Treatment of Periodontal Abscess
Classification of Abscesses
The periodontal abscess is a localized purulent inflammation of the periodontal tissues.6 It has been classified into three diagnostic groups: gingival abscess, periodontal abscess, and pericoronal abscess. The gingival abscess involves the marginal gingival and interdental tissues. The periodontal abscess is an infection located contiguous to the periodontal pocket and may result in destruction of the periodontal ligament and alveolar bone. The pericoronal abscess is associated with the crown of a partially erupted tooth.22
Periodontal Abscess
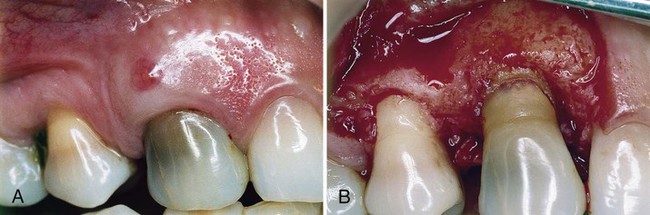
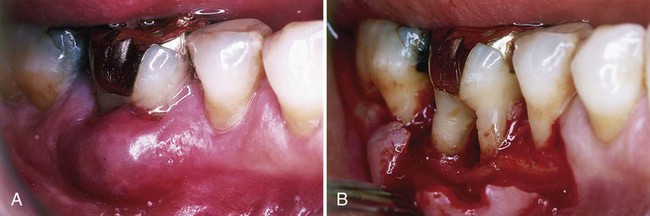
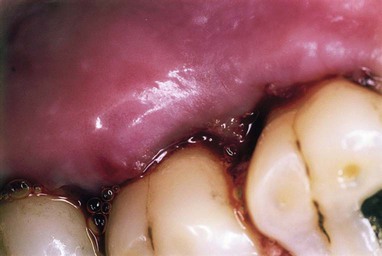
The periodontal abscess is typically found in patients with untreated periodontitis and in association with moderate-to-deep periodontal pockets.5,25 Periodontal abscesses often arise as an acute exacerbation of a preexisting pocket6 (Figure 42-1). Primarily related to incomplete calculus removal, periodontal abscesses have been linked to a number of clinical situations.8,15,16,24 They have been identified in patients after periodontal surgery,12 after preventive maintenance (Figure 42-2),7,10,17,21 after receiving systemic antibiotic therapy,26 and as the result of recurrent disease.15,16 Conditions in which periodontal abscess is not related to inflammatory periodontal disease include tooth perforation or fracture2,24 (Figure 42-3) and foreign body impaction.1,23 Poorly controlled diabetes mellitus has been considered a predisposing factor for periodontal abscess formation22 (Figure 42-4). Formation of periodontal abscess has been reported as a major cause of tooth loss12–21; however, with proper treatment followed by consistent preventive periodontal maintenance, teeth with significant bone loss may be retained for many years7 (see Figure 42-10).
Acute Versus Chronic Abscess
Abscesses are categorized as acute or chronic. The acute abscess is often an exacerbation of a chronic inflammatory periodontal lesion. Influencing factors include increased number and virulence of bacteria present, combined with lowered tissue resistance and lack of spontaneous drainage.11,25 The drainage may have been prevented by a deep, tortuous pocket morphology, debris, or closely adapted pocket epithelium blocking the pocket orifice. Acute abscesses are characterized by painful, red, edematous, smooth, and ovoid swelling of the gingival tissues.15,16,25 Exudate may be expressed with gentle pressure; the tooth may be percussion sensitive and feel elevated in the socket (Figure 42-6). Fever and regional lymphadenopathy are occasional findings.22

The chronic abscess forms after the spreading infection has been controlled by spontaneous drainage, host response, or therapy. Once homeostasis between the host and infection has been reached, the patient may have few or no symptoms.9 However, dull pain may be associated with the clinical findings of a periodontal pocket, inflammation, and a fistulous tract.22
Box 42-1 compares the signs and symptoms of the acute and chronic abscess.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses