Chapter 6
Medical emergencies
LEARNING OUTCOMES
At the end of this chapter you will have a clear understanding of:
- Recognising the signs and symptoms of common emergencies that could occur in the dental surgery.
- Managing these conditions efficiently.
- Reducing the risk of an emergency in the surgery.
INTRODUCTION
Any patient could suffer an emergency while undergoing treatment in the surgery. Life threatening emergencies are rare, but they can happen and the team must be prepared to manage any condition that occurs. For the team to be able to manage any and all emergencies they must seek the appropriate training in medical emergencies and resuscitation. A dental practice can, in conjunction with training, implement various mechanisms to reduce the risk of an emergency, which is naturally preferable to having to deal with one [1].
PREVENTION OF MEDICAL EMERGENCIES
Prevention is much better than having to deal with a patient who is experiencing an emergency, as it is stressful and disturbing not only for the patient but also for the team, even if the patient does make a full recovery. To reduce the risk of an emergency within the surgery the following points should be implemented as they are deemed to be good practice [1]:
- All staff, including the receptionist, should undertake regular training and attend updates in emergency situations and resuscitation to ensure that their knowledge and skills are in line with the current resuscitation council (UK) guidelines.
- Medical emergency simulations are extremely valuable as they allow the team to implement their knowledge and practice their skills in a controlled environment without compromising a patient’s health. When undertaken, all participants should discuss the activity to establish if the simulation went well and if not how it could be improved should it ever occur in a real-life situation.
- All staff should understand their role during an emergency. The normal situa-tion is for the nurse to obtain the emergency drugs/equipment and to assist the clinician as directed, while the receptionist alerts the emergency services. However, if the nurse is the first person on the scene, then he/she should administer first-line treatment to the patient and give clear instructions to others while waiting for the dentist and/or the emergency services arrival so that the patient’s condition hopefully remains stable.
- Careful assessment and good patient management can prevent emergencies. Updating a patient’s medical history every time they visit the dental practice would establish if there has been any change in their condition or medication since their last visit. All the team should be encouraged to look at a patient’s medical history to make themselves aware of any condition/s that the patient may suffer. In this way they can prepare for any eventuality and plan how they would assist the clinician to facilitate the patient’s recovery. If a dental nurse is aware of a patient’s medical condition they can request that the patient places their medication on the work surface for easy access. By taking/updating a medical history from a patient a clinician can establish the patient’s medical fitness. They can evaluate the information discussed and decide whether the patient would be better managed within a hospital setting. The method commonly used is the American Society of Anaesthesiologists’ (ASA’s) classification of medical fitness as explained in Chapter 4.
- It is imperative to monitor the patient’s vital signs during and after treatment, with monitoring commencing as soon as they enter the practice, with any concerns being relayed to the clinician.
- Emergency drugs and equipment should be easily accessible. A daily check should be undertaken to ensure that all drugs are in date and that emergency equipment is functional. Any drugs due to expire must be ordered immediately, with any that are out of date being replaced. These checks should be fully documented to avoid any confusion which could lead to a serious failure. All emergency equipment must be serviced at recommended intervals with all documentation being kept. All staff should be aware of the contents of the emergency drugs box and know which medication is used for any/each arising condition. Audits of these activities should take place on a regular basis.
- Recording any incidents in the patient’s notes is a reminder to yourself and is informative to others who may treat the patient in the future so that you and they can be prepared for the eventuality should it reoccur.
- Postponing treatment should be considered if it is identified that the patient is unwell, allowing him or her time to recover and, if needed, seek the necessary appropriate medical attention.
- Scheduling appointments to suit the patient’s medical condition can help to prevent problems occurring. For example, if a patient is diabetic (type 1 or 2) then an appointment just after a meal is preferable as they will have eaten and their blood sugar would not be low, thereby decreasing the risk of them experiencing a hypoglycaemic episode.
- Risk assessments to look at the ergonomics of the practice to establish any difficulties you might encounter should an emergency arise.
LEGAL ASPECTS DEALING WITH MEDICAL EMERGENCIES
Dental professionals have a duty of care to patients and are expected to deal with any emergency that occurs in the surgery. The implication of any action taken irrespective of the outcome doesn’t mean that they were negligent.
DEALING WITH MEDICAL EMERGENCIES
Two mistakes are most common in the management of emergencies. The first is to attempt to do too much and the second doing too little — therefore team effort is important. This ensures that everything that could possibly be done to aid patient recovery is carried out and that nothing is missed [1].
Control of medical emergencies
- When an emergency occurs in the surgery the team need to assess their surroundings to ensure not only the patient’s safety, but also their own, because if they injure themselves they will not be able to aid the patient. This is a common mistake which could lead to unnecessary accidents occurring due to the team being in familiar surroundings and possibly forgetting to check for hazards [1].
- The patient’s general condition and vital signs should be assessed to determine the preliminary diagnosis, which is not always the definitive one. Continual monitoring is essential to recognise any changes in the patient’s medical status, which can then be acted upon accordingly. It is important to check for any injuries that the patient may have sustained so that first aid can be administered promptly. Should an injury occur the team should prioritise and deal with whichever is more life threatening [1].
- Whenever a patient collapses and it is realised that an emergency has occurred help should always be called for. You should never attempt to cope on your own, because help that could possibly be more experienced could take the lead and request that you support them as they direct or if this is not the case take instructions from you. For example, they could call the emergency services and fetch the appropriate drugs, oxygen and masks [1].
Emergency drugs box and equipment
For a dental practice to manage the emergencies that can occur in the surgery they should have an easily identifiable area/box/trolley housing the recommended drugs and equipment required [1].
Drugs
- Adrenaline (1:1000 1mg/ml) (Figure 6.1)
Figure 6.1 Adrenaline (1:1000 1mg/ml).

- Aspirin, dispersible (300mg) (Figure 6.2)
Figure 6.2 Aspirin (300mg).

- Glucagon (1mg) (Figure 6.3)
Figure 6.3 Glucagon (1mg).

- Glyceryl trinitrate (GTN) spray (400mcg per dose) (Figure 6.4)
Figure 6.4 Glyceryl trinitrate spray (400mcg per dose).

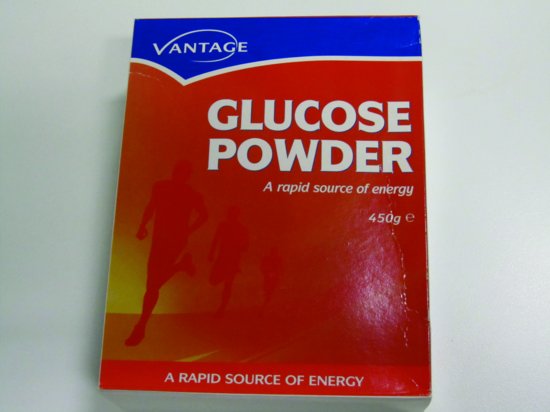
Figure 6.5 Oral glucose.
- Midazolam (5mg/ml or 10mg/ml, buccal or intranasal)
- Oral glucose/tablets/gel/powder (Figure 6.5)
- Oxygen (D size with a pressure reduction valve and flow meter) (Figure 6.6)
Figure 6.6 CD size oxygen cylinder.

Figure 6.7 Salbutamol inhaler (100mcg per dose).

- Salbutamol (100mcg per dose) (Figure 6.7) [1,8]
Where possible any drugs in a solution should be drawn into a pre-filled syringe, saving time and making them easier to administer. As intramuscular, inhalation, sublingual, buccal and nasal routes of drug administration are faster in an emergency they should be the preferred routes to use, with the intravenous route of drugs being discouraged within a general practice setting. Portable oxygen cylinders should be of a suitable size to enable them to be carried, as well as containing sufficient oxygen to allow enough oxygen delivery to patients at an adequate flow rate, for example 10–15L/min, until the arrival of the emergency services or until the patient fully recovers. A full ‘D’ size oxygen cylinder contains 340L of oxygen and if administered to a patient at a flow rate of 10–15L/min it will provide up to 20–30 minutes of oxygen. It may be necessary to have two cylinders within the practice to ensure that the supply of oxygen does not fail when it is used during an emergency [1].
Equipment
Where possible all emergency medical equipment within the practice should be latex free and single use only [1]:
- Different size oxygen face masks with tubing.
- Size 1, 2, 3 and 4 oropharyngeal airways (Figure 6.8).
Figure 6.8 Size 1, 2, 3 and 4 oropharyngeal airways.

- Pocket mask with an oxygen port (Figure 6.9).
- A self-inflating bag and mask with an oxygen reservoir bag and tubing (Figure 6.10) with different size masks to accommodate both paediatric and adult patients. If staff members have been appropriately trained to use them a 1L bag should be stocked.
- Portable suction (Figure 6.11) with suction catheters and tubing. A Yankauer sucker (Figure 6.12) would be an ideal suction tip to hold.
- Different size, single-use sterile syringes and needles (Figure 6.13).
- A large volume spacer device for inhaled bronchodilators (Figure 6.14).
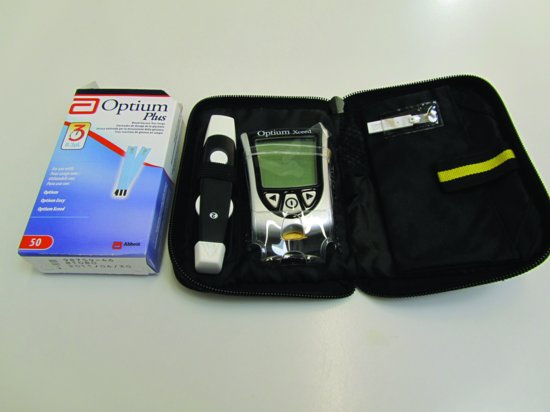
- A blood glucose monitoring measurement kit (Figure 6.15).
- Automated external defibrillator (AED) (Figure 6.16).
AEDs are expected to be available in a dental practice as they require very little training to use them safely and they reduce mortality rates from cardiac arrest. All staff should be familiar with the device they have in their practice and they do not have to be trained to use one. However, training will increase the effectiveness of its use, improving the speed at which the pads are placed
Figure 6.9 Pocket mask with an oxygen port.

Figure 6.10 Self-inflating bag and mask with an oxygen reservoir bag and tubing with different size masks.

Figure 6.11 Portable suction.

Figure 6.12 A Yankauer sucker.

Figure 6.13 Different size, single-use sterile syringes and needles.

Figure 6.14 Large volume spacer device.
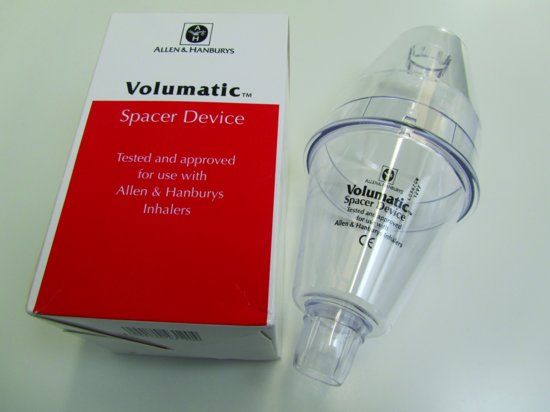
Figure 6.15 Blood glucose monitoring measurement kit.
and the shock delivery time. A defibrillator should have recording facilities built in and standardised consumables such as self-adhesive pads and connecting cables [1].
Figure 6.16 AED.

COMMON MEDICAL EMERGENCIES
Common emergencies that can occur in the dental practice are as follows:
- Adrenal insufficiency
- Asthma
- Anaphylaxis
- Cardiac emergencies
- Choking and aspiration
- Epileptic seizures
- Hypoglycaemia
- Syncope (faint)
Asthma, angina, myocardial infarct, respiratory arrest, choking and aspiration can be categorised as conditions involving breathing difficulties and/or chest pain. Epilepsy and hypoglycaemia are conditions associated with fits. Anaphylaxis, adrenal insufficiency, faint and cardiac arrest are all conditions involving loss of consciousness [1].
SIGNS AND SYMPTOMS OF MEDICAL EMERGENCIES
A sign is an indication that the patient is experiencing an emergency, as it would be observed, whereas a symptom is something the patient would experience enabling them, if it was a regular occurrence, to recognise that the condition was imminent.
MEDICAL EMERGENCIES
Adrenal insufficiency
Any patient who has been taking corticosteroids for any length of time, or has stopped taking them, can suffer adrenal insufficiency due to physiological stress, as this results in hypotension. As patients can become anxious at the thought of and actually receiving treatment there is a possibility that they may collapse because of this insufficiency. It is possible that routine dental treatment does not affect them so other reasons should not be ruled out when an assessment is made. A few patients have warning cards and by updating a patient’s medical history it can be established whether they would require a prophylactic administration of steroids prior to treatment to prevent its occurrence [1,4,8].
Signs and symptoms of adrenal insufficiency
- Pale.
- A fall in blood pressure.
- A rapid loss of consciousness.
- Low blood glucose levels [1,4,8].
Management of adrenal insufficiency
- Patients should be laid flat with their legs higher than their head.
- Oxygen administered at 10–15L/min.
- Emergency services called.
- Monitored and reassured.
- Hydrocortisone administered [1,4,8].
Asthma attack
Asthma is a very common condition, which many sufferers make light of despite it affecting a large number of the population. However, it must be remembered that it can be life threatening. It is a chest condition which occurs due to narrowing of the airways where the lining of the walls swell and become inflamed. Occasionally sticky mucus and phlegm can attach to the airways making the tubes even narrower. Asthma attacks can occur because of stress, emotion, anxiety, exercise, being exposed to an allergen, colds or chest infections and laughter. Many people with asthma suffer from eczema and hay fever, with their condition being worsened during the hay fever season [1,5,8].
Signs and symptoms of an asthma attack
- Breathlessness.
- Inability to complete a sentence.
- Wheezing on exhalation.
- Accessory muscles of respiration in action.
- Increased respiratory rate (more than 25 per minute).
- Tachycardia, a fast pulse rate (more than 110 per minute).
- Anxiety [1,6].
Life threatening signs and symptoms
- Bradycardia, a slow pulse rate (less than 8 per minute).
- Decreased respiratory rate (less than 50 per minute).
- Cyanosis, blueness of the lips and/or extremities.
- Exhaustion, confusion and a decreased level of consciousness [1].
Management of an asthma attack
- Reassure the patient and sit them up. Do not lay the patient flat as this will increase their breathlessness.
- Patients normally carry their salbutamol (ventolin) inhaler (100mcg per activation) with them. They should be encouraged to take a few activations as this is usually all that is required. If they do not have their medication with them obtain it from the emergency drugs box. To eliminate the spread of infections the inhaler can be either given to the patient or discarded in the waste drugs box to be disposed of in the normal way.
- If a patient is unable to use their inhaler effectively, then additional doses should be given through a large volume spacer device.
- Call the emergency services if the patient does not improve or they exhibit life threatening signs and symptoms.
- If the patient’s nebuliser is unavailable a large volume spacer device should be used with 4–6 activations of salbutamol being given and repeated every 10 minutes, as needed, until the emergency services arrive.
- While waiting for the emergency services maintain a patient’s airway and administer oxygen at 10–15L/min.
- If a patient becomes unresponsive you should check for breathing and signs of life and if necessary undertake cardiopulmonary resuscitation, ignoring the occasional gasp.
- At all times patients must be monitored and reassured.
Any sick, cyanosed patient with respiratory difficulty should be administered a high flow of oxygen until the ambulance arrives as this is of benefit to them, even in the case of a patient who has chronic obstructive pulmonary disease. The benefit would outweigh any risks of causing respiratory depression [1].
Anaphylaxis
An anaphylactic shock is a type of hypersensitive reaction to otherwise unknown antigen (i.e. antibiotics, nuts). In dentistry, anaphylactic reactions may follow the administration of a drug or exposure to latex. It is caused by the release of histamine following an exposure to an antigen in a person who has previously been sensitised to that allergen. Anaphylactic reactions can also be attributed to additives and recipients in medicines, so it is vital to check the full contents of any which may contain fats and oils. Generally the more rapid the onset of the anaphylactic reaction the more serious the condition will be [1,8].
Signs and symptoms of anaphylaxis
Symptoms of an anaphylactic reaction can develop within minutes of exposure and early, effective management of this condition could be life saving. Unfortunately, as there are a huge range of possible signs and symptoms it can make the condition very difficult to diagnose:
- Urticaria (an itchy skin eruption which is characterised by weals that have pale interiors with well-defined red margins).
- Rhinitis (an inflammation of the mucous membrane lining the nose).
- Conjunctivitis (inflammation of the conjunctiva of the eye).
- Nausea, vomiting, diarrhoea and abdominal pains.
- Patients experience a sense of unease and impending doom.
- Flushing is very common — however a pale complexion may also occur.
- Marked upper airway (laryngeal).
- Oedema (swelling) of the tongue and upper airway.
- Bronchospasms may develop, causing strider (a whistling noise on inspiration and wheezing).
- Peripheral coldness and cold clammy skin.
- Rapid/weak impalpable pulse, tachycardia with a rapid drop in blood pressure.
- Vasodilation leading to a drop in the blood pressure and collapse.
- Respiratory arrest (breathing has stopped, but circulation is still present).
- Loss of consciousness and cardiac arrest [1,8].
Management of anaphylaxis
First-line treatment
- Remove the item that has caused the reaction and if a drug was being administered stop its use immediately.
- Immediately place the patient in the supine position to restore their blood pressure.
- Maintain the patient’s airway and administer oxygen at 10–15L/min [1,8].
Severe reaction
- Call the emergency services.
- A semi-conscious patient or one presenting severe bronchospasms and a widespread rash should have a 0.5ml adrenaline injection 1:1000 administered intramuscularly (IM) in either their outer arm or thigh.
- An auto-injector (epipen) preparation of adrenaline is available as a 0.3ml injection, 1:1000 for self-administration by a patient who is aware that they will have a severe reaction. If the patient has his/her epipen and it is immediately available then it is acceptable to use it.
- The dose of adrenaline should be repeated every 5 minutes according to the patient’s blood pressure, respiratory and pulse rates.
- At all times monitor and reassure the patient.
- If the patient loses consciousness they should be assessed for signs of life and breathing and, if necessary, undertake cardiopulmonary resuscitation, ignoring the occasional gasp.
- All patients should be transferred to hospital for further assessment, irrespective of their initial recovery.
- An antihistamine drug, chlorpheniramine maleate (Piriton) and steroid, hydrocortisone succinate (Solu-cortef) are useful in the management of an allergic reaction but they are not first-line drugs and will be administered by the emergency services if necessary [1,8].
Children
The dose of intramuscular adrenaline 1:1000 is based on the approximate age of the child or their weight:
- 12 years – 500mcg IM (0.5ml)
- If child is small or pre-pubertal – 250mcg
- 6–12 years – 250mcg IM (0.25ml)
- 6 months to 6 years – 120mcg IM (0.12ml)
- 6 months –50mcg (0.05ml)
Less severe cases and asthma sufferers
- Any patient wheezing or experiencing difficulty breathing can be treated with a few activations of a salbutamol inhaler and if necessary a large volume spacer device can be used with 4–6 activations of salbutamol being administered. This can be repeated every 10 minutes until the emergency services arrive.
- If the patient shows signs and symptoms that are life threatening then intramuscular adrenaline can be administered [1].
CARDIAC EMERGENCIES
Cardiac emergencies cover a range of conditions. These are:
- Angina pectoris
- Myocardial infarct
- Cardiac arrest
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


