CHAPTER 48 Management of Fear and Anxiety
Fear and anxiety of dental procedures are common emotions. The severity ranges widely, with mild apprehension being reported by 75% of the population,59 and severe anxiety, leading to avoidance of dental treatment, being reported by 4% to 21%.11,21,49 As shown in Table 48-1, the prevalence of fear and anxiety is not restricted to one culture but shows consistency internationally.11 Dental anxiety has not diminished but has remained stable over the past 50 years despite advances in the delivery of dentistry.61 It has also been shown that this fear begins in childhood and can persist throughout life, leading to avoidance of dental care and contributing to diminished oral health.23 Although mild fear may have only a minor effect on oral health, detrimental consequences for overall health can result if true phobia causes patients to avoid treatment despite significant symptoms.8,49
TABLE 48-1 International Prevalence of Dental Fear and Anxiety
| COUNTRY | PREVALENCE OF HIGH DENTAL FEAR AND ANXIETY |
|---|---|
| Australia | 13.7% |
| Canada | 4.4-16.4% |
| Denmark | 4.2% |
| Iceland | 4.8% |
| Japan | 20.9% |
| Netherlands | 3.9-10.8% |
| New Zealand | 12.5-21.1% |
| Singapore | 7.8-20.8% |
| Sweden | 3.9-6.7% |
| United States | 10-19% |
Data compiled by Chanpong B, Haas DA, Locker D: Need and demand for sedation or general anesthesia in dentistry: a national survey of the Canadian population, Anesth Prog 52:3-11, 2005.
Approximately 40% of the population do not receive routine dental care, with apprehension being cited as the most common reason.4 These patients often require special nonpharmacologic or pharmacologic approaches to allow dental procedures to be done. Pharmacologic approaches involve drugs that produce effects ranging from minimal sedation to general anesthesia.
Dentistry has historically been at the forefront in the development of anesthetic techniques to manage fear and anxiety. As described in Chapter 17, two dentists, Horace Wells and William Morton, were largely responsible for the clinical introduction of general anesthesia. The first description of nitrous oxide (N2O) as a sedative, as opposed to a general anesthetic, appeared in a textbook on anesthesia for dentistry published in 1908.17 The modern form of N2O and oxygen sedation evolved in the 1940s and 1950s, and this practice has become a standard component of the predoctoral dental curriculum.3 Intravenous anesthesia with hexobarbital was pioneered by the English dentist S.L. Drummond-Jackson in the 1930s. Shortly after World War II, Harold Krogh and Adrian Hubbell developed the use of thiopental for oral surgery. Intravenous conscious sedation (now termed moderate sedation) was introduced by Niels Jorgensen in 1945.
GENERAL PRINCIPLES
Indications for Use
The primary indication for pharmacologic methods of patient management is the presence of anxiety, fear, or phobia sufficient to prevent the delivery of needed dental care. Anxiety may be defined as a stress response to an ill-defined or anticipated situation46 and may consist of patterns of autonomic arousal with thoughts of fear and feelings of threat.54 Dental anxiety may be related to specific dental procedures or may be precipitated by a mere visit to the dentist’s office. Although anxiety of dentistry usually originates from past experiences as a child,40 it may develop in adulthood and not be associated with any previous adverse event.66
Fear is defined as an emotional response to a perceived immediate threat.24,57 Fear of dentistry may evolve from many sources, including past traumatic experiences, concerns about physical loss and disfigurement, observation of anxiety or fear in others, and exposure to frightening anecdotes by friends or the mass media.59 Specifically, fears of the anesthetic “shot” and dental “drill” are the most common.36,47 A phobia is a persistent and irrational fear that results in a compulsion to avoid a specific object, activity, or situation.
A strong relationship exists between anxiety and pain. Expectation of pain contributes significantly to dental anxiety, and anxiety can reduce pain tolerance59 to the extent that normally innocuous stimuli, such as touch, may be interpreted as pain. Many cases of failed mandibular block are a result of patient anxiety.67 Anxiety can also contribute to adverse reactions in the dental chair; these are commonly misdiagnosed as either allergic or toxic reactions to the local anesthetic or vasoconstrictor. Comprehensive pain control requires an ability to manage fear and anxiety.
Identification of Fearful or Anxious Patients
To address the needs of fearful or anxious patients, the dentist must first be able to recognize or diagnose anxiety and fear. Discussion of how to identify these patients accurately is beyond the scope of this chapter but can be found in other excellent sources.24,48 The degree of anxiety should be determined as part of an appropriate history and patient evaluation. Observation of the patient and questions addressing possible anxiety caused by dentistry may aid in diagnosis. Patient interviews can identify specific concerns, such as fear of the injection of local anesthetic, the sound of the handpiece, or certain surgical procedures. Standardized measures of anxiety, such as the Corah scale,13 may be useful in quantifying the severity of anxiety.
Treatment Planning
After identifying an anxious, fearful, or phobic patient, thought should be given to the optimal method of managing the patient. Initially, nonpharmacologic methods of anxiety reduction should be considered.41,54,57 Appropriate chairside manner is often all that is required; this includes use of basic behavioral modification, positive suggestion, and reassurance. This approach is valuable not only when used alone, but also when used with more specific therapies for anxiety reduction. Specific psychological interventions that may be helpful include desensitization and hypnosis. Although these techniques would not overcome poor chairside manner, they can effectively aid the dentist in achieving patient comfort.
Despite effective chairside manner, many patients still wish to receive sedation or anesthesia. It has been reported that more than 50% of Americans classified as having high fear or anxiety preferred sedation for their dental care.21 The same study showed that three times as many subjects reported a preference for parenteral sedation or general anesthesia when undergoing dental treatment than were actually receiving these modalities.21 This same pattern was seen in a subsequent Canadian study in which patients were asked if they would prefer to have sedation or general anesthesia for each of five procedures.11 There were large differences in this preference compared with actual prevalence for each procedure—specifically, 3.8-fold difference for cleaning, 2.8-fold difference for restorative dentistry, 9.6-fold difference for endodontics, 15.9-fold difference for periodontal surgery, and 2.2-fold difference for extraction. The low preference/prevalence ratio for extractions suggests that dental patients have better access to sedation/anesthesia services for extractions than for other procedures. Extrapolation of these results suggests that nearly 25 million American adults are definitely interested in sedation or general anesthesia for dentistry regardless of the cost.
An absolute requirement basic to the success of patient management is effective local anesthesia. One cannot avoid this necessity in most invasive dental procedures unless complete general anesthesia is being administered. Even then, there may be benefits to the so-called preemptive use of local anesthetic.34,45,68 The dentist should not be misled into thinking that poor local anesthetic technique can be overcome by administering a sedative. Only when the anesthetic failure is strictly caused by anxiety67 would sedation be fully effective.
The ability to use a particular pharmacologic approach depends on the level of training of the dentist and the applicable laws and regulations.3 Education for minimal sedation, such as given through inhalation and oral administration, is within the realm of the predoctoral dental curriculum. More advanced forms, such as moderate sedation, given either orally or parenterally, usually require training at a postdoctoral or continuing education level, although some dental schools have shown that it can be part of a predoctoral program. The most advanced modalities—deep sedation and general anesthesia—require the most formal training. Education for advanced modalities entails a specific postgraduate program devoted to anesthesia (i.e., an accredited residency in dental anesthesiology or an accredited oral and maxillofacial surgery residency, which must include advanced training in anesthesia as part of its curriculum).
Patient Selection
Before choosing pharmacologic adjuncts for patient management, the dentist should carefully review the patient’s medical history. In this context, the American Society of Anesthesiologists (ASA) Physical Status Classification System can be helpful (Box 48-1). This assessment tool can be used to estimate the patient’s overall ability to tolerate the stress of a planned procedure. It can also help determine the need for further patient evaluation and the degree of monitoring required for the procedure.
BOX 48-1 American Society of Anesthesiologists Physical Status Classification System
| CLASS | DESCRIPTION |
|---|---|
| I | Normal, healthy patient |
| II | Patient with mild systemic disease |
| III | Patient with severe systemic disease that limits activity, but is not incapacitating |
| IV | Patient with incapacitating systemic disease that is a constant threat to life |
| V | Moribund patient not expected to survive 24 hr with or without operation |
| E | Emergency operation of any type; E is appended to the patient’s physical status |
ASA I and II patients are usually suitable candidates for sedation or general anesthesia in the outpatient setting. Although outpatient general anesthesia is often inappropriate for ASA III patients, these same patients are at increased risk during stressful procedures when fear and anxiety are not adequately controlled. Techniques to control anxiety involving minimal, moderate, or possibly even deep sedation may be particularly valuable to ASA III patients because they reduce the release of endogenous catecholamines.18,20 ASA IV (and higher) patients are not candidates for sedation or anesthesia in the dental office.
PHARMACOLOGIC APPROACHES
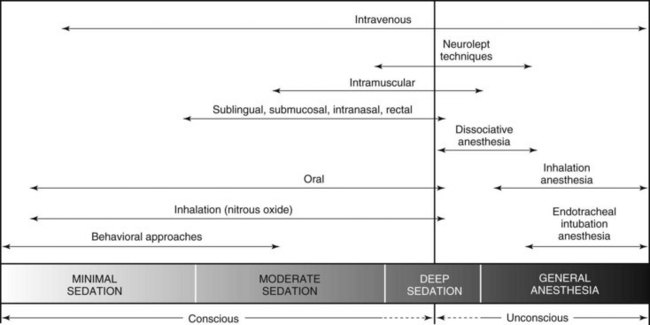
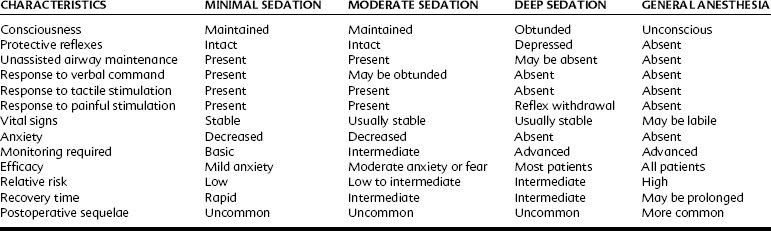
Several pharmacologic approaches can be used to manage fear and anxiety in dental patients. These are commonly referred to collectively as the spectrum of pain and anxiety control, which incorporates all major routes of administration and levels of central nervous system (CNS) depression.43 The route of administration is not synonymous with the level of CNS depression. A spectrum of fear and anxiety control as depicted in Figure 48-1 shows the range of sedation or anesthesia normally sought from the various routes and techniques of administration. In its simplest form, this spectrum is divided into techniques expected to leave the patient awake or to render the patient unconscious. These modalities correspond to sedation and general anesthesia. More recently, definitions of the various levels of sedation have been standardized to include the states of minimal, moderate, and deep sedation.3 The characteristics of these states and of general anesthesia are defined next and compared in Table 48-2:
Minimal and moderate forms of sedation are not substitutes for appropriate chairside manner and use of behavioral techniques but are used to reinforce positive suggestion and reassurance in a way that allows dental treatment to be performed with minimal physiologic and psychological stress. These techniques should carry a margin of safety wide enough to render unintended loss of consciousness unlikely.55 Deep sedation or general anesthesia can be induced by many of the same drugs that induce moderate sedation. The resulting state depends on patient susceptibility, age, medical status, and degree of anxiety and the drug or drugs used and doses administered. Either deep sedation or general anesthesia may be indicated when lighter forms of CNS depression are insufficient to permit treatment.
Reliable morbidity and mortality data for the different forms of sedation or general anesthesia are scarce, but several studies have shown that, overall, the techniques used in dentistry should be considered safe.22,39,42,51,69 Increased mortality is usually associated with inadequate training or inadequate monitoring of the patient.15,16,25,33,38 In a review of adverse events related to sedation in pediatric patients, the use of three or more sedating drugs was more strongly associated with adverse outcomes than was the use of only one or two.15,16 If the goal is minimal or moderate sedation, one must avoid administering excessive doses of a sedative to a patient who remains uncooperative while conscious because it could easily lead to a deepening of sedation in which airway patency and protective reflexes may be lost. Any subsequent lack of oxygenation can rapidly lead to a tragic result. Although the progression from moderate to deep sedation can be accomplished easily, it requires a significantly increased degree of practitioner training, patient monitoring, and physical resources (e.g., anesthetic equipment and supplies) to be performed safely.
MINIMAL AND MODERATE SEDATION
The intramuscular route provides an onset and uptake intermediate between that of oral and intravenous routes. There is a limited ability to titrate with this route, but it can be particularly advantageous for patients who are incapable of cooperating, such as cognitively impaired patients.6 Its use should be restricted to clinicians with training in at least parenteral moderate sedation.
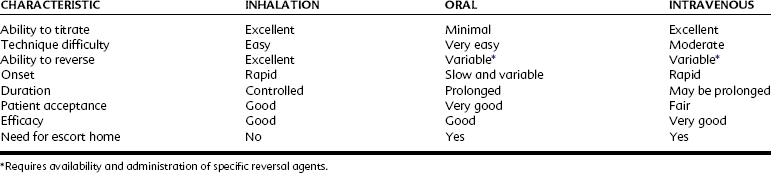
As stated earlier, the route of administration is not synonymous with the depth of sedation. Any route has the potential to induce any degree of sedation or anesthesia. Management of an anxious patient can be discussed according to route of administration, however, because the inhalation and oral techniques are most commonly used for minimal and moderate sedation and are normally the first to be considered. The intravenous route is more likely to be selected to induce a greater depth of effect. Table 48-3 compares the routes of administration for sedation. Commonly used drugs, their routes of administration, and doses for minimal and moderate sedation are summarized in Table 48-4.
TABLE 48-4 Drugs, Routes, and Doses for Minimal or Moderate Sedation
| DRUG | ROUTE OF ADMINISTRATION | APPROXIMATE DOSE* |
|---|---|---|
| Nitrous oxide | Inhalation | 20-50% |
| Diazepam | Oral, IV | 0.05-0.3 |
| Midazolam | Oral, IV | 0.03-0.1 (IV), 0.3-1 (oral) |
| Alprazolam | Oral | 0.002-0.007 |
| Lorazepam | Oral | 0.015-0.06 |
| Triazolam | Oral | 0.002-0.007 |
| Hydroxyzine | Oral | 0.5-1 |
| Promethazine | Oral | 0.5-1 |
| Chloral hydrate | Oral | 40-50 |
| Fentanyl | IV | 0.0006-0.0015 |
| Meperidine | IV | 0.5-1 |
| Morphine | IV | 0.05-0.1 |
| Nalbuphine | IV | 0.05-0.1 |
| Propofol† | IV infusion | 0.025-0.1/min |
* In mg/kg unless otherwise marked.
† The use of propofol is generally restricted in the United States to dentists with formal advanced training in general anesthesia.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses