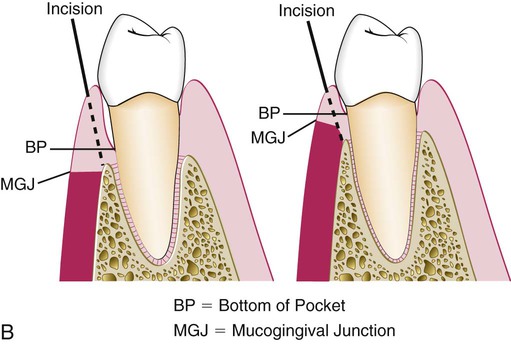
The apically displaced flap technique is selected for cases that present a minimal amount of keratinized, attached gingiva. For this reason, the internal bevel incision should be made as close to the tooth as possible (i.e., 0.5 mm to 1.0 mm) (see Figure 59-1). There is no need to determine where the bottom of the pocket is in relation to the incision for the apically displaced flap as one would for the undisplaced flap. The flap is placed at the tooth–bone junction by apically displacing the flap. Its final position is not determined by the placement of the first incision.
For the undisplaced flap, the internal bevel incision is initiated at or near a point just coronal to where the bottom of the pocket is projected on the outer surface of the gingiva (see Figure 59-1). This incision can be accomplished only if sufficient attached gingiva remains apical to the incision. Therefore, the two anatomic landmarks—the pocket depth and the location of the mucogingival junction—must be considered to evaluate the amount of attached gingiva that will remain after the surgery has been completed. Because the pocket wall is not displaced apically, the initial incision should eliminate the pocket wall. Thus, an incision should not be made too close to the tooth, because it will not eliminate the pocket wall, and it may result in the re-creation of the soft-tissue pocket. If the tissue is too thick, the flap margin should be thinned with the initial incision. The proper placement of the flap margin at the tooth–bone junction during closure is important to prevent either recurrence of the pocket or the exposure of bone. The internal bevel incision should be scalloped into the interdental area to preserve the interdental papilla (see Figure 59-2). This will allow better coverage of the bone at both the radicular and interdental areas.
Reconstructive Techniques
The techniques that are used to achieve reconstructive and regenerative objectives are the papilla preservation flap8 and the conventional flap, which involve only crevicular or pocket incisions. This will allow the clinician to retain the maximum amount of gingival tissue, including the papilla, which is essential for graft or membrane coverage.
Modified Widman Flap
In 1965, Morris4 revived a technique described early during the twentieth century in the periodontal literature; he called it the “unrepositioned mucoperiosteal flap.” Essentially, the same procedure was presented in 1974 by Ramfjord and Nissle,6 who called it the “modified Widman flap” (Figure 59-3). This technique offers the possibility of establishing an intimate postoperative adaptation of healthy collagenous connective tissue to tooth surfaces,2,3,5,6 and it provides access for adequate instrumentation of the root surfaces and immediate closure of the area. The following steps outline the modified Widman flap technique.

Step 1: The initial incision is an internal bevel incision to the alveolar crest starting 0.5 mm to 1 mm away from the gingival margin (Figure 59-3, C). Scalloping follows the gingival margin. Care should be taken to insert the blade in such a way that the papilla is left with a thickness similar to that of the remaining facial flap. Vertical relaxing incisions are usually not needed.
Step 2: The gingiva is reflected with a periosteal elevator (Figure 59-3, D).
Step 3: A crevicular incision is made from the bottom of the pocket to the bone in such a way that it circumscribes the triangular wedge of tissue that contains the pocket lining.
Step 4: After the flap is reflected, a third incision is made in the interdental spaces coronal to the bone with a curette or an interproximal knife, and the gingival collar is removed (Figure 59-3, E and F).
Step 5: Tissue tags and granulation tissue are removed with a curette. The root surfaces are checked and then scaled and planed, if needed (Figure 59-3, G and H). Residual periodontal fibers attached to the tooth surface should not be disturbed.
Step 6: Bone architecture is not corrected unless it prevents good tissue adaptation to the necks of the teeth. Every effort is made to adapt the facial and lingual interproximal tissue adjacent to each other in such a way that no interproximal bone remains exposed at the time of suturing. The flaps may be thinned to allow for close adaptation of the gingiva around the entire circumference of the tooth and to each other interproximally.
Step 7: Continuous, independent sling sutures are placed in both the facial and palatal areas (Figure 59-3, I and J) and covered with a periodontal surgical pack.
Ramfjord and Nissle6 performed an extensive longitudinal study that compared the Widman procedure (as modified by them) with the curettage technique and the pocket elimination methods, which include bone contouring when needed. The patients were assigned randomly to one of the techniques, and results were analyzed yearly for up to 7 years after therapy. The researchers reported similar results for each of the three methods tested. Pocket depth was initially similar for all methods, but it was maintained at shallower levels with the Widman flap; the attachment level remained higher with the Widman flap.
Undisplaced Flap
Step 1: The pockets are measured with the periodontal probe, and a bleeding point is produced on the outer surface of the gingiva to mark the pocket bottom.
Step 2: The initial or internal bevel incision is made (Figure 59-4) after scalloping the bleeding marks on the gingiva (Figure 59-5). The incision is usually carried to a point apical to the alveolar crest, depending on the thickness of the tissue. The thicker the tissue is, the more apical the ending point of the incision (see Figure 59-4). In addition, thinning of the flap should be performed with the initial incision, because it is easier to accomplish at this time than it is later with a loose, reflected flap that is difficult to manage. (The use of this technique in palatal areas is considered in the discussion that follows this list.)
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses