Chapter 3
Role of the dental nurse and equipment
LEARNING OUTCOMES
At the end of this chapter you should have a clear understanding of:
- The importance of the role of the second appropriate person during a patient’s treatment when receiving any form of conscious sedation.
- The importance of clinical monitoring.
- The equipment used in the surgery.
INTRODUCTION
During any treatment that a patient receives the dental nurse must remain in the surgery and when any form of conscious sedation is used as an adjunct to allow patients to accept treatment it is imperative that a second appropriately trained person be present at all times. This is due to the extended role that a person has to undertake in caring for a patient during treatment. Whoever the second appropriate person is he or she must have received the proper training. In normal situations, the second appropriate person is a dental nurse, but in some clinical settings it could be another clinician. However, in some surgeries where they have numerous members of staff there could be the clinician, a nurse to assist with treatment and a nurse assigned to the conscious sedation aspect of the patient’s appointment [1].
ROLE OF THE DENTAL NURSE
When a dental nurse is the second appropriate person in the surgery assisting with patients who are receiving any form of conscious sedation their role will encompass a wide range of tasks. They will utilise many skills which have been acquired during the early stages of their basic training. The required additional knowledge and skills must have been attained by taking a recognised course in conscious sedation. Best practice and the usual pathway for a dental nurse is to take a course that leads to the National Examining Board for Dental Nurses qualification in dental sedation nursing. However, there are many very good short-term courses available through various training providers that do not lead to qualifications. Advanced training is important for the second appropriate person to help them understand their role within the team so that they do not work outside that remit and are able to recognise the areas of patient care for which they are responsible. In order for a patient to receive treatment with conscious sedation in a safe, relaxed and calm atmosphere, it is good practice for the team not only to work together on a regular basis but also to establish a routine, so that there is a good working relationship. Before a patient attends their appointment, it is important that the team prepare for their arrival so that every aspect runs as smoothly as possible. It is here that the dental nurse, acting as the second appropriate person, would start their duties and responsibilities within the patient’s treatment care plan [1].
Role of the second appropriate person when a patient is receiving treatment with conscious sedation
The second appropriate person will start by preparing the surgery, ensuring that it is disinfected and identifying primary and secondary zones. They will also ensure that all instruments for the procedure are sterilised and all materials and medicaments are prepared. They will prepare the appropriate equipment to reflect the type of sedation the patient is to receive, along with all the equipment required to undertake the medical checks and monitoring equipment. They will collect the patient’s dental notes and radiographs and ensure that a signed consent form has been completed. They will, at some stage, read the patient’s notes, paying particular attention to the medical history to make themselves aware of the patient’s medical status and be prepared for an emergency, should one arise. They will refer to any previous treatments that the patient has undergone with conscious sedation to establish if there were any complications experienced during the treatment and recovery stages. They will also be aware of the amount of sedation the patient received. Keeping good, contemporaneous notes is vital for the team’s reference purposes. These notes provide a history of the patient’s treatment with the use of conscious sedation and allow modifications to be made at future appointments reflecting any written comments. A very important role before any conscious sedation treatment takes place is to ensure that the medical emergency equipment is present and functional by checking the drug expiry dates, ensuring that the oxygen cylinder content is sufficient and that portable suction is present. If intravenous sedation is being administered, the reversal drug flumazenil must be available. If inhalation sedation is being administered, it is important to ensure that the machine is safe to use, the scavenging system is attached and that there is good ventilation within the surgery [1].
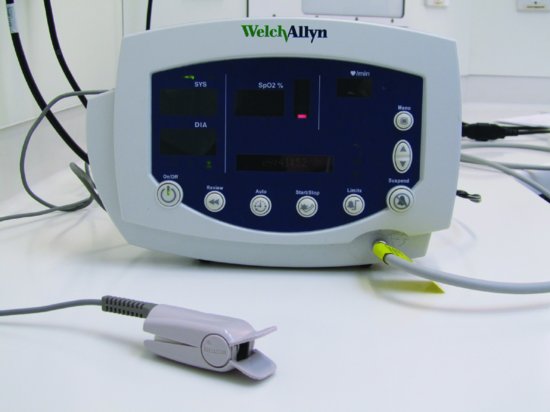
Figure 3.1 Pulse oximeter.
INTRAVENOUS SEDATION
Role of the second appropriate person before a patient receives treatment
Once the surgery is prepared to receive a patient, the second appropriate person can greet them, introduce themselves and take them into the surgery, or preferably into a separate room, in order to undertake the medical checks required to ensure that the patient is fit to undergo treatment using conscious sedation. Upon entering the room, they will ask the patient and the patient’s escort to take a seat while taking care of the patient’s belongings. They will have previously prepared a blood pressure machine, pulse oximeter (Figure 3.1), weighing scales, if required, and a method of documentation to record the patient’s response to mandatory questions, ensuring that they have and will comply with the pre and post-operative instructions. Some dental practices formulate a pro-forma that they can use as documentation to record the patient’s treatment pathway from start to finish, whereas other practices may record this information in the patient’s notes. It is a good idea to request that the patient’s escort accompanies them at this stage so that it can be established whether after care for the patient will be adequate. This reinforces the importance of the role of the escort and the post-operative instructions that were provided at the assessment appointment. Once the patient and the escort are seated the second appropriate person should inform the patient that they will be looking after them during their treatment. They should commence by asking the patient the following questions:
Figure 3.2 Pulse being taken.

- Are you normally fit and healthy?
- How do you feel today?
- Has your medical history changed since the assessment appointment?
- Has any of your medication changed since the assessment appointment?
- Have you recently visited the doctor?
- Have you any allergies?
- When did you last have any food or drink?
- Have you had any alcohol today?
- What arrangements have been made for you to travel home?
- Who will be looking after you at home?
- When are you planning to go back to work?
Figure 3.3 Blood pressure being taken.

Figure 3.4 (a) Patient with pulse oximeter attached to finger. (b) Pulse oximeter monitor.

Once these questions have been answered and documented it is important to clarify with the patient’s escort some of the answers given, in respect of after care. Record their name and take their mobile telephone number so that if they decide to leave the premises for the appointment duration they can be contacted. Once satisfied that the patient will be properly cared for at home the second appropriate person will take the patient’s pulse rate (Figure 3.2), respiratory rate, blood pressure (Figure 3.3), oxygen percentage saturation levels (Figures 3.4a and b) and weight, if required, and document them. They will then present the readings to the clinician who will also act as the sedationist. It is useful to take the patient’s pulse manually as this provides the rate per minute, the quality and strength of the pulse and whether it is irregular. This information is useful when monitoring a patient during treatment to identify any changes in the status and in particular when dealing with and diagnosing an emergency for comparison. They will note the colour of the patient’s skin, their demeanour and whether they have false nails or are wearing nail varnish. If they are the varnish must be removed to prevent interference with the pulse oximeter readings or another site selected (i.e. a toe). Finally, the second appropriate person will ask the patient if they have any questions, answer them accordingly and if necessary explain the procedure for both the mode of sedation and the treatment being provided. A stop signal will also be arranged. Once this pre-assessment stage is complete, the second appropriate person will ask the escort to take a seat in the waiting room, advising them of the approximate length of treatment [1].
Role of the second appropriate person during patient treatment
The second appropriate person will ensure that the patient is seated comfortably in the dental chair and request their permission to apply personal protective equipment. They will, if necessary, introduce them to the clinician and wait attentively until the clinician is ready to commence. When all aspects of the appointment that the clinician wishes to discuss with the patient are com-plete, treatment will begin. Depending upon the sedation being used the role of the second appropriate person will differ slightly and this will be explained as the chapter progresses. For any sedation being provided the following role of the second appropriate person will apply:
- They will check whether a signed consent form is present.
- They will ensure that the patient has followed all pre-operative instructions relevant for the type of sedation they are to receive.
- They will act as a chaperone to both the patient and the clinician, irrespective of gender, so that if the patient had reason to believe that the clinician had acted inappropriately the second appropriate person will be able to vouch that this was not the case. Accusations can occasionally occur as the drug administered for intravenous sedation can lead to the patient experiencing dreams/hallucinations.
- They will aid the clinician in the clinical and electrical monitoring of a patient’s vital signs, alert the clinician to any changes and respond accordingly. Monitoring should commence from the point the patient came into contact with the second appropriate person.
- They will assist with the procedure.
- They will reassure the patient throughout treatment.
- They will respond and assist the clinician in the event of an emergency.
- They will assist with the recovery of the patient. Some clinicians may decide to place this responsibility upon the second appropriate person. In this instance the clinician will remain on the premises.
- They will assist when assessing the patient for discharge.
- If the clinician decides that it is in order the second appropriate person may be requested to provide verbal post-operative instructions to the patient and escort, relevant to the mode of sedation received, the procedure undertaken and to furbish the patient and escort with written instructions for reinforcement.
- They may have to book a follow-up appointment.
- They will take the payment for the treatment and the method of sedation provided.
- Throughout the appointment they will practice excellent cross infection control, ensuring the health and safety of all, maintain the patient’s diversity, dignity/rights and uphold the confidentiality of the patient.
Role of the second appropriate person while a patient is receiving treatment
Before the patient’s treatment can commence they have to be prepared for cannulation. A simple explanation is given, advising them that its use is mandatory in order that the drug being used to sedate them can be administered. Discussions should be held with the patient as to whether they have any preference for the site of the cannula. The normal sites used are the antecubital fossa, the inner surface of the elbow or the back of the hand, known as the dorsum. They are advised that on insertion they will feel a small, sharp scratch and once inserted the cannula will be taped into place and tested to ensure that it has been correctly inserted by administering a solution (sodium chloride). Once successful cannulation is achieved the patient is told that the drug will then be administered. They will start to feel more relaxed and consequently less anxious.
Role of the second appropriate person during cannulation
The second appropriate person will have already prepared the following items for cannulation and administration of the sedation drug:
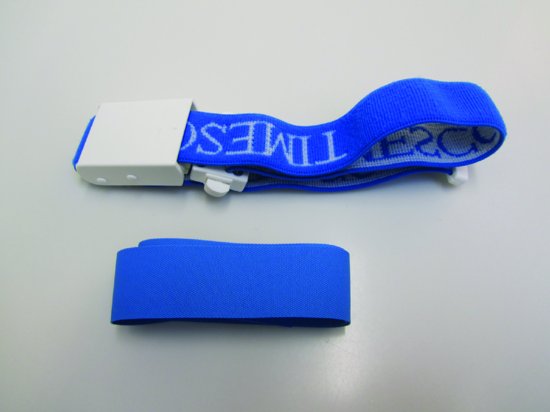
- A tourniquet (Figure 3.5). To restrict the venous return, thus engorging the vein so that cannulation can take place.
Figure 3.5 A non-disposable and disposable tourniquet.
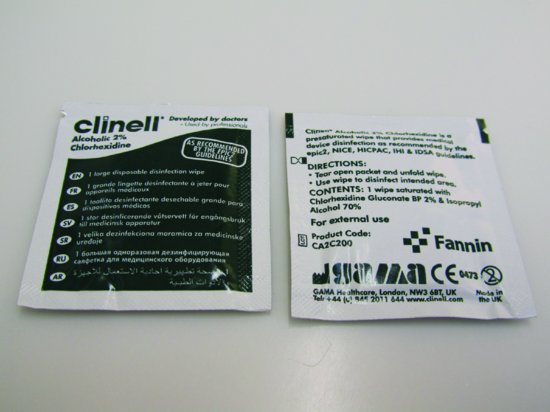
- A disinfectant surface medi-wipe (Figure 3.6). To cleanse the selected cannulation site. This must be allowed to dry prior to inserting the cannula, because medi-wipes contain alcohol which on insertion of the cannula will be taken into the vein and the patient will experience a stinging sensation. It is also not acceptable, once the cannulation site has been disinfected, for the area to be tapped to increase the engorgement of the vein as this would result in potential cross contamination and possible infection at the cannulation site. If this action is undertaken, then a new medi-wipe should be used.
Figure 3.6 A medi-wipe.
- A cannula, either a 22-gauge Venflon (Figure 3.7), a Y-can (Figure 3.8) or a 23-gauge butterfly needle (Figure 3.9). To gain access into the vein, which, once sited, is known as an indwelling cannula in order to administer the drug. When placing a cannula the clinician will not probe, but be decisive. Probing can be very painful for the patient. Best and modern-day practice is to use a Venflon or a Y-can.
Figure 3.7 22-gauge Venflon.

Figure 3.8 Y-can. (From Hollins, C. (2008) Levison’s Textbook for Dental Nurses, 10th edn. Reproduced with permission from John Wiley & Sons.)
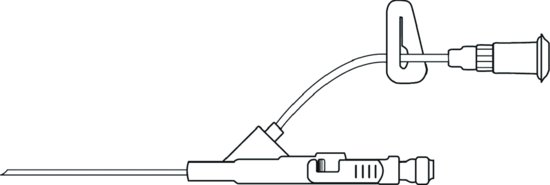
Figure 3.9 23-gauge butterfly needle.

- Two 23-gauge drawing-up needles (Figure 3.10). One to draw the drug into a sterile syringe and the other to draw the flush into a sterile syringe. There are other available sizes of drawing-up needles, with the 23-gauge needle being the ideal choice as it is a filter needle, which means that it will filter any potential minute particles of glass that may have dropped into the glass ampoule. This prevents such particles from being drawn into the sterile syringe and being administered to the patient. The length of the needle means that it will reach the bottom of the glass ampoule drawing the entire drug into the syringe.
Figure 3.10 23-gauge drawing-up needle.

Figure 3.11 5ml sodium chloride flush.

- A 5ml sodium chloride flush (Figure 3.11). To administer when the cannula is in place after ensuring that it has been sited properly. Sodium chloride is used, because it is compatible with the body. If cannulation has been unsuccessful it will not cause damage to the internal tissues as it disperses. Some clinicians may not use a flush after cannulation to check that it has been sited correctly. This means that as they administer the drug, given that cannulation has failed, the drug would disperse into the internal tissues. As a result, they have to estimate how much of the drug dispersed into the tissues and take this into account when titrating the remainder of the drug, because the dispersed drug will eventually act upon the patient’s body. If cannulation is unsuccessful it may be left in situ. This, of course, is at the clinician’s discretion. Another cannula will be required and another site selected.
- A 2ml sterile syringe with a sodium chloride label placed (Figure 3.12). This is to contain the flush used to ensure that the cannula is sited correctly.
Figure 3.12 Sterile syringe with sodium chloride label.

- A 5ml sterile syringe with a drug label (midazolam) placed (Figure 3.13). This is to contain the drug prior to administration.
Figure 3.13 Sterile syringe with midazolam label.

- The sedation drug to be used, midazolam (Figure 3.14). To sedate the patient.
Figure 3.14 Ampoule of midazolam.

The second appropriate person will also have ensured that the reversal drug flumazenil is available, together with a 5ml sterile syringe and a 23-gauge drawing-up needle (Figure 3.15), which should be drawn up and administered to a patient only in the event of over sedation. This constitutes an emergency. The reversal drug must only be titrated to a patient during an emergency after all other basic assessments, airway management and the administration of oxygen have failed. It is not acceptable to use it as a means of reversing the action of the sedation drug, so that the patient can be discharged more quickly in order to shorten the appointment time.
Figure 3.15 Ampoule of flumazenil, a 5ml syringe and a 23-gauge drawing-up needle.

When a patient is having a cannula placed, the second appropriate person will undertake the following duties:
- They must ensure that the patient is seated comfortably and that the chair is placed in a high position, with the back semi-supine. This allows the drainage of blood into the cannulation site when the arm is lowered and in the event of a patient feeling faint they are already semi-supine.
- If required they will aid the clinician in locating a suitable vein to place the cannula and if the patient has cold hands they must provide a source of heat such as a jug of warm water. The cannulation will then be easier, as warm hands provide better visibility of the patient’s veins, because they will engorge, as opposed to cold hands where the veins become more difficult to locate.
- They may have to pass the tourniquet to the clinician. Some clinicians may request that the second appropriate person applies a tourniquet (Figures 3.16 and 3.17). Some clinicians do not use tourniquets. Instead, they request that the second appropriate person places both hands around the patient’s arm to apply pressure (Figure 3.18), thereby providing the same function as a tourniquet.
Figure 3.16 Tourniquet placed on antecubital fossa.

Figure 3.17 Tourniquet placed on lower arm.

Figure 3.18 Lower arm being held to engorge vein.

- Once the veins are engorged they will pass the medi-wipe to the clinician and when it has been used accept it in exchange for the cannula.
- When the cannula is being inserted (Figure 3.19) it is important that the patient is put at ease. The second appropriate person should talk to the patient and remind them that they will feel a sharp scratch as the cannula is being inserted. This is so that the patient does not jump on insertion. A back flash of blood will appear within the cannula giving an indication that it has been inserted into the vein (Figure 3.20). However, this indication is not a guarantee of successful cannulation. The second appropriate person should also make small talk to occupy the patient, taking their thoughts away from the placement, as most patients find this part of their treatment unpleasant.
Figure 3.19 Placement of a 22-gauge cannula.

Figure 3.20 Blood flash back.

- Once the cannula has been inserted they may be requested to apply pressure at the point (Figure 3.21) of entry to restrict blood flow while the clinician removes the introducing needle. The clinician will then remove the end cap, place it onto the cannula where the introducing needle was removed (Figure 3.22). This is known as the luer lock (Figure 3.23). Some clinicians request patients to raise their arm when removing the introducing needle in order to place the cap. This should prevent blood flow from the area.
Figure 3.21 Pressure applied to cannula to prevent blood leakage.

Figure 3.22 Cap placed onto luer lock.

Figure 3.23 The luer lock.

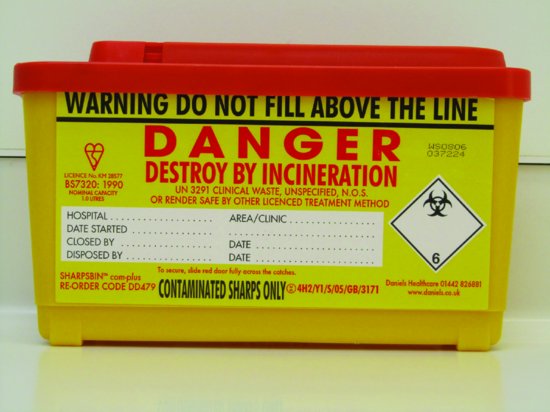
- They must have a sharps bin (Figure 3.24) at hand for the clinician to place the used introducing needle.
Figure 3.24 A sharps bin.
- The second appropriate person may be requested to remove the tourniquet.
- The 2ml sterile labelled syringe, previously drawn up by the clinician, containing the sodium chloride flush will be passed to the clinician, stating the contents of the syringe. The batch number and the expiry date should have already been checked with the clinician and documented using the method of recording a patient’s treatment pathway.
- As the sodium chloride flush is being administered the cannulation site should be observed ensuring its correct position. If swelling appears it will be an indication that the sodium chloride flush has dispersed into the surrounding tissues and that the cannula has pierced the vein wall. The raised area will look somewhat like a fried egg. The second appropriate person should inform the patient that they will experience a cold sensation travelling up their arm and that there should be no pain. Any failed cannulation must be recorded on/in the documentation of the patient’s treatment pathway, along with the successful cannulation, recording the size of the cannula and the site used.
- Once it has been established that cannulation has been successful they will secure the cannula with either non-allergenic tape or a Venflon dressing, taking care not to pull the cannula out of the vein wall.
- They will place the pulse oximeter probe onto the patient’s finger, explaining the reason for its use. They will have previously set the pulse and oxygen saturation level warning alarms that are incorporated in the pulse oximeter to suit the physiology of the patient.
- They will now pass the 5ml sterile, labelled syringe, containing the sedation drug to the clinician previously drawn up by him/her, stating its contents. Once again, the batch number and the expiry date should have been checked with the clinician and documented using the method of recording a patient’s treatment pathway.
- When the sedation drug is titrated to the patient, against their response, the second appropriate person should continue talking to the patient, as their speech is a good indication of when the drug is taking effect. They will start to slur words, with their response to questions being slower. The second appropriate person may be expected to advise the patient what they may experience and ask them how they are feeling. To establish if sedation is sufficient they may ask the patient to extend an arm and touch their nose. This action is known as the Eve sign. This tests the patient’s coordination. If they can touch their nose they are classed as Eve sign negative and they are not adequately sedated. If they cannot find their nose or carry out the task slowly then they are Eve sign positive and are adequately sedated. Other factors need to be taken into account to establish whether the patient is adequately sedated. Observance of their general demeanour, their vital signs and level of consciousness or any adverse reactions must also be looked for. Continue to praise and reassure the patient.
- During the administration of the drug, they will record, once again using the method of documenting the patient’s treatment, the initial bolus and any incremental titrations of the drug given. It is important to make a note of the time. The patient’s percentage of saturated oxygen and pulse must also be recorded, along with a brief statement of the patient’s response — for example, if the patient is still responsive – Eve sign negative — or if the patient is relaxed with slurred speech – Eve sign positive.
Once the patient is relaxed and cooperative, possibly sleepy but still conscious and the clinician deems them to be nicely sedated, the treatment can commence.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


