Phase II Periodontal Therapy
Although in a strict sense, all instrumental therapy can be considered surgical, this chapter refers only to those techniques that include the intentional severing or incising of gingival tissue* with the following purposes:
Objectives of the Surgical Phase
The surgical phase of periodontal therapy has the following main objectives:
The purpose of surgical pocket therapy is to eliminate the pathologic changes in the pocket walls; to create a stable, easily maintainable state; and if possible, to promote periodontal regeneration. To fulfill these objectives, surgical techniques (1) increase accessibility to the root surface, making it possible to remove all irritants; (2) reduce or eliminate pocket depth, making it possible for the patient to maintain the root surfaces free of plaque; and (3) reshape soft and hard tissues to attain a harmonious topography. Pocket reduction surgery seeks to reduce pocket depth by either resective or regenerative means or often by a combination of both methods (Box 53-1). Chapters 59 to 61 describe the different techniques used for these purposes.
The second objective of the surgical phase of periodontal therapy is the correction of anatomic morphologic defects that may favor plaque accumulation and pocket recurrence or impair esthetics. It is important to understand that these procedures are not directed to treat disease but aim to alter the gingival and mucosal tissues to correct defects that may predispose to disease. They are performed on noninflamed tissues and in the absence of periodontal pockets. Three types of techniques fall into this category, as follows (see Box 53-1):
• Plastic surgery techniques are used to create or widen the attached gingiva by placing grafts of various types.
• Esthetic surgery techniques are used to cover denuded roots and to recreate lost papillae.
• Preprosthetic techniques are used to adapt the periodontal and neighboring tissues to receive prosthetic replacements; these include crown lengthening, ridge augmentation, and vestibular deepening.
The plastic and esthetic surgery techniques are presented in Chapter 63 and the preprosthetic techniques in Chapter 66.
In addition, periodontal surgical techniques for the placement of dental implants are available. These involve not only the implant placement techniques but also a variety of surgical procedures to adapt the neighboring tissues, such as the sinus floor or the mandibular nerve canal, for subsequent placement of the implant (see Box 53-1). These methods are discussed in Chapters 75 and 77.
Surgical Pocket Therapy
The effectiveness of periodontal therapy is predicated on success in completely eliminating calculus, plaque, and diseased cementum from the tooth surface. Numerous investigations have shown that the difficulty of this task increases as the pocket becomes deeper.2,5 The presence of irregularities on the root surface also increase the difficulty of the procedure. As the pocket becomes deeper, the surface to be scaled increases, more irregularities appear on the root surface, and accessibility is impaired.11,15 The presence of furcations will also create insurmountable problems for scaling the root surface4 (see Chapter 62).
These problems can be reduced by resecting or displacing the soft tissue wall of the pocket, thereby increasing the visibility and accessibility of the root surface.3 The flap approach and the gingivectomy technique attain this result.
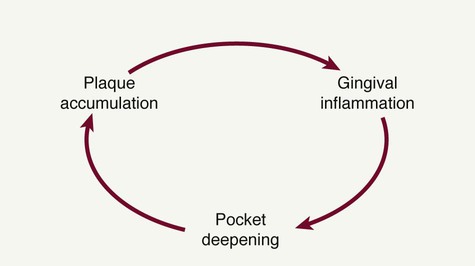
The need to eliminate or reduce the depth of the pocket is another important consideration. Pocket elimination consists of reducing the depth of periodontal pockets to that of a physiologic sulcus to enable cleansing by the patient. By proper case selection, both resective techniques and regenerative techniques can be used to accomplish this goal. The presence of a pocket produces areas that are impossible for the patient to keep clean, which establishes the vicious cycle depicted in Figure 53-1.
Results of Pocket Therapy
A periodontal pocket can be in an active state or a period of inactivity or quiescence. In an active pocket, underlying bone is being lost (Figure 53-2, top left). It often can be diagnosed clinically by bleeding, either spontaneously or on probing. After Phase I therapy, the inflammatory changes in the pocket wall subside, rendering the pocket inactive and reducing its depth (Figure 53-2, top center). The extent of this reduction depends on the depth before treatment and the degree to which the depth is the result of the edematous and inflammatory component of the pocket wall.
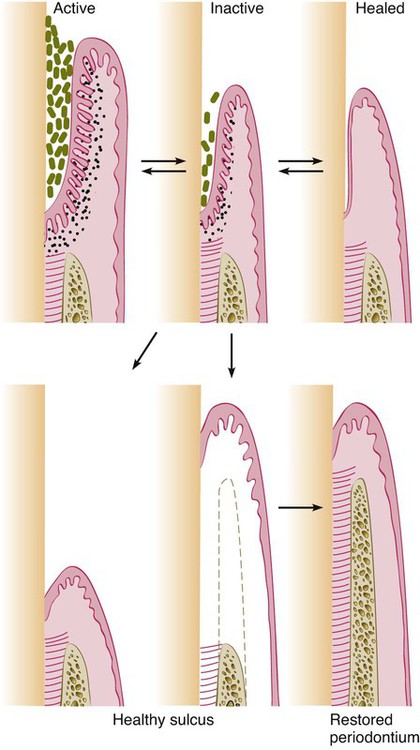
Inactive pockets can sometimes heal with a long junctional epithelium (Figure 53-2, top right). However, this condition also may be unstable, and the chance of recurrence and re-formation of the original pocket is always present because the epithelial union to the tooth is weak. However, one study in monkeys has shown that the long junctional epithelial union may be as resistant to plaque infection as a normal connective tissue attachment.9
Studies have shown that inactive pockets can be maintained for long periods with little loss of attachment by means of frequent scaling and root-planing procedures.6,10,12 A more reliable and stable result is obtained, however, by transforming the pocket into a healthy sulcus. The bottom of the healthy sulcus can be located either where the bottom of the pocket was localized or coronal to it. In the first case, there is no gain of attachment (Figure 53-2, bottom left), and the area of the root that was previously the tooth wall of the pocket becomes exposed. This does not mean that the periodontal treatment has caused recession but rather that it has uncovered the recession previously induced by the disease.
The healthy sulcus can also be located coronal to the bottom of the preexisting/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses