Chapter 2
Medico-legal aspects of dental sedation
LEARNING OUTCOMES
At the end of this chapter you should have a clear understanding of:
- The legislation associated with the provision of dental sedation.
- The importance of the consent process.
INTRODUCTION
Law and ethics within dentistry are very interesting, but dry, subjects that quite naturally go hand in hand. However, this aspect must be taken seriously in order to provide safe, effective treatment and to avoid patient complaints. The General Dental Council (GDC) regulates the practice of dentistry to protect patients. They publish various booklets (Figures 2.1a–f), one of which gives guidance on the principles of good practice. These booklets address legal and ethical issues that the dental team may face on a day-to-day basis, providing an overview of what is expected to prevent such issues occurring. A couple of paragraphs within the Standards for Dental Professionals booklet deal with conscious sedation, where the GDC state they support letters of advice from Chief Dental Officers, guidance and recommendations of two publications for the practice of dental sedation and that they expect the dental team to implement these when treating patients with sedation. These documents are:
- A Conscious Decision published in July 2000 by the Department of Health (DH), known as a review of the use of general anaesthesia and conscious sedation in primary dental care.
Figure 2.1 (a) General Dental Council’s (GDC’s) Principles of Patient Consent. (b) GDC’s Principles of Patient Confidentiality. (c) GDC’s Principles of Complaints Handling. (d) GDC’s Principles of Raising Concerns. (e) GDC’s Principles of Dental Team Working. (f) GDC’s Standards for Dental Professionals. (Reproduced with kind permission from the General Dental Council. Information correct at the time of going to press. Please visit the GDC website to check for any changes since publication: www.gdc-uk.org.)
- Conscious Sedation in the Provision of Dental Care published in November 2003 by the Standing Dental Advisory Committee who are recognised experts within the field of dental sedation. This document was requested by DH [1,2].
RECOMMENDATIONS CURRENTLY IN PLACE WHEN PROVIDING DENTAL SEDATION
As pain and anxiety control are integral parts of dentistry, guidelines are in place for clinicians practising dental sedation techniques. These guidelines highlight the appropriate use of techniques and best practice reflecting the current definition of conscious sedation [1–3]. They state:
- The provision of sedation avoids a general anaesthetic for treatment of patients who have anxiety and/or phobia and for patients who are happy to attend but require a more complex procedure. The clinician will justify each provision of sedation, ensuring that the technique employed is relevant for the patient’s medical, dental and social history and that the dental procedure to be undertaken will reduce the patient’s anxiety levels without being too invasive. This is established by a thorough patient assessment with consent taken from the patient for the intended treatment. Ideally, only those patients who come under the American Society of Anaestheologists (ASA) I and II Medical Fitness Classification should be treated in the dental surgery (explained in Chapter 4). The clinician will, of course, know that the mainstay of pain and anxiety control is local anaesthesia and this must be the starting point before providing any sedation technique. They will also know that on occasions one sedation technique may not be successful and that they may have to adopt two techniques (i.e. a needle-phobic patient could be administered inhalation sedation to allow cannulation to take place). However, if the clinician chooses to adopt this approach, they would accordingly take into account the drug combination of the two [1–3].
- Most patients are suitable and conducive to intravenous, inhalation and oral sedation as adjuncts to aid them in the acceptance of treatment. The use of off-licence sedation in oral, intranasal and transmucosal forms is not recommended for routine use in the dental surgery. If practised, they will only be administered by a clinician in appropriate circumstances and setting [1–3].
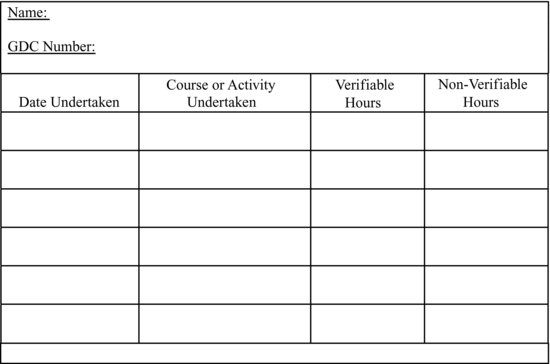
- When a patient receives treatment with sedation, all members of the team must have undergone suitable practical and theoretical training, with every staff member in training being adequately supervised. Any training undertaken must encompass the drugs and equipment used, so that the team can recognise the difference between the normal and the abnormal. As a result of training they will understand the action of each drug and also the use of the equipment. They will be able to clinically monitor patients, identify complications and know how to rectify them. The team must be capable of recognising and managing any emergency, so they must source training of this nature and undertake regular simulations. Training can be either through attendance at a formal course or in-house. Any person organising training for others must ensure that the training is delivered by appropriate instructors and in suitable settings. Continued professional development is vital to ensure that the practice of sedation is safe, relevant and up-to-date, with the frequency of any courses attended being variable, depending upon the area of work. All training received must be documented [1–3] (Figure 2.2).
Figure 2.2 Continued professional development tracking document.
- The surgery will, of course, be suitable for the provision of sedation, with both the treatment and recovery areas being spacious enough for the team to undertake treatment and manage an emergency should one occur with the chair’s equipment allowing the head down tilt position [1–3].
- Should any complications occur the team must be able to respond accor-dingly and be aware of the associated risks. The entire team must be familiar with emergency procedures, having received training and updates on a regular basis. Simulations should be held within the practice. All emergency drugs must be available, restocked and kept secure, coupled with a means of administering them to patients. They should be checked on a daily basis to ensure that they are in date, with equipment serviced and maintained according to the manufacturer’s guidelines. A means of securing a patent airway and administering oxygen must be available. Risk assessments must be undertaken in order to control the provision of sedation and to reduce the risk of accidents or mishaps. Dental practices should undertake audits to police the quality of care provided, ensuring best practice [1–3].
- For inhalation sedation, only dedicated machines for dental use should be used. They must conform to British Standards, be regularly serviced and cared for as per the manufacturer’s guidelines, with records of all this being kept. The oxygen and nitrous oxide cylinders must be stored securely. For piped machines the colour-coded pipes must only fit into their respective outlets. They must also comply with the set standards and have fail-safe mechanisms installed so that the patient cannot receive a hypoxic mixture. Scavenging systems to remove the waste nitrous oxide from the atmosphere must be installed and used to prevent any health problems for the team. The nasal mask provided to the patient must be a good fit to avoid excess nitrous oxide being exhaled into the surgery [1–3].
- For intravenous sedation, the surgery must be stocked with all the required sedation and emergency equipment in order for it to be provided to patients, with all members of the team involved having sufficient and suitable know-ledge and skills. All electrical equipment used must be calibrated, serviced and maintained according to the manufacturer’s guidelines, with records of such being kept. Drugs and syringes must be labelled for correct identification and administration of any drug should be according to accepted current guidelines when titrated against the response of the patient [1–3].
- For oral sedation, the lowest possible dose should be prescribed, which is only sufficient to allow the patient to sleep the night before their appointment and to reduce their anxiety level. Patients must be advised that they will have to adhere to the same pre and post-operative restrictions as for intravenous sedation and they must be accompanied by a responsible escort. Oral sedation in this form is not to be mistaken for oral off-licence sedation. This specific technique, along with intranasal and transmucosal techniques, should only be undertaken in a suitable setting where the team have the knowledge and skills to provide this mode of sedation [1–3].
- To prepare patients for sedation, written and verbal pre and post-operative instructions must be provided to both the patient and their escort so that they both understand their respective roles before, during and after the appointment [1–3].
- Following treatment, patients must be supervised by an appropriate member of the team who will monitor and respond should an emergency arise, with all emergency drugs and equipment available. The recovery phase will initially commence in the dental chair until the patient is assessed as being ready to be moved to a recovery area, if available. The patient must be allowed time to recover and during this period the clinician must be available. It is not acceptable for any patient’s recovery to take place in the waiting room. Not all patients recover at the same rate, with the rate dependent upon the drugs and amounts provided. Before being discharged, patients must be able to walk without help and be steady on their feet. They will be assessed for discharge by the clinician/sedationist and, when ready, discharged into the care of the responsible escort who will be in receipt of the post-operative instructions for both sedation and dental treatment. These instructions should also contain emergency telephone numbers [1–3].
- Excellent record keeping is important and must reflect the patient’s treatment pathway and consent to treatment. Therefore they must contain the following details:
- Patients’ medical, dental and social history, including any previous treatments, general anaesthetic and/or conscious sedation and any change in the medical history/status.
- Details of the assessment appointment.
- The mode of sedation and the treatment being provided, the justification for its use and any patient preferences.
- Written consent and that verbal and written pre and post-operative instructions were provided. The patient is still happy to proceed with the planned treatment and they have adhered to all instructions. The re/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


