Chapter 5
Types of sedation
LEARNING OUTCOMES
At the end of this chapter you will have a clear understanding of:
- The various modes of sedation provided to patients.
- The way each mode is administered and acts upon the body.
- The advantages, disadvantages, indications and contraindications of usage.
INTRODUCTION
Patients are offered different modes of sedation depending upon their medical, dental and social history, preference, cost and team experience. The mode chosen is identified through an assessment appointment and all modes are independent of each other but can be used in conjunction. All modes of sedation act on the body differently, with the patient having to comply with the different restraints of each mode to enable them to receive it. The common forms of dental sedation provided to patients are:
- Intravenous
- Off-licence (transmucosal) sedation (It is an advanced technique which should only be used in exceptional circumstances.)
- Inhalation
- Oral sedation (It is not widely used but plays an important role within the provision of treatment with or without other forms of sedation as it reduces anxiety [1].)
INTRAVENOUS SEDATION
A cannula is placed into a vein and a drug is administered directly into the patient’s blood stream which results in sedation. The drug used is titrated (given) according to the patient’s response and is age related, not weight related as is a general anaesthetic. The most widely used drug is midazolam (Hypnovel). It belongs to the family of benzodiazepines drugs and its clinical actions and advantages are:
- It is anxiolytic to reduce a patient’s anxiety levels.
- It is hypnotic to induce sleep.
- It is anticonvulsant to reduce the risk of a convulsive fit.
- It is a muscle relaxant.
- It produces anterograde amnesia. The patient will be aware of treatment but may not remember anything after the first increment of drug.
- It lowers the blood pressure and in return the body responds by raising the pulse rate to increase the cardiac output, thus raising the blood pressure.
- Less pain is experienced at the injection site.
- It results in sedation, thus allowing treatment to take place.
- It causes slurred speech and impaired coordination, indicating that the patient is sedated enough to commence treatment.
- It has a rapid onset with a pronounced effect and is short acting.
- It is water soluble, so a non-irritant.
- It can be titrated to produce a desired effect to reflect individual patient’s needs.
- As a patient’s vein is continually maintained drugs can be provided in the event of an emergency or if the patient becomes over sedated.
- Patient recovery time is faster than with oral or intramuscular drugs.
- Nausea and vomiting rarely occur.
- It reduces the gag reflex slightly [1,2].
Its disadvantages are:
- Venepuncture is mandatory and therefore needle phobics are not always conducive or cooperative to this form of sedation.
- Training is required to undertake venepuncture and it requires great skill.
- The site of venepuncture can cause problems.
- An experienced second appropriate person must be available to clinically monitor the patient at all times.
- It can cause respiratory depression to reduce the respiratory drive.
- It can have a minimal effect on the cardiovascular system (depressing it).
- Due to the rapid onset of midazolam, its action and its more pronounced effects, the risk of any potential complication is elevated.
- It does not provide any analgesia, therefore a local anaesthetic would be required for pain relief where applicable.
- Paradoxical effects occasionally occur in children and the elderly.
- Appointment times need to be longer to allow for the patient’s recovery period.
- Consent must be taken, with every eventuality being considered, discussed and agreed prior to its provision.
- Patients must be able to comply with the rigid pre and post-operative instructions that intravenous sedation attracts. Most clinicians will give very similar instructions to patients. However, some may give additional instructions or alternatives that are their preference and/or specific to their area of work. Generic instructions are:
- To be accompanied by a responsible adult to act as an escort. This person must remain at the surgery while treatment takes place and accompany the patient home by car. They must also be able to stay with the patient for the next 24 hours and be free of other responsibilities. The reason: The clinician has a duty of care to ensure that when a patient leaves the surgery they are adequately supervised and cared for so that they come to no harm.
- Not to be in charge of other people on the day of sedation. The reason: To allow the patient to rest and recover from treatment.
- Not to make any responsible decisions or sign any legal documents for the remainder of the day. The reason: It may not be remembered.
- Not to drive any vehicle, operate machinery, climb ladders or scaffolding. The reason: It is illegal to drive under the influence of drugs — judgement and coordination will be impaired.
- Not to eat or drink for 4 hours prior to the appointment time. Some clinicians do not request their patients to be starved of food and drink but advise a light meal a few hours prior to the appointment. The reason: When a person is starved of food and drink they are more difficult to cannulate as they could be dehydrated, plus they could collapse due to lack of food.
- To wear loose clothing with sleeves that can easily be pulled above the elbow and not to wear high-heel shoes. The reason: Tight clothing restricts breathing making it more difficult to monitor and once sedation is complete it is preferable for the patient to be wearing flat shoes to avoid the risk of stumbling.
- To remove any nail varnish. The reason: It can interfere with the pulse oximeter, giving an incorrect reading.
- To avoid alcohol on the day of sedation. The reason: Alcohol will potentiate (speed up) the sedation drug.
- To ensure that their teeth and gums are clean. A clean mouth heals more quickly [1,2].
Midazolam (Hypnovel)
Midazolam is a short-acting benzodiazepine, one of approximately 35 benzodiazepines which are currently being used medically as sedative drugs. Although it was produced in the 1970s, it didn’t become available for use until the 1980s. In the 1990s it was accepted that it was very effective in the management of status epilepticus and could be administered intramuscularly. It is a clear odourless liquid in glass ampoules that can be obtained as:
- 10mg in 5ml
- 10mg in 2ml
- 5mg in 5ml (Figure 5.1)
Figure 5.1 Ampoule of midazolam.

Figure 5.2 Box of midazolam.
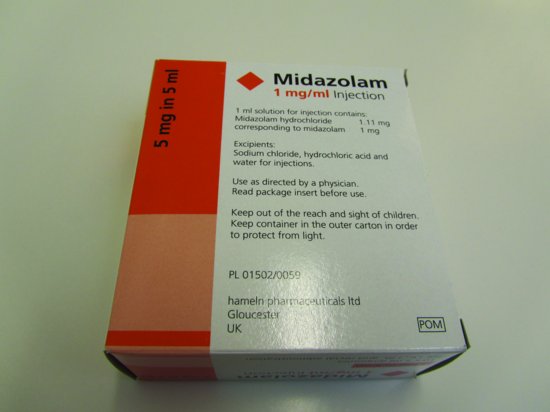
The recommended presentation for use in the dental surgery is 5mg in 5ml as this helps to prevent the risk of over sedation. Each box obtained will contain glass ampoules of midazolam that are stamped with the name, concentration, expiry date and the batch number (Figure 5.2). Midazolam is a controlled drug, and should, be under lock and key and treated as such with the ampoules being stored in the outer carton to protect them from light [1,2].
Pharmacology (action within the body)
Within the central nervous system (CNS) there are benzodiazepine receptors that allow benzodiazepine drugs to bind to them. These receptors are parallel to gamma-aminobutyric acid (GABA) receptors. Benzodiazepine does not directly activate GABA receptors but enhances the effect of neurotransmitters on the GABA receptors resulting in inhibition of brain activity. Therefore, conscious sedation is achieved by midazolam acting on the CNS thus reducing the excitability of the neurons in the mid brain, resulting in either the slowing down or stopping of certain nerve signals with the brain. All drugs have a half-life. This means the time it takes for the plasma level of the drug to drop to half. Benzodiazepines have two stages which form their half-life and comprise the following:
- Alpha: Distribution and redistribution. This is where the drug is introduced into the body, taken to the brain and then redistributed to other areas of the body.
- Beta: Metabolism and excretion. This is where the drug is broken down by the body and eliminated.
The distribution (alpha) half-life of midazolam is 4–18 minutes with the elimination (beta) half-life being 1–4 hours. Approximately 5mg of drug will be eliminated from the body within 5 hours. However, in the elderly and adolescents the elimination half-life is longer. When midazolam is titrated, it is thought to go through four phases of sedation very quickly with the patient reaching phase IV after an hour [1–3].
Phases of sedation
Phase I
The midazolam within the blood at the site of the brain is at its maximum — therefore it is at this point that the sedation technique will also be at its maximum. This will result in the patient’s coordination being impaired and their speech slurred. These signs of sedation can be established by talking to the patient, noting the change in their speech and requesting that they touch their nose. If they are successful in touching their nose they are classed as Eve sign negative and therefore not sedated sufficiently, but if they are unable to locate their nose they are Eve sign positive and sedated enough to commence treatment. At this stage the patient will be unaware of their surroundings and the team and will experience/notice a period of almost total amnesia, despite them conversing quite normally [1,2].
Phase II
As the amount of midazolam within the blood will now start to decrease so will the effects of sedation. This is attributed to the midazolam being redistributed to other tissues within the body (alpha half-life). As a result, the patient will experience an awareness of their surroundings and the team as the amnesic effect decreases. This means that some patients may remember parts of their treatment [1,2].
Phase III
It is at this stage that the patient will start to feel normal and will still appear to look relaxed. They will not be anxious as the anxiolytic effect of midazolam is still active. They will not experience any pain because of the numbing effects of the local anaesthetic [1,2].
Phase IV
The patient will look and feel recovered. It must be remembered that the patient is not fully recovered at this stage as it is only the alpha half-life (distribution and redistribution) that has occurred. The midazolam has yet to undergo the beta half-life (metabolism and excretion) and is therefore still present within the body. The amnesic effects of midazolam must also not be forgotten. They can be profound enough to last until phase IV of the sedation, meaning that the post-operative instructions must be reiterated and always provided in writing to both the patient and escort [1,2].
Administration of midazolam
If a patient has received previous treatment with intravenous sedation, well-written notes will provide an indication of how well the patient responded and the amount they received. The dose titrated can then be adjusted accordingly. The usual administration of midazolam for a young person who is classified as an ASA I (as explained in Chapter 4) is:
- Initial bolus of 2mg over 30 seconds. Patient response will be observed and monitored for 2 minutes.
- After 2 minutes, a further 0.5–1mg is administered until the level of sedation required has been achieved, with the usual dose being between 2.5 and 7.5mg.
As the elderly are much more sensitive to midazolam its administration must be slower, allowing longer periods between the titrations. This avoids over sedation with the initial bolus being slowly administered over 2 minutes with the dose being as low as 1–1.5mg. The total amount of midazolam given may not need to exceed 3.5mg. The reason is that elderly patients’ arm brain time is much slower than that of younger patients. If midazolam is titrated in the same way to an elderly patient it could lead to over sedation. Upon administration of midazolam the elderly patient may not appear sedated as it takes longer for the dose to travel to the brain than that of the younger patient. If further increments of midazolam are administered the initial dose will eventually reach the brain. This initial dose may have been enough to sedate the patient. However, the body still contains the additional increments and they will not have yet reached the brain. Once they do, it could result in an over sedated patient [1].
Side effects of midazolam
All drugs can cause side effects with many patients experiencing minor symptoms to intravenous midazolam. These are:
- Minimal cardiovascular effects
- Respiratory effects
- Hiccoughs
- Coughing
- Headaches
- Drowsiness
- Nausea and vomiting
- Loss of inhibition
- Restlessness
- Irritation at the cannula site (However, as midazolam is water soluble it is not common for the patient to experience any irritation [1,2].)
Special precautions and some contraindications of usage
Pregnancy and the nursing mother
As with all drugs, using midazolam on a pregnant patient is not recommended as it is known to slowly cross the placental barrier to enter the fetal blood. If used, it would be likely that the effects would manifest in the fetus and if used regularly in the third trimester it could lead to the baby experiencing benzodiazepine withdrawal syndrome. If a nursing mother is breastfeeding and receives treatment with intravenous sedation she would have to express enough breast milk prior to the treatment to last for 24 hours and to avoid breast feeding for the same period. If she does not undertake this the baby would receive traces of midazolam from her milk when feeding [1–3].
Kidney or liver impairment
This could slow down the rate at which midazolam is eliminated from the body resulting in prolonged and enhanced effects [1–3].
The elderly
As previously explained, elderly patients are more sensitive to the effects of midazolam. They may also metabolise and eliminate it much slower and are potentially more at risk to prolonged drowsiness, amnesia, hangover effects, confusion and accidental falls [1–3].
Children
The use of intravenous midazolam for children is not recommended as they may exhibit a paradoxical effect (i.e. agitation, involuntary movement and hyperactivity) [1].
Allergy to benzodiazepines
If a patient has a hypersensitivity to benzodiazepines, or any constituents thereof, it should not be used. In the event that this is unknown and a patient experiences a reaction, then the administration of the drug should be stopped, the patient’s airway maintained, oxygen provided and adrenaline administered. As the patient will have an indwelling cannula the intravenous concentration of adrenaline can be provided, which is 0.5ml 1:10,000. Flumazenil must never be given as it would increase the anaphylactic reaction.
Alcohol and drug abuse
Benzodiazepines should be used with extreme caution in patients who have a history of alcohol abuse as the effects of the alcohol can potentiate (speed up) the effect of the drug. There is also a risk that the patient may have liver impairment which could prolong the elimination of the midazolam. Patients with a history of drug abuse may be difficult to cannulate and thus other sites may have to be used. They may also be more difficult to sedate, requiring larger doses. As with any substance that depresses the central nervous system and/or provides any muscle-relaxant effects particular care should be taken when administering midazolam (i.e. in the case of myasthenia gravis, as these patients have pre-existing muscle weakness) [2,3].
Cardiorespiratory disorders
Effects associated with cardiovascular disorders are rare but can occur and include effects such as respiratory depression, apnoea, respiratory arrest and/or cardiac arrest. These life threatening incidents are more likely to occur in patients over 60 years of age and with those who have pre-existing respiratory insufficiency or impaired cardiac function, particularly when the injection is given too rapidly or when a high dose of midazolam is administered [1].
Analgesics and midazolam
Opiates, normally Nubain (nalbuphine), can be, but are very rarely used in conjunction with midazolam to enhance sedation effects. The use of two intravenous drugs being titrated together is known as polypharmacy. The reason it may be used is for the provision of additional post-operative pain relief for patients. However, the use of a long-acting local anaesthetic is usually sufficient and eliminates the need for their use. Nubain should be administered first as it is not titrated but given in one dose. This means that midazolam can be safely titrated on top of any sedation induced by the analgesic. Patients who receive both drugs tend to experience sleepiness, nausea and vomiting and can experience profound respiratory depression. If an emergency occured, Nubain’s reversal drug Narcan (naloxone) would be administered [3].
Erythromycin
It inhibits the metabolism of midazolam resulting in a prolonged effect [2].
St John’s wort
It enhances the metabolism of midazolam resulting in a reduced effect [2].
Potential complications
- The wrong drug administered, due to failure to check the ampoule contents, lack of drug labelling or incorrect labelling.
- Drug out of date due to the expiry date not being checked or recorded on the patient’s treatment pathway documentation.
- Allergic reaction due to patient sensitivity to the drug not being known or recorded in the patient’s notes.
- Venepuncture complication (i.e. extravasation where the cannula has been inserted into the vein and exits the other wall, meaning that when the drug is titrated a swelling like a fried egg will occur in that area). To treat this, administration of the drug should be stopped and depending upon the clini-cian the cannula will be either left or removed and if removed, pressure will be applied to the area. Bruising can occur on insertion or removal of a cannula. This is usually attributed to poor venepuncture technique upon insertion and lack of pressure being applied upon removal. Collapse of the vein during cannulation. This is difficult to overcome and is normally attributed to patient anxiety. To avoid these and other complications the right anatomical site should be chosen along with the correct size cannula and the tourniquet should be secured tightly with the chosen limb adequately restrained. It is very important that the patient is monitored and reassured and the clinician will of course be decisive regarding the success or failure of the cannula’s placement. Upon removal, pressure applied to the cannulation site must be undertaken by the clinician or second appropriate person and not the patient.
- The cannula comes out due to it not being secured properly, meaning that the continual access required to administer further increments of midazolam and more importantly for the administration of a drug or drugs should an emergency occur has been lost.
- Inadequate post-sedation supervision. The patient was not fit for discharge when they left the dental surgery or the escort either did not attend or was unsuitable. If an escort is not in attendance, treatment should be postponed.
- Over sedation, which is recognised by the patient’s chin dropping and lack of response to verbal commands [1].
Overdose of midazolam
The signs and symptoms that a patient would exhibit if they were over sedated are: Drowsiness, mental confusion, lethargy and muscle relaxation. They would not respond if they were asked a question or would not rouse if tapped on the shoulder. An overdose of midazolam should not be life threatening unless it has been combined with other central nervous system depressants, which includes alcohol. More serious signs and symptoms would be hypotension, cardiorespiratory depression, apnoea and rarely, a coma. Careful titration of midazolam, coupled with good patient management and comprehensive clinical monitoring, can prevent over sedation.
Figure 5.3 Ampoule of flumazenil.

Treatment of an overdose of midazolam
Careful observation of the patient’s vital signs is required, coupled with airway maintenance and the provision of oxygen. The benzodiazepine antagonist flumazenil (Anexate) will be used to control the effects of over sedation. This emergency drug must always be available when intravenous sedation takes place with the minimum of two vials being held. The maximum dose a patient can receive is 1mg. If necessary cardiopulmonary resuscitation will be undertaken and the emergency services called [1].
Flumazenil (Anexate)
This is a clear liquid, obtained as 500 micrograms (mcg) in a 5ml glass ampoule with the name, batch number, expiry date and quantity of drug stamped on each ampoule (Figures 5.3 and 5.4). It is the antidote for an overdose of a benzodiazepine and is an imidazobenzodiazepine derivative, which antagonises the clinical actions of benzodiazepines on the central nervous system. The pharmacology of flumazenil is that it competitively inhibits the activity at the benzodiazepine GABA receptors. This allows the neurons to return to their normal state of excitability, thus reversing the sedative effect. Flumazenil is a controlled drug, be kept under lock and key and treated as such with the ampoules being stored in the outer carton to protect them from light [1,6].
Figure 5.4 Box of flumazenil.

Administration of flumazenil
It is titrated as follows:
- 200mcg over 15 seconds.
- If required, further doses of 100mcg are repeated every minute until the desired level of consciousness has been achieved.
The maximum dose is 1mg, which is two vials. The usual dose administered is 300–600mcg [1].
Effects of flumazenil
The patient may exhibit and experience the following effects:
- Anxiety
- Disorientation
- Head pains
- Aggressiveness
- Agitation [1]
Re-sedation
Patients who have received flumazenil for the reversal of benzodiazepine effects should be monitored for re-sedation and respiratory depression for an appropriate period. This is because the half-life of flumazenil is approximately 50 minutes and the half-life of midazolam is 1–4 hours. Therefore, it is conceivable that when used to reverse the action of midazolam the patient will initially be reversed, but could become re-sedated as the action of flumazenil decreases. However, very little re-sedation will occur as both drugs will wear off together. Once broken down flumazenil is excreted in urine. Any patient who has received flumazenil to reverse the effects of midazolam must be warned that the post-operative care instructions are still applicable. They must also be kept in the surgery for a suitable period of time and be assessed for discharge before being allowed to leave the surgery [1,6].
Some contraindications of usage
Patients dependent on benzodiazepines
If patients who rely on benzodiazepine medication for medical conditions become over sedated when reversing the effects of midazolam the effects of their medication will be reversed as well.
Coronary heart disease
When treating patients who have heart conditions with midazolam their anxiety levels are reduced, thus reducing the strain placed on their heart when they are in stressful situations. If the effects of the sedation are reversed they will be placed very quickly into the situation/environment that was being avoided by sedating them. They would be very anxious and their heart rate would increase, placing unnecessary strain on it.
Epileptic patients
Patients who suffer from epilepsy are prescribed medication that belongs to the benzodiazepine family. Therefore, when the action of the midazolam is reversed so will their epileptic therapy, resulting in the patient experiencing convulsions [1].
Figure 5.5 Ampoule of propofol.

Figure 5.6 Pump driver.

Propofol (Diprivan)
Propofol is widely used in hospital settings. It is not commonly used for dental sedation in a general practice, as it is used by anaesthetists to induce and maintain patients receiving a general anaesthetic. The recovery time with its use is rapid. It provides patients with amnesic and hypnotic effects and reduces the chance of a patient vomiting. It works by enhancing the effect of GABA to depress the central nervous system without using the receptors directly. It is a white, milky liquid which is obtained in glass ampoules of 200mg in 20ml (10mg per ml) (Figure 5.6). It has a rapid onset and quick recovery with the half-life being estimated between 2 and 24 minutes and patient recovery being within 5 minutes. For dental sedation propofol is used with a patient controlled electronic infusion pump driver so that it can be continually administered (Figure 5.7). These drivers are similar to those used after general surgery for post-operative pain relief in general hospitals. The pump driver is set up by the clinician or the anaesthetist by inputting the amount of drug a patient will receive each time they press a button and the interval period between activations. This means that the patient is in control, because they hold the button throughout treatment, which when pressed will administer a dose of propofol. Due to the data input (hence the lockout time), they would not receive a dose every time they press the button. Injection of propofol can be painful — therefore, it should be administered into larger veins or following a pre-injection with a local anaesthetic. As the margin between sedation and anaesthesia is far narrower than that of midazolam, it must be remembered that when administering any general anaesthetic agent it has to be undertaken where appropriately trained staff and facilities for monitoring patients are available. Proper airway management, together with a supply of supplemental oxygen, artificial ventilation and cardiovascular resuscitation must also be available. Propofol attracts the same pre and post-operative instructions as midazolam and is a controlled drug, should be under lock and key and treated as such with the ampoules being stored in the outer carton to protect them from light [1,9].
Some contraindications of usage
Patient prescribed respiratory depressants
Propofol is potentiated by these drugs [9].
Pregnancy and the nursing mother
As with all drugs, using propofol for a pregnant patient is not recommended, as it is known to slowly cross the placental barrier to enter the fetal blood.
Patients who are allergic to eggs
Propofol is an emulsion which is dissolved in a soya-bean oil, glyceryl and purified egg — therefore, these patients would suffer an anaphylactic reaction [9].
Transmucosal (off-licence) sedation
The off-licence use of a drug means that it is being used in an alternative way to that for which it has been researched, tried and tested. This form of sedation is classed as an advanced technique, as the clinician has no control over the absorption of the drug within the body. If midazolam was />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


