14 TISSUE MANAGEMENT AND IMPRESSION MAKING
All teeth in the arch and the soft tissues immediately surrounding the tooth preparation must also be reproduced in the impression. They allow the cast to be accurately articulated and contribute to proper contouring of the planned restoration. Particular attention is given to reproducing the lingual surfaces of anterior teeth because they influence anterior guidance, which determines the occlusal structure of the posterior teeth (see Chapter 4). The impression must be free of air bubbles, tears, thin spots, and other imperfections that might produce inaccuracies.
The patient’s mouth is a challenging environment in which to make an accurate impression. Moisture control is probably one of the most important aspects of successful impression making. Except for the polyethers, all elastomeric impression materials are hydrophobic1 (i.e., they do not tolerate or displace moisture). Any moisture results in voids. Consequently, saliva flow into the area must be reduced and diverted to obtain the necessary dry field of operation. Any bleeding must also be controlled in order to obtain a successful impression.
PREREQUISITES
Tissue Health
After the teeth are prepared and an interim restoration has been made (see Chapter 15), the health of the surrounding soft tissues must be reevaluated. Careful preparation results in minimal tissue damage; however, if a subgingival margin is needed, some tissue trauma in the sulcular area may be unavoidable. The effects of this trauma can be transient as long as the patient receives a properly made interim restoration and maintains adequate oral hygiene. However, if the interim restoration is poorly contoured, is not polished, or has defective margins, plaque retention will lead to a localized inflammatory response. The combination of such tissue trauma in the presence of preexisting periodontal disease can produce disastrous results. Periodontal disease must be treated and resolved before fixed prostheses are placed.
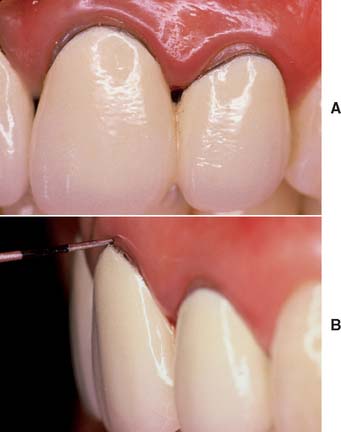
On occasion, a defective restoration contributes to greater plaque accumulation2 and an inflammatory sulcular response (Fig. 14-1). If this is the case, a properly adapted and well-contoured polished interim restoration must be fabricated and cemented on the prepared teeth; the focus must shift from the teeth to the soft tissues, which must be returned to a state of optimum health before impression making is even considered.
Saliva Control
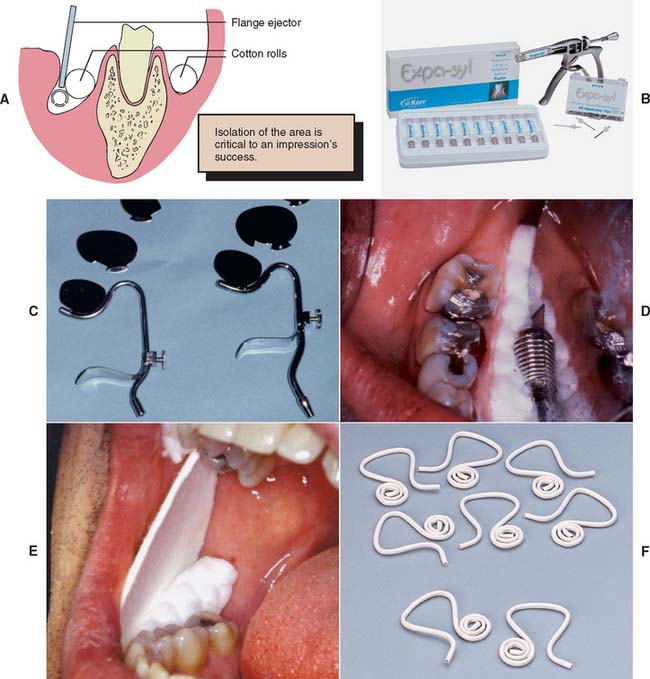
Depending on the location of the preparations in the dental arch, several techniques can be used to create the necessary dry field of operation (Fig. 14-2). In areas where only supragingival margins are present, moisture control with a rubber dam is probably the most effective method. In most instances, however, a rubber dam cannot be used, and absorbent cotton rolls must be placed at the source of the saliva; an evacuator must be placed where the saliva pools. In the maxillary arch, placing a single cotton roll in the vestibule immediately buccal to the preparation and a saliva evacuator in the opposing lingual sulcus is usually sufficient. When work is being done on a maxillary second or third molar, multiple cotton rolls must sometimes be placed immediately buccal to the preparation and slightly anterior to block off the parotid duct, which opens just anterior to the maxillary first molar. If a maxillary roll does not stay in position but slips down, it can be retained with a finger or the mouth mirror. When a mandibular impression is made, placement of additional cotton rolls to block off the sublingual and submandibular salivary ducts is usually necessary. Rolls on the buccal and lingual sides of the prepared teeth help with soft tissue retraction: the cotton on the buccal side displaces the cheek laterally, and the cotton on the lingual side displaces the tongue medially. One or two cotton rolls placed vertically between the horizontally placed cotton rolls in the buccal vestibules help maintain the latter in position.
An alternative to multiple cotton rolls is placement of one long roll “horseshoe fashion” in the maxillary and mandibular mucobuccal folds. However, when part of the cotton is saturated, the entire roll must be replaced. The use of moisture-absorbing cards (see Fig. 14-2E) is another method for controlling saliva flow. These cards are pressed-paper wafers that may be covered with a reflective foil on one side. The paper side is placed against the dried buccal tissue and adheres to it. In addition, two cotton rolls should be placed in the maxillary and mandibular vestibules to control saliva and displace the cheek laterally.
The tongue can cause problems when work is being done in the mandibular arch. Saliva evacuators may help eliminate excess flow, but most of these are easily displaced by a “probing” tongue. If lingually placed cotton rolls continually become dislodged or, in conjunction with a conventional saliva evacuator, fail to control moisture adequately, a flange-type evacuator (e.g., the Svedopter* or the Speejector†) should be considered (see Fig. 14-2C). To avoid the risk of soft tissue trauma, this device must be placed carefully. A cotton roll between the blade and the mylohyoid ridge of the alveolar process minimizes intraoral patient discomfort. Simultaneously, if properly positioned, the cotton roll provides a “stop” that prevents the flange from being displaced farther buccally and thereby allows excellent lingual access to mandibular posterior teeth. Care must be taken not to tighten the chin clamp excessively, because considerable discomfort can result from pressure to the floor of the mouth. A disposable saliva ejector designed to displace the tongue may also be effective (see Fig. 14-2F).
When saliva control is especially difficult, a medication with antisialagogic action may be considered (Table 14-1). Dry mouth is a side effect of certain anticholinergics3,4 (drugs that inhibit parasympathetic innervation and thereby reduce secretions, including saliva). This group of drugs includes atropine, dicyclomine, and propantheline. Anticholinergics should be prescribed with caution in older adults and should not be used in any patient with heart disease. They are also contraindicated in individuals with glaucoma, because they can cause permanent blindness. The incidence of undiagnosed glaucoma in the general population is high, and some physicians recommend that all patients be evaluated ophthalmologically before anticholinergics are used.
| Brand name | Active ingredient | Dosage |
|---|---|---|
| Pro-Banthine | Propantheline bromide | 7.5–15 mg |
| Robinul (Robinul Forte) | Glycopyrrolate | 1–2 mg |
| Sal-Tropine | Atropine sulfate | 0.4 mg |
| Antipas, Bentyl | Dicyclomine HCl | 10–20 mg |
* Given 30–60 minutes before drying effect is required. (Individual dosage should be adjusted in keeping with most recent guidelines.)
Clonidine,5 an antihypertensive drug, has successfully reduced salivary output. It is considered safer than anticholinergics and has no specified contraindications. However, it should be used cautiously in patients who take hypertension medication. In a clinical trial,6 0.2 mg of clonidine reduced salivary flow as effectively as 50 mg of methantheline.
Displacement of Gingival Tissues
Mechanical displacement is most effectively achieved by placement of a cord (Fig. 14-3) (generally impregnated with a chemical agent). Alternatively, paste systems can be used, often in conjunction with directed pressure. Chemicals such as aluminum sulfate or epinephrine cause localized soft tissue shrinkage. Surgical tissue removal can be accomplished through curettage, excision with a scalpel, or electrosurgery.
Displacement cord
Some enlargement of the gingival sulcus can be obtained by placing a nonimpregnated cord and leaving it in place for a sufficient length of time. The cord is pushed into the sulcus and mechanically stretches the circumferential periodontal fibers. Placement is often easier if a braided cord (e.g., GingiBraid)* or a knitted cord (e.g., Ultrapak†) is used. However, larger sizes of braided cord should be avoided because they have a tendency to “double up” and can become too thick for atraumatic intrasulcular placement. In areas where very narrow sulci preclude placement of the smaller sizes of twisted or braided cord, wool-like cords that can be flattened are preferable for initial displacement of tissue.
Better sulcus enlargement can be achieved with a chemically impregnated cord or by dipping the cord in an astringent (e.g., Hemodent‡). These materials (Fig. 14-4) contain aluminum or iron salts and cause a transient ischemia, shrinking the gingival tissue. Cords with metal filament reinforcement have been developed to help maintain their intrasulcular position.
Even so, the sulcus closes quickly (less than 30 seconds) after the cord is removed; therefore, the impression must be taken immediately.7 In addition, medicaments help control seepage of gingival fluid. Aluminum chloride (AlCl3) and ferric sulfate [Fe2(SO4)3] are suitable because they cause minimal tissue damage. As an alternative, a sympathomimetic amine-containing eye wash§ or nasal decongestant¶ has been shown to be effective.8
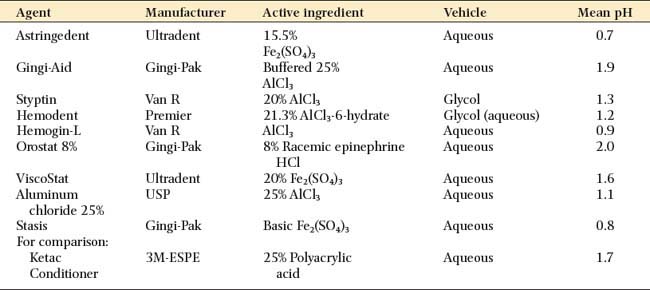
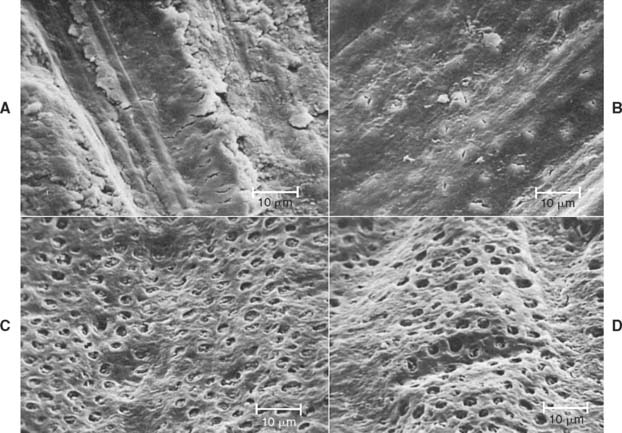
Many of the chemicals used for their astringent effect are stable only at narrow ranges of low pH levels. Table 14-2 shows the mean pH of some commonly used materials. The low pH levels have raised concern about the effect of acidic solutions on tooth structure and, perhaps of more importance, on the smear layer.9,10 Figure 14-5 represents scanning electron micrographs of dentin after various durations of exposure to a commonly used ferric sulfate solution. Contact between the astringent and the prepared tooth surfaces must be minimized if the smear layer is to be maintained. A nonacidic hemostatic agent can be used as an alternative.
Several displacement cords preimpregnated with epinephrine are available commercially. Epinephrine should be used with caution, because it may cause tachycardia,11 particularly if it is placed on lacerated tissue. Dosage control is also a potential problem. In one study,12 clinicians were unable to detect any advantages of using gingival retraction cords that were impregnated with epinephrine.
A 1999 survey determined that 54% of prosthodontists prefer use of buffered AlCl3 to soak displacement cord, whereas more than 35% routinely use ferric sulfate or aluminum.13 The same researchers reported use of a double-cord technique in almost half of the clinical situations. With this technique, a thin cord is placed without overlap at the bottom of the gingival crevice. A second cord is placed on top to achieve lateral tissue displacement. The latter is removed immediately before impression making, whereas the initial cord is left in place to help minimize seepage.
Step-by-step procedure
It is best to start in the interproximal area (Fig. 14-6D), because the cord can be placed more easily there than facially or lingually. The instrument should be angled toward the tooth so the cord is pushed directly into the sulcus. It should also be angled slightly toward any cord already packed; otherwise, that might be displaced. A second instrument (Fig. 14-6E) may aid placement.
Evaluation
On many occasions, it is better to delay impression making and concentrate on how to improve tissue health (e.g., by reassessing the quality of the interim restoration and reinforcing oral hygiene instructions) rather than to attempt impression making under adverse conditions. Minor hemorrhaging can sometimes be controlled with an astringent* or by infiltrating a local anesthetic directly into the adjacent gingival papillae.
Hemorrhage control with an infusor syringe
Displacement paste
Some dentists advocate displacement paste† (Fig. 14-8) as an alternative to cord.14 The product consists of an aluminum chloride-containing paste that is injected into the dried sulcus with a special delivery gun. Advantages of the system include good hemostasis with less discomfort than traditional cord. However, less tissue displacement is achieved than with cord, which may make die trimming more problematic. Improved displacement may be achieved if the paste is directed into the sulcus by applying pressure with a hollow cotton roll.‡
Electrosurgery
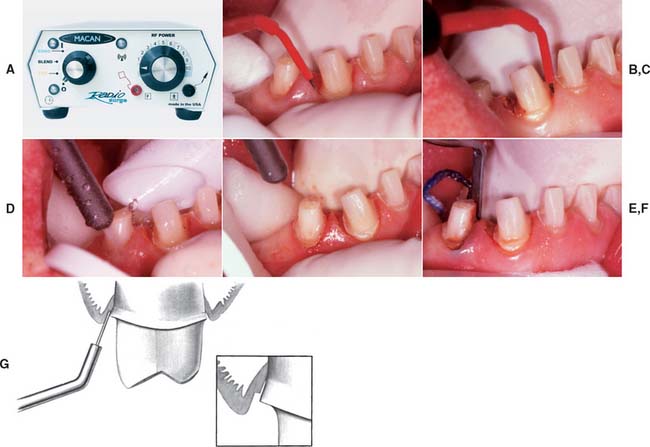
An electrosurgery unit15—18 (Fig. 14-9A) may be used for minor tissue removal before impression making. In one technique,19 the inner epithelial lining of the gingival sulcus is removed, thus improving access for a subgingival crown margin (see Fig. 14-9B to F) and effectively controlling postsurgical hemorrhage20 (provided that the tissues are not inflamed). Unfortunately, there is the potential for gingival tissue recession after treatment.21
An electrosurgery unit works by passage of a high-frequency current (1 to 4 million Hz*) through the tissue from a large electrode to a small one. At the small electrode, the current induces rapid localized polarity changes that cause cell breakdown (“cutting”). For restorative procedures, an unmodulated alternating current is recommended, because it minimizes damage to deeper tissues.16
The following facts should be considered before electrosurgery is attempted:
MATERIALS SCIENCE
Elastic Impression Materials
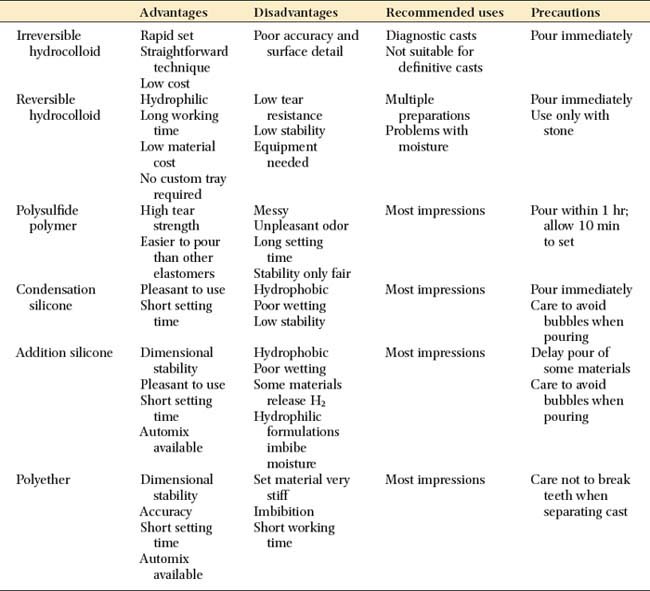
Irreversible hydrocolloid is not sufficiently accurate for cast restorations. Each material has advantages and disadvantages, and none is entirely free of shortcomings. However, they all share one important characteristic: when handled correctly, they can produce casts of sufficient accuracy25 and surface detail26 for the fabrication of clinically acceptable fixed prostheses.
Nevertheless, there are reasons for selecting one material over another: If it becomes necessary to store the impression before a cast is made, the polyethers and addition silicones are preferable because they exhibit sufficient long-term dimensional stability; the other materials, particularly the reversible hydrocolloids, must be poured immediately. If the impression is to be poured in epoxy or electroplated (see Chapter 17), reversible hydrocolloid should not be selected because it is compatible only with die stone.
The advantages and disadvantages of the elastic impression materials are summarized in Table 14-3.
Reversible hydrocolloid
Reversible hydrocolloid (also called agar hydrocolloid or simply hydrocolloid) (Fig. 14-11) was originally derived as a natural product of kelp. However, the material currently available is considerably different.

Fig. 14-11 Reversible hydrocolloid impression material. A, Tray and wash material. B, Syringe material.
(Courtesy of Dux Dental, Oxnard, California.)
If poured immediately, reversible hydrocolloid produces casts of excellent dimensional accuracy and acceptable surface detail. At elevated temperatures, it changes from a gel to a sol. This change is reversible; that is, as the material cools, the viscous fluid sol is converted to an elastic gel. Agar changes from gel to sol at 99°C (210°F) but remains a sol as low as 50°C (122°F), forming a gel only slightly above body temperature. These unique characteristics are very favorable for its use as an impression material.
Reversible hydrocolloid is supplied in a range of viscosities. In general, a heavy-bodied tray material is used with a less viscous syringe material. The required temperature changes are effected with a special conditioning unit (see Fig. 14-31) and water-cooled impression trays.
Reversible hydrocolloid’s lack of dimensional stability results primarily from the ease with which water can be released from or absorbed by the material (syneresis and imbibition). The accuracy of a reversible hydrocolloid impression is improved if the material has as much bulk as possible (low surface area/volume ratio). This contrasts with the elastomeric impression materials, whose accuracy is improved by minimizing bulk (e.g., polysulfide and condensation silicone), because stresses produced during removal are reduced.27 Therefore, an additional advantage of reversible hydrocolloid is that a custom impression tray is not required.
Polysulfide polymer
The polysulfides (Fig. 14-12), commonly (although erroneously) known as rubber bases,* were introduced in the early to middle 1950s. They were received enthusiastically by dentists because they had better dimensional stability and tear strength than did hydrocolloid. Nevertheless, they should be poured as soon as possible after impression making; delays of more than an hour result in clinically significant dimensional change.22
There is a slight contraction of polysulfide during polymerization, but the effects can be minimized with a custom impression tray to reduce the bulk of the material.28 In general, a double-mix technique is used with a heavy-bodied tray material and a less viscous syringe material. These polymerize simultaneously, forming a chemical bond of adequate strength.29
The high tear resistance30,31 and enhanced elastic properties of polysulfide facilitate impression making in sulcular areas and pinholes, and it has improved dimensional stability over hydrocolloid (inferior to polyether and addition silicone). Although it is the least expensive elastomer, it is not well liked by patients because of its unpleasant sulfide odor and long setting time in the mouth (about 10 minutes). Furthermore, high humidity and temperature dramatically reduce its working time,32 which may be so short that polymerization begins before it is inserted in the mouth, which results in severe distortion. Although air conditioning is common in dental operatories/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses