5
Piezocision™: Minimally invasive periodontally accelerated orthodontic tooth movement procedure
Serge Dibart1,2 and Elif I. Keser3,4
1 Department of Periodontology and Oral Biology, Boston University Henry M. Goldman School of Dental Medicine, Boston, MA, USA
2 Private Practice Limited to Periodontics and Implant Dentistry, Boston, MA, USA
3 Department of Orthodontics, Boston University Henry M. Goldman School of Dental Medicine, Boston, MA, USA
4 Private Practice, Istanbul, Turkey
Introduction
As already seen in the previous chapters, surgical interventions on alveolar ridges aiming at facilitating orthodontic treatment are not a new concept (Köle, 1959a–c; Suya, 1991), but it was only in the late 1990s that the Wilcko brothers questioned the mechanical concept of bony block movement after reviewing radiographs and computed tomography scans of their patients who had undergone corticotomy-facilitated orthodontic therapy (Wilcko et al., 2001). They hypothesized that rapid tooth movement resulted from a marked but transient decalcification–recalcification process of the alveolus. This concept is known in the orthopedic literature as the regional acceleratory phenomenon (RAP) described by Frost (1983). The Wilckos had understood and witnessed that in their own patients. The elevation of buccal and lingual full-thickness flaps, with extensive decortications of the buccal and lingual alveolar bone, resulted in a physical injury that was responsible for the initiation of a temporary demineralization process coupled with an increased regional bone turnover that characterizes the RAP. They surmised that this transient osteopenia (diminished bone density, same bone volume) is responsible for the rapid tooth movement, as the teeth move in a more “pliable” environment (Wilcko WM et al., 2003; Wilcko MT et al., 2007). Their pioneering work, combining alveolar decortication concomitant with bone grafting to expand alveolar volume and allow for rapid tooth movement into the newly expanded sites, stands out as seminal. Then Vercelotti and Podesta (2007) introduced the use of piezosurgery in conjunction with the conventional flap elevations to create an environment conducive to rapid tooth movement. Although effective, these techniques require flap elevations. They have the potential to generate post-surgical discomfort as well as post-operative complications. Because of these shortcomings they have not been widely embraced by the patient or dental communities. Park et al. (2006) and Kim et al. (2009) introduced the corticision technique as a minimally invasive alternative to create surgical injury to the bone without flap reflection. In this technique, the authors use a reinforced scalpel and a mallet to go through the gingiva and cortical bone, without raising a flap bucally and lingually. The surgical injury created is enough to induce the RAP effect and move the teeth rapidly during orthodontic treatment. This technique, although innovative, has two drawbacks: the inability to graft soft or hard tissues during the procedure to correct inadequacies and reinforce the periodontium, and the repeated malleting, which may cause dizziness after surgery. We are describing here a new minimally invasive procedure that we called Piezocision™. This technique combines micro-incisions limited to the buccal side that will allow for the use of the piezoelectic knife and selective tunneling that allows for hard or soft tissue grafting (Dibart et al., 2009).
Piezocision™
Piezocision can be used to:
- Accelerate orthodontic treatment in a generalized, localized or sequential manner (including localized “ boosters”);
- Enhance the scope of tooth movement through grafting (i.e., posterior buccal expansion, decrowding without extractions due to the increased alveolar volume);
- Achieve differential tooth movement by altering anchorage value through changing the bone density at certain areas;
- Enhance the patient’s profile in certain cases by altering the labiomental fold;
- Repair the alveolar cortical bone fenestrations and dehiscences, and improve the periodontium strength by adding hard or soft tissue grafting;
- Possibly enhance the stability of the orthodontic treatment through stronger alveolar cortices, when grafted.
Indications
- Class I malocclusions with moderate to severe crowding (extraction and nonextraction).
- Selected class II malocclusions (end-on).
- Selected class III malocclusions (dental).
- Correction of deep bite.
- Correction of open bite.
- Rapid adult orthodontic treatment.
- Orthodontic treatment with clear aligners (i.e., Invisalign®).
- Rapid intrusion and extrusion of teeth.
- Simultaneous correction of osseous and mucogingival defects.
- Prevention of mucogingival defects that may occur during or after orthodontic treatment.
- Multidisciplinary treatments.
Contra-indications
- Medically compromised patients.
- Patients taking drugs modifying normal bone physiology (i.e. biphosphanates, corticosteroids etc.).
- Any bone pathology.
- Ankylosed teeth.
- Noncompliant patients.
- Mixed dentition.
- Piezoelectric units must not be used if the patient and/or the operator has a pacemaker or any other active implant (e.g., a cochlear implant).
Armamentarium
- Topical and local anesthetic.
- Scalpel + blade no. 15C.
- Periosteal elevator (24G, Hu-Friedy, Chicago, IL).
- Piezotome (Satelec, Acteon group, Merignac France), insert BS1.
- Bone allograft or xenograft.
- 5-0 chromic gut suture.
- Castroviejo needle holder.
- Surgical scissors.
- PeriAcryl®, cyanoacrylate glue.
- Coe-pack if soft tissue grafting is needed.
Technique
Piezocision is performed 1 week after the placement of orthodontic appliances (Figure 5.1). The patient is anesthetized using Xylocaine 2% with 1/100 000 epinephrine in infiltration. Once complete anesthesia is achieved, a small vertical incision is performed buccally and interproximally in the attached gingiva or mucosa. The incision into the attached gingiva is preferable as it will give less visible postoperative scarring. A mid-level incision between the roots of the teeth involved is made, keeping in mind that the soft tissues and the periosteum need to be cut to create an opening that will allow for the insertion of the piezoelectric knife.

Figure 5.1 Class I malocclusion with moderate anterior crowding. Notice the mucogingival defect on tooth no. 11.
At this point it is important to emphasize the following concept: Piezocision has a localized and selective effect on the teeth. Only the teeth or arch(es) to be moved need to be operated upon. The areas not surgerized have a higher anchorage value, since they are not affected by the demineralization process, and can be used as such in the global treatment plan. Once the vertical interproximal incisions are completed on the maxillary and mandibular arches or in localized segments, the tip of the Piezotome (BS1) is inserted in the openings previously made and a 3 mm piezoelectrical corticotomy is done (Figures 5.2–5.4).

Figure 5.2 Interproximal incisions done with blade no. 15.

Figure 5.3 Interproximal incisions completed in the maxilla.

Figure 5.4 Piezoelectric corticotomy done with the Piezotome (tip BS1, Satelec, Acteon).
The first mark on the BS1 insert can be used as the landmark for the decortication depth as it is located 3 mm from the tip (the decortication has to pass the cortical layer and reach the medullary bone to get the full effect of the RAP). One has to be very careful not to be too close to the interproximal papilla or to the roots, as irremediable damage may occur. In the areas with thin or little gingiva (recessions) or with thin or no cortical buccal bone (dehiscences, fenestrations), hard and soft tissue grafts can be added via a tunneling procedure (Figures 5.5 and 5.6).

Figure 5.5 Tooth no. 11 presents with a gingival recession that will be corrected during Piezocision. A thin periosteal elevator (24 G, Hu-Friedy) is used to create a tunnel from one vertical incision to another. This tunnel will host the connective tissue graft needed to correct the recession.
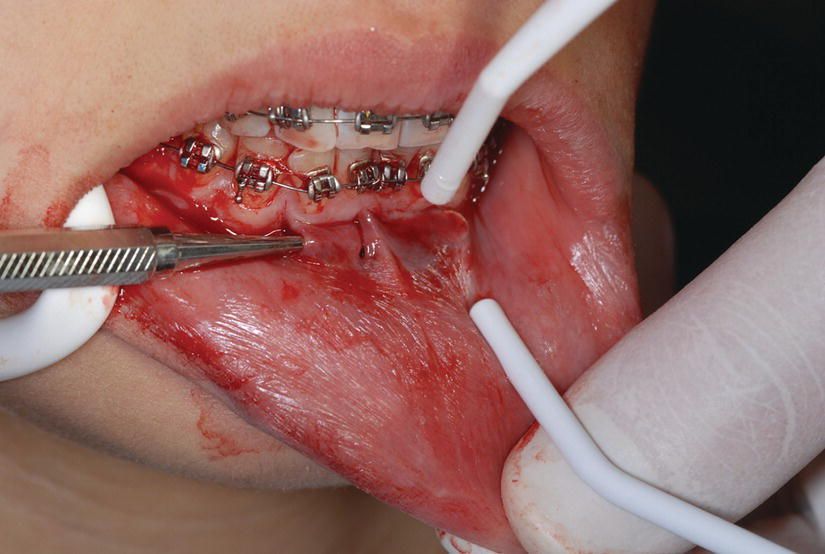
Figure 5.6 Tunneling is being done with the periosteal elevator from canine to canine to accommodate the bone graft needed to expand the mandibular alveolar bony envelope. This added bone will allow for the safe movement of the lower incisors forward.
From one of the vertical openings a periosteal elevator (24G, Hu-Friedy, Chicago, IL) is inserted between the periosteum and the bone and a blunt dissection is carried forward. This will create a tunnel that will host a soft tissue or a bone graft. Once the tunnel has been created, the piezoelectric corticotomy is done in between the roots of the teeth, and a bone graft or soft tissue graft is then added (Figures 5.7 and 5.8).

Figure 5.7 A subepithelial connective tissue graft has been harvested from the palate and placed into the tunnel and secured with 5-0 chromic gut sutures.

Figure 5.8 A bone allograft is being syringed into the prepared tunnel. This will enhance the bone volume and allow for anterior tooth movement with minimal risk.
In the anterior mandible, this can be a little tricky, as only three vertical incisions in the soft tissue are made: between canines and laterals and between the two lower central incisors. This allows for a longer pouch, helping with the retention of the bone graft. Once the procedure is finished, only the areas that have been tunneled will require suturing with a 5-0 chromic gut interrupted sutures. A few drops of cyanoacrylate glue (PeriAcryl) can also be useful to protect these sutures.
The remaining areas (verticals with corticotomy that have not been tunneled) do not need suturing or gluing. The patient is seen a week after the surgery for a follow-up visit and 2 weeks post surgery to start the active phase of the orthodontic treatment. It is very critical for the patient to be seen every 2 weeks thereafter by the orthodontist in order to benefit from the temporary demineralization phase created by Piezocision and allow for faster tooth movement and early completion of treatment (Figures 5.9 and 5.10).

Figure 5.9 At 3 months into treatment, notice the correction of the recession on tooth no. 11 and the appearance of tooth no. 26.

Figure 5.10 Case completed after 12 months.
Differences between conventional orthodontics and Piezocision orthodontics
Piezocision was designed to accelerate orthodontic treatment and at the same time improve the periodontium by hard and/or soft tissue grafting. As mentioned above, this procedure combines micro-incisions limited to the buccal gingiva that allow for the use of the piezoelectric knife to decorticate the alveolar bone without flap elevations and initiate RAP. It also has the advantage of allowing for hard and/or soft tissue grafting via selective tunneling when needed. Virtually all aspects of the accelerated orthodontic treatment utilizing Periodontally Accelerated Osteogenic Orthodontics™ (PAOO) discussed in Chapter 4 also apply to the Piezocision procedure, and therefore the orthodontic considerations in relation to both procedures are very similar. While we will not repeat that discussion here, certain considerations will be briefly reviewed in order to give the Piezocision procedure its proper context.
When the bone is injured, a very dynamic healing process occurs at the site of the bone injury that is proportional to the extent of the surgical insult (Frost, 1989a,b). There is a localized surge in osteoclastic and osteoblastic activity that results, in the early phases, in a decrease in bone density with an increased bone turnover. The RAP begins within a few days of the surgery and usually peaks in 1–2 months and then slows down and disappears as remineralization sets in.
Various animal experiments (Sebaoun et al. 2008, Baloul et al. 2011) have confirmed that alveolar decortication induced a RAP response, and these were discussed in Chapter 4.
More recently, similar research has been done to show the effects of Piezocision on the alveolar bone and tooth movement (Dibart et al., 2013). It has been shown that a similar RAP effect is produced when decortications are done by the piezoelectric knife. In a preliminary study on animals we have found that, although more conservative as a surgical procedure, Piezocision and the use of the piezoelectric knife appear to induce a more extensive and diffuse demineralization effect on the bone than the bur.
When these findings are applied to the clinical setting, it can be suggested that, in addition to accelerating the treatment, the RAP changes the orthodontic treatment planning in two major ways: (1) in anchorage planning, by creating a more “pliable” bone due to the transient osteopenia, and (2) the treatment timing and progress during the “window of opportunity,” where the teeth move faster.
Anchorage
The practice of orthodontics is largely dependent on the availability of anchorage.
The density of the alveolar bone and the cross-sectional area of the roots in the plan perpendicular to the direction of tooth movement are the primary considerations for assessing anchorage potential. The volume of osseous tissue that must be resorbed for a tooth to move a given distance is its anchorage value (Roberts, 2005).
Piezocision can now be defined as another tool for creating differential anchorage. Since it has been shown that the density of the bone around the Piezocision cut is less, the anchorage values of the teeth at the decortication site would be different. Piezocision can be done only around the teeth that are going to be moved, and the anchorage values of these teeth can be decreased. Therefore, the need for additional anchorage devices can be eliminated by designing the alveolar decortication according to the desired tooth movements.
Window of opportunity
The theory behind accelerated tooth movement is that injury to the alveolar cortex induces a bimodal response in the alveolar bone (RAP) that can demineralize the bone around the dental roots. Looking at the literature, once the bone has demineralized following bur corticotomy, there is a 3–4 month window of opportunity to move teeth rapidly through the demineralized bone matrix before the alveolar bone remineralizes (Lee et al., 2008). The effect of Piezocision on the length of this window of opportunity is being investigated. Preliminary results indicate that owing to the more extensive nature of the demineralization engendered by the piezoelectric knife this RAP could last up to 6 months.
This concept is best observed by the patients treated with Invisalign. When Piezocision is done in combination with the Invisalign treatment, the patient changes the aligners every 5 days instead of every 2 weeks. In our practice, Piezocision-assisted Invisalign cases reported that after the fifth or sixth month in treatment, the pressure felt by the aligner decreases much more slowly compared with the earlier months in treatment. This would seem to indicate that the tooth movement starts to slow down back to the normal speed 5–6 months after the Piezocision.
Reduced treatment time
A split-mouth study was done by Gun and Cakirer (2013), to evaluate the effects of Piezocision on the canine distalization rate and rotation, in first premolar extraction cases. When the movement was studied at 10 weeks the canine distalization was two times more on the Piezocision side than the control side, and the canine rotation was similar on both sides. The study concluded that Piezocision is a minimally invasive alternative to corticotomies, significantly shortening the orthodontic treatment time.
Grafting: increasing the scope of tooth movement and improvement of the periodontium
The orthodontic treatment of teeth beyond the limits of the labial or lingual alveolar plate can lead to dehiscence formation (McComb, 1994; Wennstrom, 1996; Joss-Vassalli et al., 2010) and predispose the patient to recession (Zachrisson, 1996; Melsen and Allais, 2005).
Bone grafting increases alveolar volume, thereby increasing the scope of orthodontic tooth movement. Crowding cases can be treated without extraction by the expansion of the alveolus with bone augmentation (Ferguson et al., 2006).
When Piezocision is used, the graft can be placed without the need of a flap elevation. The area where bone graft is needed can be tunneled, the graft material can be placed with a syringe and sutured, and the alveolus of that area can be expanded.
Another positive effect of bone augmentation during alveolar decortication is that it improves the patient’s profile. By grafting the mandibular anterior region, a deep labiomental fold can be corrected and the profile can be enhanced (Figure 5.11).

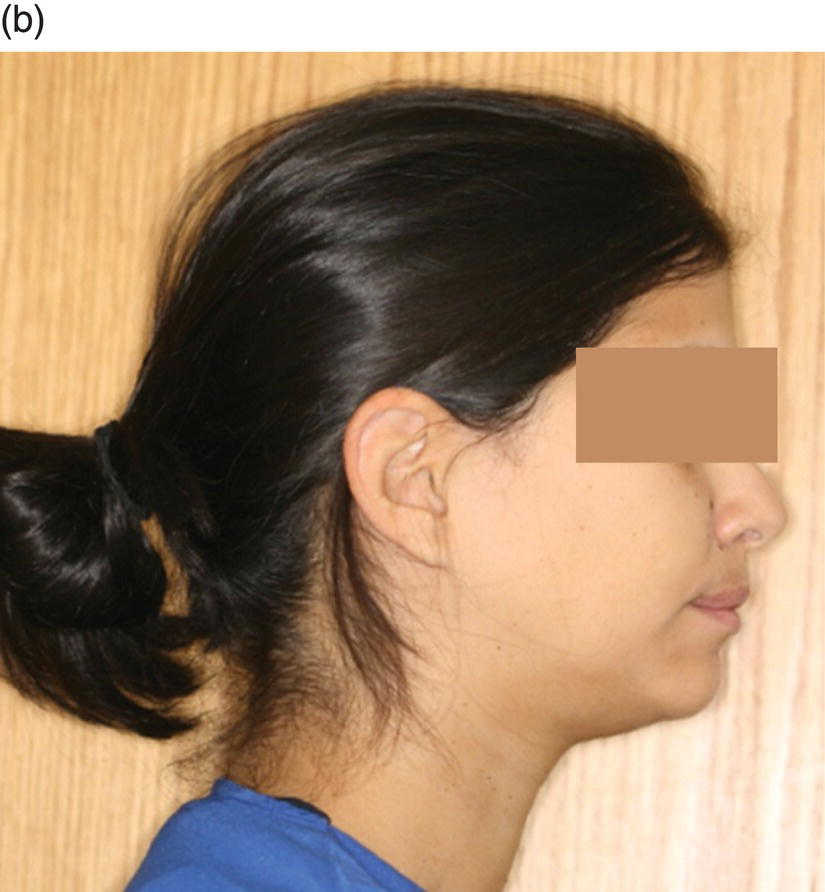
Figure 5.11 (a) Deep labiomental fold. Courtesy of Dr Eleni Kanasi. (b) Improvement of the labiomental fold after grafting.
Courtesy of Dr Eleni Kanasi.
Applications
Piezocision can be used in a generalized, localized, or sequential manner.
If the correction of the malocclusion requires the movement of all the teeth in both the maxilla and mandible at the same time, the decortications should be done in both arches in a single step, and in a generalized manner. Certain cases can benefit from a sequential approach, where the RAP effect is induced at certain areas of the arch at a specific time. And once the desired tooth movement is achieved at these specific locations, the other areas are decorticated to induce the RAP. Since a sequential approach requires decortications at different time points throughout the treatment (meaning multiple surgeries), Piezocision is the preferred option. Piezocision is a minor surgical intervention and does not require flap elevations; therefore, a sequential approach can be clinically applicable by using this minimally invasive method.
When the malocclusion is limited to a segment or only one arch, Piezocision can be used in a localized manner. An example of this woul/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


