5
Three – Dimensional Diagnosis and Treatment Planning of Dentoalveolar Problems
Dentoalveolar surgery is often required for the removal of impacted teeth, difficult extractions, the exposure of teeth for orthodontic reasons, and endodontic and implant surgery. Diseases of the jawbone and soft tissue are also treated in this field of oral surgery.
X- ray imaging is frequently applied to support the clinical diagnosis of dentoalveolar problems and to establish a treatment plan. For the broad scope of interventions in dentoalveolar surgery, a range of different imaging procedures and technologies are available. The basic diagnostic tools are twodimensional (2D) radiographs such as panoramic, periapical, cephalogram, and transversal images. In the early 1970s, the 2D spectrum of diagnostic capabilities was extended by three-dimensional (3D) imaging based on computed tomography (CT).1 Since then, the high- paced development of 3D imaging in dentistry has led not only to an excellent image quality, but also to a wide range of software applications supporting diagnosis and treatment planning in dentoalveolar surgery. These include:
- 3D representations of tomographic scans that can be reconstructed and visualized from arbitrary views by computers;2
- virtual as well as real stereolithographic 3D models that can be generated individually for each patient and used as models for exact surgical planning and the prediction of surgical outcomes;3–5
- computer- driven, image- guided robots that can be used to precisely and constantly drill, cut, and saw;6
- virtual surgical training devices and 3D representations of normal anatomy that may be used to enhance medical education and training;7
- tomographic scans and 3D models that can be matched to the real operating scene and provide the surgeon with image guidance during surgery.6,8,9
Although these technologies were in part developed in other fields of oral and maxillofacial surgery, dentoalveolar surgery has greatly benefited from these developments, especially in the field of dental implantology. Computer- aided planning software based on 3D imaging has been established since the late 1990s.10 Following this development, different approaches to transfer virtual plans into surgical reality have been proposed and clinically applied.
The aim of this chapter is to introduce the diagnostic options and capabilities of 3D imaging in combination with computer- aided methods for the treatment of dentoalveolar problems.
Requirements for 3D imaging in dentoalveolar surgery
For a successful application of 3D imaging over the wide spectrum of dentoalveolar problems, a sufficient volume size, the highest possible spatial resolution at short exposure time, and the lowest possible dose are required. Furthermore, the space requirement for the unit should be small, and the operation and positioning of the patient efficient and simple, so that imaging can be well integrated into the clinical workflow.
The required volume size depends upon the relevant indication but should as a rule display the area of interest with a sufficient safety margin. For osteotomies of wisdom teeth, present in all quadrants, and for implant planning, both jaws should be shown completely, as well as the temporomandibular joint for implantologic diagnostics and planning. For other impacted or retained teeth, a smaller volume may be sufficient, but for smaller volumes (e.g., 6 × 6 × 6 cm), positioning of the patient is critical since the volume of interest has to be aimed at before the exposure. Volumes too small in size tend to provoke repetitive scans since the volume of interest is not fully contained in the actual scan, resulting in an additional dose for the patient.
The spatial resolution should be between 0.3 and 0.8 mm for displaying dental structures.11 However, for a proper diagnostic workup of impacted teeth and endodontic surgery, a resolution of 0.1 mm or less is desirable in order to diagnose subtle pathologic processes involving the root canals or the periodontal ligament.
Image quality and resolution are influenced by the amount of dose applied, the duration of the scan (i.e., probability of motion artifacts), and the reconstruction algorithms. The shortest possible exposure time is crucial, since the risk for moving artifacts rises with longer exposure times.12 The necessary dose for 3D imaging for planning dental implants should be comparable to that of conventional exposures, whereby the exposures for the conventional second- plane X- ray must be considered in the total summation. The exposure itself should be able to display clearly in 3D the bone substance of the region of interest, and permit comparative density measurements for estimating the bone quality.
Requirements for 3D diagnostic software
With the advent of 3D image volumes, a significant amount of additional information is available to the dentist. Considering an efficient clinical workflow, the software for inspecting 3D image volumes has to be designed specifically for its main group of users, and thus prioritize dental requirements over radiologic ones. For 3D diagnostics in general medicine, predominantly orthogonal slice views are used, and doctors are trained accordingly. In dentistry, panoramic, periapical, and occlusal radiographs and cephalograms are common radiologic techniques. Slice- based diagnostics have so far been rarely used in dentistry and are therefore challenging for many active practitioners.
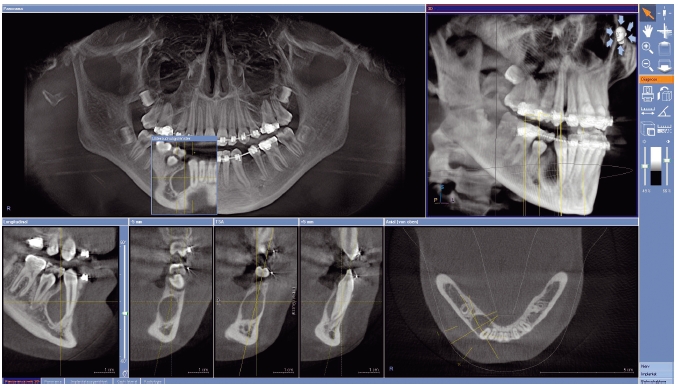
To provide the user with a familiar environment, some software mathematically calculates a panoramic view from the 3D data record as an overview. For a dentist, this means that a customary clear display of the relevant anatomy should be easy as a navigational basis in the 3D space (Figure 5.1). Using that functionality requirement, the common panoramic view can be linked to the 3D information provided by the scan. This approach cannot only be realized for the panoramic view, but also for cephalograms. Basic functionality as measuring true distances and angles, as well as contrast and brightness adjustment, are mandatory in 3D software packages.13
Figure 5.1 User interface of the GALILEOS System (Sirona Dental Systems, Bensheim, Germany), offering a panoramic and volumetric view in the upper row for overview as well as perpendicular cuts in the lower row, providing a clear visualization of the anatomy.
In the following section, clinical examples ranging from impacted teeth to implant cases are given for the application of 3D diagnostics and treatment planning based on cone beam imaging.
TREATMENT PLANNING FOR RETAINED OR IMPACTED TEETH
The surgical removal of retained or impacted teeth is one of the most common procedures in dentoalveolar surgery. 14 One of the primary causes of this disturbance in eruption is a lack of space. The third molars, which erupt last, are affected most frequently.15 Depending on the horizontal growth of the jaw, the available space may be inadequate for the molars erupting last in the dental arch, resulting in impacted and/or ectopic wisdom teeth in the region of the mandibular angle.
Besides the wisdom teeth, the maxillary cuspids exhibit the highest incidence of eruption disturbances. These are usually caused by an early loss of the deciduous teeth with mesialization of the premolars erupting before the cuspids. In addition to genetic factors, exogenous influences also determine the eruption of the permanent teeth, resulting in impaction caused by trauma, apical periodontal pathologies, and cyst formation.16 In many cases, the etiology of eruption disturbances remains unknown.
With the exception of the wisdom teeth, the diagnosis of impacted or ectopic teeth is frequently incidental because they are often clinically asymptomatic and are rarely accompanied by other pathologic processes.17 Besides the wisdom teeth, the maxillary and mandibular second molars and the maxillary cuspids are most frequently displaced.18 If the clinical examination records a delayed eruption, dental migration, or an alteration in the bony structures such as a prominence, an X- ray image should be prepared. The affected groups of teeth are described in the following section.
Ectopic incisors
Ectopic incisors are associated with supernumerary tooth buds in the anterior maxillary region and can also result from trauma to the deciduous dentition. 3D imaging allows the exact localization of the tooth and the identification of its root length and root path. Ectopic front teeth frequently exhibit a bend in the root, that is, a dilaceration that can complicate the classification of the tooth.17
Ectopic maxillary cuspids
Ectopic cuspids occur in 1 – 3% of cases, making them less common than ectopic wisdom teeth.15 Palatal displacement is 2.5 – 5 times more common than buccal displacement. A close topographic relationship with the adjacent teeth often exists, and the root may deviate from the longitudinal axis. A radiologic diagnosis of these clinically concealed teeth provides information on their location and morphology, as well as on adjacent structures.19 This includes their positioning and angulation in the dental arch, their developmental stage, the shape and length of the root, the size of the follicle, and possible resorptions on adjacent teeth.
2D images are of limited use. The 3D image of ectopic cuspids permits their differentiated examination and serves as a valuable diagnostic tool. In contrast to conventional 2D imaging, the teeth can be more accurately localized, the possibility of orthodontic correction of the tooth can be assessed based on the periodontal gap, and damage to adjacent structures can be evaluated using a 3D image.
Ectopic mandibular cuspids
The less common displacement of the mandibular cuspids can extend to the mandibular border. The transverse orientation of the tooth and its position in the bone structure should be determined prior to treatment. If a tooth is located in the compact cortex, it must first be moved towards the spongiosa, facilitating orthodontic correction.
Ectopic premolars
Ectopic premolars frequently occur at the end of the primary dental lamina. They can be associated with supernumerary teeth. Due to their location at the transition of the dental lamina, displacements may range from mild manifestations to inversions of the tooth germ.
Ectopic molars
With the exception of the wisdom teeth, ectopic molars are rare and are associated with ectopic adjacent tooth germs.
Imaging parameters
In all eruption disturbances, the decision to either remove, leave, or orthodontically integrate the tooth has to be made by the treating dentist. Together with the clinical history, the diagnostic X- ray procedure is the foundation for this important therapeutic decision (Figure 5.2). The following questions should be answered from the diagnostic X- ray for impacted teeth in order to formulate an appropriate treatment plan:
- What are the dimensions of the tooth, and is there enough space for eruption and integration into the dentition?
- What is the distance to the occlusal plane?
- Is the tooth ankylosed?
- What is the surrounding bone structure of the tooth?
- Are neighboring teeth resorbed, or can a resorption be expected?
- Can a cystic process be detected?
- Is the tooth malformed?
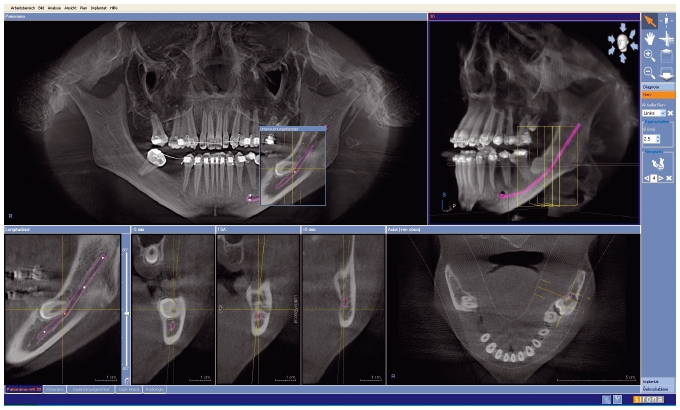
Figure 5.2 Visualization of an impacted third molar in the lower left jaw. The canalis mandibularis is marked.
In the case of leaving the tooth in its position, the patient has to be informed about the potential risk of developing complications and has to be advised for recall. If the tooth can be integrated into the dentition by orthodontic treatment, a surgical treatment plan has to be established to intraoperatively apply a bracket to the tooth that can be used to pull the tooth into occlusion.
The indication for surgical removal of the impacted or retained tooth should be formulated either if integration into the dentition is unlikely to be achieved or if any negative consequences for the surrounding anatomic structures are present or can be expected, as for example the development of a cystic lesion, recurring inflammation (pericoronitis) or the resorption of neighboring teeth.
ORTHODONTIC INTEGRATION OF IMPACTED OR RETAINED TEETH
In order to integrate teeth by orthodontic treatment, the position and angulation of the tooth and its surrounding structures and their relation to the tooth to be integrated have to be clearly identified. Depending on the buccal or oral position, the age of the patient, and the distance of the tooth to the occlusal plane, a combined orthodontic – surgical treatment plan is established. The pre – treatment radiologic information can be used not only to optimally prepare the surgical intervention, but also to estimate the following orthodontic treatment duration.20
SURGICAL REMOVAL OF IMPACTED OR RETAINED TEETH
For any tooth removal, intimate anatomic relationships to the normal structures exist, so that accurate diagnostics are required to prevent secondary injury when removing persisting teeth in abnormal physiological positions.21 Therefore, several diagnostic questions arise prior to surgical removal that can be resolved by 3D diagnostics:
- The anatomic relation to:22
- the alveolar nerve
- the adjacent teeth
- the maxillary sinus
- the nasal floor and cavity.
- The surgical approach:
- a vestibular or oral surgical path
- sectioning of teeth if necessary
- the size of the osteotomy.
The risk of surgical complications involving the surrounding anatomic structures can be reduced by 3D preoperative imaging.22 When planning the surgical procedure, detailed 3D information about the spatial relationship of the tooth to be removed to its surrounding tissues permits not only a clear visualization, but also exact measurements. By assessing the space between the structures involved, minimally invasive surgical approaches can be chosen. This is especially so in the adolescent patient and allows for minor soft tissue preparation and a precisely described surgical procedure. Particularly in dental malformations with associated impaction, preoperative diagnostics allow an estimation of the ability to preserve the tooth and a determination of further therapeutic procedures.23
For wisdom teeth, space limitations often cause eruption disturbances with symptoms ranging from severe pain to recurrent inflammatory reactions in the context of pericoronitis. In addition to the determination of the anatomic position of the tooth, the 3D image serves in the evaluation of crown and root structure and of root growth.22
The 3D image is particularly useful in evaluating potential damage to adjacent structures. For that purpose, specific software tools have been developed that enable the user to enhance the path of the mandibular canal, facilitating the preoperative assessment of its anatomic relation to the tooth to be removed.
From a surgical point of view, ectopic or impacted wisdom teeth are preferably removed after root growth has been substantially reached, ensuring better positional stability of the tooth in the surgical field than would be the case with germectomy. The risk of nerve damage increases significantly with age. Age 25 is given as the critical age. Especially in cases where the root is close to the nerve canal, 3D diagnostics provides greater diagnostic reliability than the combination of panoramic radiography and cranial posteroanterior survey imaging (occipitofrontal beam path, 15 degrees inclination with an open mouth).24
With advanced age or in cases of pronounced displacement, cysts may form. As a rule, the impaction of wisdom teeth is less pronounced in the maxilla than in the mandible. To aid in the prevention of an oroantral fistula, 3D diagnostics provides accurate information regarding the position and characteristics of the roots and of the osseous boundary to the maxillary sinus. In the very rare cases of extreme displacement of wisdom teeth in the maxilla, 3D diagnostics permits an accurate positional determination and an assessment of cystic changes, and thus also determines whether extraction is indicated. By virtue of computer- assisted surgery, such teeth can be easily located, and tissue can be removed conservatively.
Summary
The various manifestations of eruption disturbance require an accurate determination of tooth position relative to the adjacent anatomic structures. 3D diagnostics permits an accurate determination of positional relationships and facilitates a prognosis regarding the course of continuing therapy. This eliminates the positional determination via the preparation of different single images, often with eccentrically guided beams or in several planes. These imaging combinations involve some uncertainty regarding the projection direction and rarely permit an accurate metric analysis or inform about the tissue structure for an assessment of bone quality or the width of the periodontal space.24
In orthodontic treatment planning, the assessment of the position and degree of ankylosis of the impacted tooth, of bone quality, and of spatial relations permits a prognosis to be made for successful orthodontic adjustment. An accurate metric analysis facilitates a decision regarding the ort/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


