5 PERIODONTAL CONSIDERATIONS
ANATOMY
The lining of the oral cavity consists of three types of mucosa, each with a different function1:
Gingiva
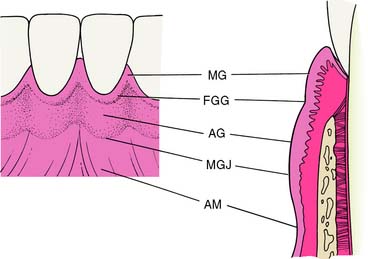
Normal gingiva (Fig. 5-1)—exhibiting no fluid exudate or inflammation caused by bacterial plaque—is pink and stippled. It varies in width from 1 to 9 mm and extends from the free margin of the gingiva to the alveolar mucosa. The gingiva and alveolar mucosa are separated by a demarcation called the mucogingival junction (MGJ), which marks the differentiation between stippled keratinized tissue and smooth, shiny mucosa; the latter contains more elastic fibers in its connective tissue. Apical to the MGJ, the alveolar mucosa then forms the vestibule and attaches to the muscles and fascia of the lips and cheeks.
The gingiva (Fig. 5-2) consists of three parts:
A V-shaped depression on the labial or buccal surface of the gingiva at or somewhat apical to the level of the epithelial attachment to the tooth is called the free gingival groove. It is not always readily apparent clinically but can be seen histologically and may serve as a reference point for dividing the free gingiva from the labially or buccally attached gingiva.2,3
The gingiva consists of dense collagen fibers, sometimes referred to as the gingivodental ligament, which can be divided into alveologingival, dentogingival, circular, dentoperiosteal, and transseptal groups. These fibers firmly bind the gingiva to the teeth and are continuous with the underlying alveolar periosteum. A more detailed description can be found in standard periodontal texts.4–8
Periodontium
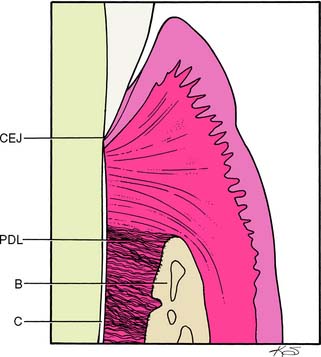
The periodontium is a connective tissue structure attached to the periosteum of both the mandible and the maxilla that anchors the teeth in the mandibular and maxillary alveolar processes. It provides attachment and support, nutrition, synthesis and resorption, and mechanoreception. The main element of the periodontium is the periodontal ligament (PDL), which consists of collagenous fibers embedded in bone and cementum, giving support to the tooth in function (Fig. 5-3). These fibers, also known as Sharpey’s fibers, follow a wavy course and terminate in either cementum or bone. There are five principal fiber groups in the PDL that traverse the space between the tooth root and alveolar bone, providing attachment and support4:
There are also smaller, irregularly arranged collagen fibers interspersed between the principal fiber groups. In addition, the PDL contains elastic fibers9 as well as oxytalan fibers.10
Cellular elements found in the PDL include fibroblasts (the main synthetic cells, which produce collagen and other proteoglycans), cementoblasts and cementoclasts, osteoblasts and osteoclasts (which maintain the viability of their respective tissues), and mast cells and epithelial rests (which play a role in pathologic conditions of the periodontium).1
Dentogingival Junction
At the base of the gingival sulcus (crevice) is the epithelium-tooth interface, also known as the dentogingival junction (DGJ). This structural relationship between hard and soft tissues is unique in the body. At the ultrastructural level, it is made up of hemidesmosomes and a basal lamina, which anchor the epithelial cells to the enamel and cemental surfaces.4,11
The depth of the sulcus varies in healthy individuals, averaging 1.8 mm.12 In general, the shallower it is, the more likely the gingiva is to be in a state of health. Sulcular depths up to 3 mm are considered maintainable. The continued maintenance of the gingiva in a state of health depends on tight, shallow sulci, which in turn depend on optimal plaque control and ensure the success of periodontal therapy, as well as affording a good prognosis for subsequent restorative treatment.
DISEASES OF THE PERIODONTIUM
The general term periodontal disease is used to describe any condition of the periodontium other than normal. It covers such pathologic states as gingival hyperplasia, juvenile periodontitis (also known as periodontosis), and acute necrotizing ulcerative gingivitis—all distinct clinical entities that warrant specific treatment. Information concerning these disease states is available in any of the standard periodontal texts.4–8 Periodontal disease must be recognized and treated before fixed prosthodontics so that the gingival tissue levels can be determined for proper margin placement, esthetics, and gingival displacement (with an AlCl3-impregnated or plain cord; see Chapter 14). Only when the gingiva and periodontium are in an optimal state of health can these determinations be made with ease or predictability.
This discussion is limited to the etiology and progression of the inflammatory gingivitis-periodontitis lesion, which affects the majority of adults13 and constitutes the bulk of pathologic disorders necessitating treatment before restorative dentistry.
Etiology
Most gingival and periodontal diseases result from microbial plaque, which causes inflammation and its subsequent pathologic processes. Other contributors to inflammation include calculus, acquired pellicle, materia alba, and food debris.5,14
Terminology
Microbial plaque
Microbial plaque (Fig. 5-4) is a sticky substance composed of bacteria and their byproducts in an extracellular matrix; it also contains substances from the saliva, diet, and serum. It is basically a product of the growth of bacterial colonies and is the initiating factor in gingival and periodontal disease. If left undisturbed, it gradually covers an entire tooth surface and can be removed only by mechanical means.
Structure of the dental plaque
Dental plaque consists mainly of microorganisms, scattered leukocytes, enzymes, food debris, epithelial cells, and macrophages in an intracellular matrix. Bacteria make up 70% of the solid portion of the mass. The remainder is an intracellular matrix consisting of carbohydrates, proteins, and calcium and phosphate ions.15–17
As the plaque mass increases and matures, the flora progresses apically from a supragingival position, facilitated by the presence of gingival crevicular fluid. The flora also change from a predominantly gram-positive, aerobic, and facultatively anaerobic population of coccoid morphology to a mix relatively high in gram-negative, anaerobic, and rodlike or filamentous organisms, along with increasing numbers of spirochetes.18,19 There is evidence5 that an increase in gram-negative organisms leads to an increase in disease activity within the periodontium and causes both direct and indirect tissue damage.
As the plaque colony matures and increases its mineral content, calculus forms within the plaque mass. Although gingival inflammation is often most severe in areas where calculus is present, the calculus itself is not the most significant source of inflammation; rather, it provides a nidus for plaque accumulation and retains the plaque in proximity to the gingiva. Dental plaque is the etiologic agent of the inflammation.20
Pathogenesis
The pathogenesis or sequence of events in the development of a gingivitis-periodontitis lesion is very complex. It involves not only local phenomena in the gingiva, PDL, tooth surface, and alveolar bone but also a number of complex host response mechanisms modified by the bacterial infection and behavioral factors.21 Implicated in the pathogenic mechanism are phagocytic cells, the lymphoid system, antibodies and immune complexes, complement and clotting cascades, immune reactions, and the microcirculation. Detailed descriptions of host response in the gingivitis-periodontitis lesion are available in standard periodontal texts and reviews.5–7
The chronic plaque-induced lesion has been investigated5,22 in great detail clinically, histopathologically, and ultrastructurally, and the model of disease activity has remained consistent over time. From these analyses, an indistinct division into initial, early, established, and advanced stages has been put forth. The salient features and approximate time frame for each stage are presented here.
Initial lesion
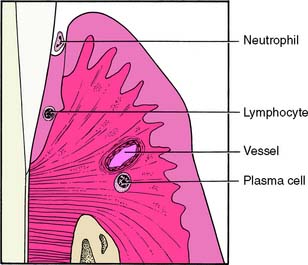
The initial lesion (Fig. 5-5) is localized in the region of the gingival sulcus and is evident after approximately 2 to 4 days of undisturbed plaque accumulation from a baseline of gingival health. The vessels of the gingiva become enlarged, and vasculitis occurs, allowing a fluid exudate of polymorphonuclear leukocytes to form in the sulcus. Collagen is lost perivascularly, and the resultant space is filled with proteins and inflammatory cells. The most coronal portion of the junctional epithelium becomes altered.
Early lesion
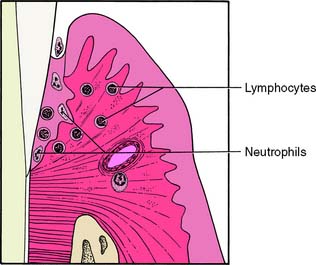
Although there is no distinct division between the stages of lesion formation, the early lesion (Fig. 5-6) generally appears within 4 to 7 days of plaque accumulation. This stage of development exhibits further loss of collagen from the marginal gingiva. In addition, an increase in gingival sulcular fluid flow occurs with increased inflammatory cells and the accumulation of lymphoid cells subjacent to the junctional epithelium. The basal cells of the junctional epithelium begin to proliferate, and significant alterations are seen in the connective tissue fibroblasts.
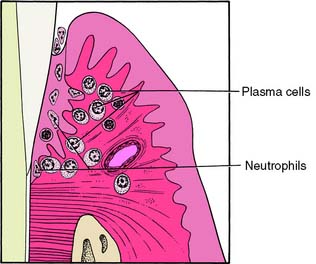
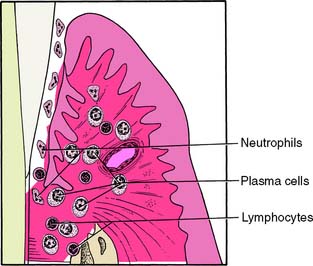
Established lesion
Within 7 to 21 days, the lesion enters the established stage (Fig. 5-7). It is still located at the apical portion of the gingival sulcus, and the inflammation is centered in a relatively small area. There is continuing loss of connective tissue, with persistence of the features of the early lesion. This stage exhibits a predominance of plasma cells, the presence of immunoglobulins in the connective tissue, and a proliferation of the junctional epithelium (Fig. 5-8). Pocket formation, however, does not necessarily occur.
Advanced lesion
It is difficult to pinpoint the time at which the established lesion of gingivitis results in a loss of connective tissue attachment to the tooth structure and becomes an advanced lesion or overt periodontitis (Fig. 5-9). Upon conversion to the advanced stage, the features of an established lesion persist. The connective tissue continues to lose collagen content, and fibroblasts are further altered. Periodontal pockets are formed, with increased probing depths, and the lesion extends into alveolar bone. The bone marrow converts to fibrous connective tissue, with a significant loss of connective tissue attachment to the root of the tooth. This is accompanied by the manifestations of immunopathologic tissue reactions and inflammatory responses in the gingiva.
Periodontitis
When a loss of connective tissue attachment occurs, the lesion transforms from gingivitis into periodontitis (Fig. 5-10), a disease that may be characterized by alternating periods of quiescence and exacerbation. The extent to which the lesion progresses before it is treated will determine the amount of bone and connective tissue attachment loss that occurs. It subsequently affects the prognosis of the tooth with regard to restorative demands.
EXAMINATION, DIAGNOSIS, AND TREATMENT PLANNING
Before treatment is rendered, all facts and findings related to the patient’s disease state should be recorded.23,24 These data can then be used to formulate a precise working blueprint for the proposed treatment. The diagnosis and treatment planning stages should be completed before therapy is initiated. In general practice, the data collection, diagnosis, and treatment planning for a patient’s restorative needs are accomplished at approximately the same time. Although laboratory assessments of gingival microflora and gingival crevicular fluid,24 as well as genetic tests for susceptibility to periodontal diseases, are available,25 traditional clinical assessments are most often employed to arrive at a periodontal diagnosis. These include such factors as probing depths, bleeding upon probing, clinical attachment levels, radiographic evidence of bone loss, and the presence or absence of the patient’s signs and symptoms.26,27 Once the diagnosis has been determined, a treatment plan is presented to the patient.
The following is a viable working model for periodontal treatment:
Initial Therapy
Initial therapy consists of all treatment carried out before evaluation for the surgical phases of periodontal therapy. A number of procedures in each patient’s treatment regimen may be accomplished before more definitive or invasive approaches are undertaken.
Control of microbial plaque
Bacterial plaque occurs on all surfaces of the teeth but is especially prevalent on the gingival third.28 It is strongly adherent to the tooth structure, which means that it is not removed by the chewing of fibrous foods.29 The prevention of plaque accumulation, by either mechanical or chemical means, is crucial in the prevention of hard and soft tissue pathosis. Although there are chemical means for removing plaque accumulation, only mechanical methods are considered in this text. Excellent reviews of the subject of chemical plaque removal are contained in standard periodontal texts.5,7
Toothbrushing
Plaque removal is accomplished with a toothbrush and other orophysiotherapy aids. Many types of toothbrushes can be used and are classified according to their size, shape, length, bristle arrangement, and whether they are manually or electrically powered. The many types of brushes and alternate techniques are reviewed in standard periodontal textbooks.4–7 The soft-bristle brush is particularly effective for cleaning in the gingival sulci and at buccal and lingual surfaces of interproximal areas30,31 without causing gingival damage and tooth abrasion, which can result from a hard-bristle brush.32
Technique
The bristles are placed in the sulci at an angle of approximately 45 degrees to the tooth surface, directed gingivally, and moved back and forth with short scrubbing motions under light pressure. The brush is applied in a similar manner throughout the mouth on all buccal and lingual or palatal surfaces of the teeth. In the anterior area, where interproximal spaces are small and where it may seem impossible to place the brush horizontally against the gingiva, the brush can be turned vertically for better access. After the sulcular areas have been cleansed, the occlusal surfaces are brushed, as is the dorsal surface of the tongue. Excellent descriptions and illustrations of toothbrush placement appear in standard periodontal texts.5–7
Flossing
Interproximal plaque can be controlled with dental floss.33,34 Both waxed and unwaxed types clean proximal surfaces, but the unwaxed floss has several advantages35:
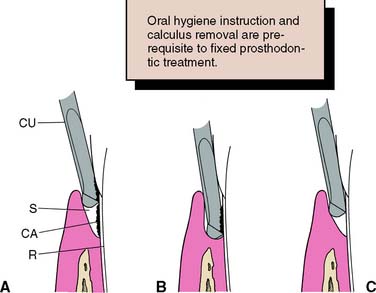
Scaling and polishing
Removal of supragingival calculus (scaling) and polishing of the coronal portion of the tooth are the first definitive steps in débridement of the teeth. Scaling consists of the removal of deposits and accretions from the crowns of teeth and from tooth surfaces slightly subgingival. This is accomplished with the use of sharp scalers or curettes. The gingiva responds to this removal of supragingival and slightly subgingival calculus with a decrease in inflammation and bleeding. Thus, the patient is able to observe the first signs of therapeutic gain, especially when part or half of the mouth is instrumented at one appointment and the remainder is done after a short time has elapsed.
Correction of defective and/or overhanging restorations
Overhanging restorations, open interproximal contacts, and areas of food impaction contribute to local irritation of the gingiva and, of greater importance, impede proper plaque control. These deficiencies (Fig. 5-11) should be corrected during the initial therapy phase of treatment by either replacement or reshaping and/or removal of the overhang (Fig. 5-12). Close cooperation and communication between the periodontist and the restorative dentist are essential during this treatment phase.
Root planing
Root planing (Fig. 5-13) is the process of débriding the root surface with a curette. It is a more deliberate and more delicately executed procedure than scaling and necessitates the administration of a local anesthetic for most patients. At present, it constitutes the primary mode of initial therapy in periodontics, and there is evidence that tooth loss is substantially reduced over time when root surfaces are débrided on a continuing basis.36 Other work has also demonstrated that disease progression continues without root planing, even with effective oral hygiene.37
Strategic tooth removal
Early extraction of teeth and/or roots allows the socket areas to heal and can provide better access for plaque control of adjacent tooth surfaces. A transitional or provisional partial removable dental prosthesis or fixed dental prosthesis can also be fabricated; this stabilizes the arch and potentially maintains or improves occlusion, function, and esthetics.5,7
Stabilization of mobile teeth
Tooth mobility occurs when a tooth is subjected to excessive forces, especially when bony support is lacking. It is not necessarily a sign of disease, because it may be a normal response to abnormal forces, and it does not always need corrective treatment. However, it is sometimes a source of discomfort to the patient, and in these cases it should be treated by reduction of the abnormal forces after occlusal evaluation. Depending on the patient’s need, the teeth may also be treated by splinting with provisional restorations (see Chapter 15) or an acid-etch resin technique (see Chapter 26) in conjunction with occlusal adjustment (see Chapter 6). Such restorations should be carefully designed so they do not impede plaque control or future periodontal treatment. Close communication between the periodontist and the restorative dentist is crucial in this phase of treatment.
Minor tooth movement
Orthodontics can be of major benefit to periodontal therapy. Malposed teeth may be realigned to make them more receptive to periodontal treatment and to improve the efficacy of plaque-control measures. As described in Chapter 6, restorative procedures can also be aided by minor tooth movement. Thus, for the best treatment of a patient with complex dental problems, good communication among consulting dentists is essential.
Surgical Therapy
Soft tissue procedures
Gingivectomy
Gingivectomy is the removal of diseased or hypertrophied gingiva. Introduced by G. V. Black,38,39 it was the first periodontal surgical approach to gain widespread acceptance. Gingivectomy is essentially the resection of keratinized gingiva only, and it may be applied to the treatment of suprabony pockets40 and to fibrous or enlarged gingiva, particularly when they result from diphenylhydantoin (Dilantin) therapy41 (see Fig. 1-4). However, it is unsuitable for the treatment of infrabony defects.
Technique
The surgical technique consists of establishing bleeding points (Fig. 5-14A) at the base of the gingival sulcus with a pocket marker or periodontal probe to serve as a guide for the gingival excision. The initial incision (Fig. 5-14B) is made at these points in a beveled manner with firm, continuous strokes from the gingivectomy knife. The interproximal tissue is freed by sharp excision and is removed from the site. The resulting ledge of tissue at the buccal and lingual or palatal terminations of the incision (Fig. 5-14C) is then smoothed with the knif/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses