Vertical discrepancies
The vertical dimension of face is often altered, either intentionally or nonintentionally, during orthodontic treatment of various dentofacial problems by the extrusion or intrusion of teeth and by growth modification and orthognathic surgery. These changes have a great impact on the way the mandible rotates, either open or closed, with corresponding alterations in maxillomandibular dental relationships, lip and tongue function and, importantly, the facial aesthetics. Therefore, before the initiation of orthodontic therapy, it is vital for the clinician to clearly define the treatment goals related to the vertical dimension of face and design a detailed individualized treatment strategy and mechanics plan based on sound biomechanical principles.
The orthodontic literature related to the management of sagittal discrepancies and to certain extent transverse discrepancies is replete with research, case studies and publications. However, for the most part in the past and still to a large extent in the present, there has been much less research and discussion on the treatment of vertical problems. A large variation in craniofacial growth in the vertical dimension should play a prominent role in orthodontist’s approach to the diagnosis and treatment of malocclusion. The relevance of assessing the vertical dimension to clinical practise is to determine if there is a vertical component contributing to the development of a problem. In a clinical practise, vertical discrepancies are often considered to be the most difficult dentofacial problems to treat. To successfully treat vertical discrepancies, it is important for the clinician to have good understanding of the factors having the greatest influence on the vertical dimension problem. The author believes that in dealing with malocclusions with abnormal vertical component, the simplicity or complexity of the force system is not the deciding factor in producing the best treatment results. Rather, clinicians should have sound knowledge of facial growth and development, interplay between the horizontal and vertical growth, function of the lips and tongue etc.
Development of a vertical problem
Facial growth in relation to the cranial base proceeds along a vector with variable amounts of horizontal and vertical growth. It is important to consider, understand and appreciate the value of vertical growth, as it relates to anteroposterior growth. Vertical growth carries the chin downward, while anteroposterior growth carries it forward (Fig 4.1). The major sites of bony additions contributing to the facial growth include the facial sutures, maxillary alveolar processes, mandibular condyle and mandibular alveolar processes.1 If vertical growth increments at the facial sutures and the maxillary and mandibular alveolar processes exceed the condylar growth, the mandible would rotate backward. However, if growth at the condyle exceeds the total vertical growth at the facial sutures and alveolar processes, the mandible would rotate forward.2 These growth changes significantly alter the lower facial height and the position of chin horizontally and vertically.
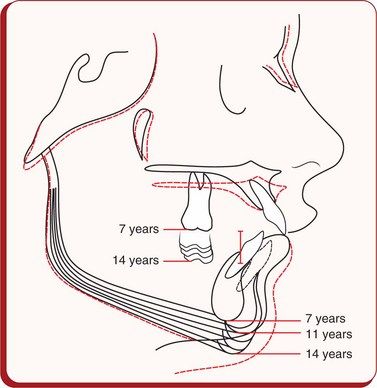
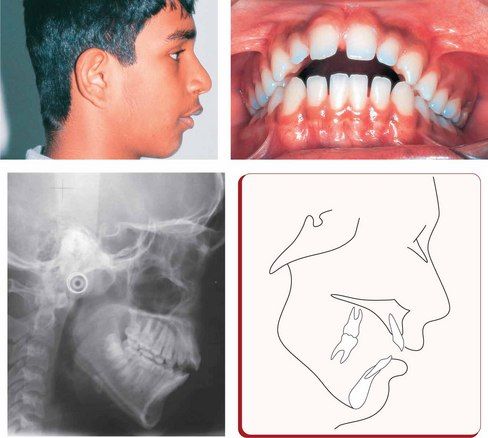
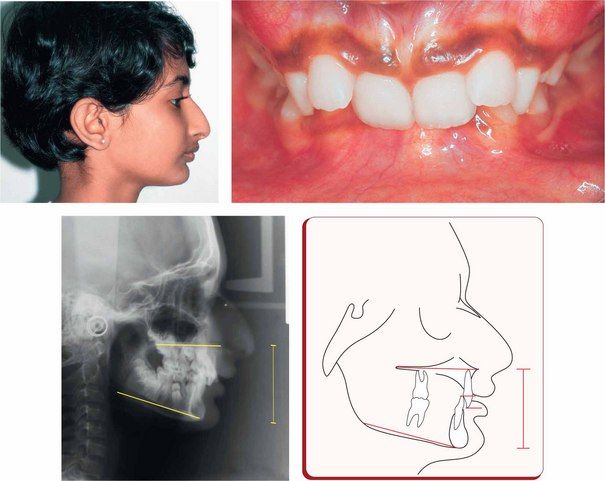
Figure 4.1 Cephalometric superimpositions showing the chin position as a result of growth changes in a patient between 7 and 14 years of age. It was observed that the chin moved downward and forward till the age of 11 years; thereafter, it was displaced downward and backward as a result of less condylar growth and more vertical growth in the molar area.
Growth
For the facial proportions and the occlusal relationships to be normal, the components of the craniofacial complex consisting essentially of the cranial base, nasomaxillary complex and the mandible should exhibit harmonious growth and should maintain a reasonable proportion in size and form. It is well recognized that the spatial position of the maxillary dentition is influenced by the eruption pattern of the teeth and the growth of the maxilla and its contiguous bones. It is also affected by the growth of the anterior cranial base, the area between the pituitary fossa and the internal plate of the frontal bone, to which the maxillary complex is attached. The growth at the sphenoethmoidal suture significantly contributes to the increase in depth of the anterior cranial base and upper face until the suture closes by the age of 7 years.3 After the age of 7 years, further growth in this area until adulthood takes place by surface remodelling of bone on the frontonasal surface, with the sella to the internal plate of the frontal bone dimension unchanged.4
After the cessation of anterior cranial base growth at an early age, the anterior half of the craniomaxillary complex is displaced in an anterosuperior direction by the growth at the spheno-occipital suture until the suture closes after puberty.5 This expression of growth shows a great degree of variation in the direction and rate among individuals. The spatial position of the mandibular dentition is determined by the growth of the mandible and its relationship to the temporal bone. It has been shown that the relationship of the mandible to the anterior border of the foramen magnum (Ba-Ar) does not vary.6 Condylar head, being the primary growth centre of the mandible, grows in upward and backward directions with the resultant downward and forward displacements of the mandible and carries the mandibular dentition away from the vertebral column and cranial base. Therefore, the growth at the spheno-occipital synchondrosis displaces the maxillary complex anterosuperiorly, while the growth at the mandibular condyle displaces the mandible downward and forward (Fig 4.2). These two diverging growth vectors create a space for vertical facial growth, alveolar growth and tooth eruption. Annual incremental growth of various craniofacial components is shown in Figure 4.3.
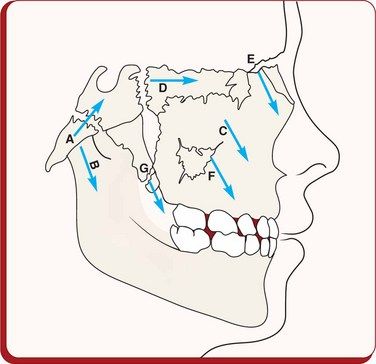
Figure 4.2 Growth at the spheno-occipital synchondrosis during the first decade displaces the maxillary complex anterosuperiorly, while the mandibular condylar growth displaces the mandible anteroinferiorly producing diverging growth vectors to create a space for vertical facial growth, alveolar growth and tooth eruption. Cartilaginous growth: A, spheno-occipital synchondrosis; B, reflection of mandibular condylar growth; C, nasal septum; D, sphenoethmoidal; E, frontomaxillary; F, zygomaticomaxillary; G, pterygopalatine. Image courtesy: Coben SE. Am J Orthod 1966; 52(1):5–26.
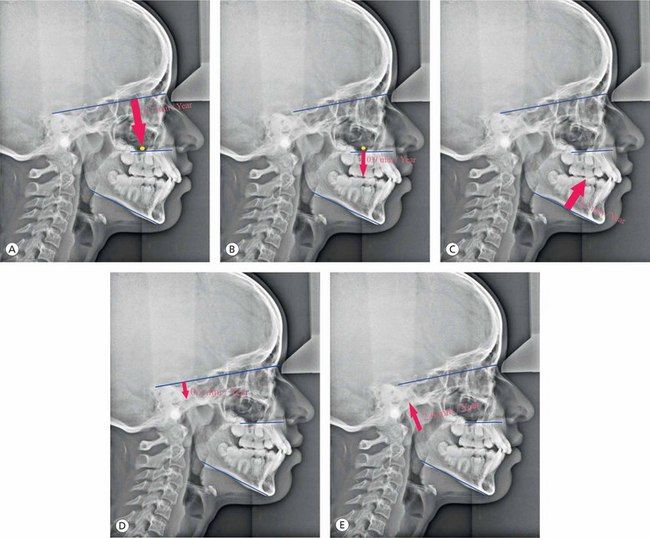
Figure 4.3 Annual incremental growth of various craniofacial components. (A) Average basal maxillary vertical displacement. (B) Vertical maxillary dentoalveolar growth. (C) Mandibular vertical dentoalveolar growth. (D) Vertical displacement of the articular fossa. (E) Condylar growth.
The mandible demonstrates a great degree of variation in the direction of its growth in the normal population as shown in studies on facial growth by Björk and Skieller using metallic implants.7–13 The most common direction of condylar growth is vertical with some anterior component; however, the posterior growth is less frequently observed. Patients with upward and forward growth of the condyle are usually characterized by reduced anterior face height and deep overbite, as seen in Class II division 1 malocclusion. Patients with extreme cases of upward and forward growth of the condyle exhibit a skeletal deep bite, as observed in Class II division 2 malocclusion. Typically, the maxillary and mandibular dentitions are characterized by considerable degree of mesial migration of teeth with some amount of mandibular incisor proclination. Patients with a more posteriorly directed mandibular condylar growth demonstrate a pronounced increase in lower face height and an anterior open bite. The erupting posterior dentition is generally vertical, and quite often, the anterior teeth may even become more proclined with time.
It is important for the clinician to consider, understand and recognize the importance of mandibular growth rotation, as it relates to anterior facial height (AFH) and overbite relationship. Björk11 suggested that under normal situations, the fulcruming point for anterior mandibular growth rotation is located at the incisors (Fig 4.4). In the absence of proper incisal contact due to lip dysfunction, finger sucking habit or severe sagittal jaw discrepancy, the fulcruming point moves posteriorly along the occlusal plane leading to the development of skeletal deep bite. In patients with posterior condylar growth rotation, the fulcruming point is located near the mandibular condyles, with the development of anterior open bite and increased anterior face height.
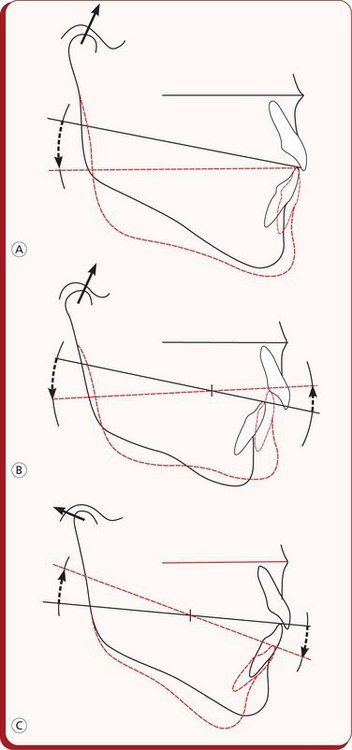
Figure 4.4 Diagrammatic illustration of mandibular growth rotations.
(A) Patients with a stable occlusion demonstrate anterior rotation of the mandible with the fulcrum point located at the incisors.
(B) Patients with lack of anterior occlusion tend to have the fulcruming point located posteriorly along the occlusal plane. (C) In patients with posterior mandibular rotation, the fulcruming point is located near the mandibular condyles. Image courtesy: Björk A. Am J Orthod 1969; 55:585–599.
In addition to the condylar growth direction, differences in AFH and posterior facial height (PFH) development do play an important role in the development of vertical skeletal discrepancies (Figs 4.5 and 4.6). These differences significantly contribute to rotational growth or to changes in mandibular position, influencing the position of the chin.14 The research findings show that the dentoalveolar heights are significantly greater in long AFH patients and smaller in short lower AFH group.15,16 The excessive maxillary posterior dentoalveolar development may be associated with weaker masticatory musculature in high-angle patients compared with stronger musculature associated with low-angle patients.
Environmental factors
The role of certain environmental factors like swallowing, breathing and tongue posture in altered vertical dimension still continues to be the subject of debate. However, breathing problems due to large adenoids, tonsils, deviated nasal septums etc are frequently associated with high-angle patients, which alter mandibular posture, creating more room for posterior teeth eruption. It has been shown that the removal of adenoids and tonsillectomy have resulted in closing of the mandibular plane (MP) angle and reduction in the anterior face height.17,18 The significance of tongue posture and tongue thrust has been evaluated by many with regard to its role as a causative factor in the development of malocclusion.
Diagnosis of vertical discrepancies
Vertical discrepancies consist of various components of the craniofacial complex and are often associated with abnormalities in other planes of space. Their accurate diagnosis is a key element in the design of any successful treatment plan. In order to plan an appropriate treatment strategy, the clinician should localize and quantify any skeletal and dental contributions, vertical and sagittal variations and the role of abnormal function to the development of vertical problems.
Facial evaluation
Facial evaluation should begin with a systematic, three-dimensional assessment of the frontal and profile views in the vertical, sagittal and transverse planes. The goal of this assessment is to establish an accurate description of the aesthetic, skeletal and occlusal abnormalities, as well as functional disorders. Based on the extraoral features, patients with vertical discrepancies may be broadly classified as long-face and short-face patients.
Long-face patients are usually characterized by leptoprosopic facial form and dolichocephalic head form, increased lower facial height, narrow alar bases, prominent nasal dorsum, retrognathic mandible, orthognathic or prognathic maxilla, incompetent lips with mentalis strain, shallow mentolabial sulcus and flattened or recessive chin. Such patients usually exhibit Class II malocclusion with the appearance of mandibular deficiency and are often associated with excessive gingival display upon smile.
Short-face patients can be found in Angle’s Class II and Class III malocclusions. Short-face patients with the most common Class II malocclusion present with decreased lower anterior face height, normal upper lip length, obtuse nasolabial angle, acute mentolabial sulcus, retruded mandible and adequate or excessive soft tissue chin. Short-face patients having Class III malocclusion exhibit many opposite facial characteristics with decreased lower anterior face height, short upper lip, acute nasolabial angle, prognathic appearing mandible and obtuse mentolabial sulcus.
Intraoral examination of the long-face patients reveals maxillary – mandibular dentoalveolar protrusion, upright and supraerupted maxillary and mandibular incisors, excessive eruption of posterior teeth, anterior open bite, high and narrow palate with posterior crossbite etc. Intraoral features common to short-face patients of both Angle’s Class II and Class III groups include excessive deep overbite and deep curve of Spee. The maxillary and mandibular incisors are often upright exhibiting a bidentoalveolar retrusion.19 A short face in these patients is often caused by overclosure of the mandible either due to vertical maxillary deficiency or due to deficient teeth eruption in either the maxilla or the mandible.
Functional assessment
An assessment of function is a very important part of the clinical examination for planning treatment of vertical discrepancies. Associated disorders involving airway, speech and tongue function should be carefully evaluated. It has been generally recognized that environmental factors that are responsible for keeping the maxillary and mandibular teeth apart promote elongation of the posterior teeth, leading to an increase in lower face height. Excessive posterior dentoalveolar development in the maxilla is considered to be associated with weaker musculature in high-angle patients compared with stronger musculature in low-angle patients.20
Morphologic characteristics
Classifying patients into high-angle or long-face patients and low-angle or short-face patients is just a broad understanding of vertical discrepancies. Patients with vertical problems should be further analyzed cephalometrically to identify and locate the structures at fault, which mainly contribute to the development of a problem (Fig 4.7). Their understanding is essential to define the treatment goals and plan a treatment strategy to resolve them. Vertical discrepancies can be divided into those that are dentoalveolar in nature and into those that are predominantly skeletal as a result of the growth patterns of the jaws.
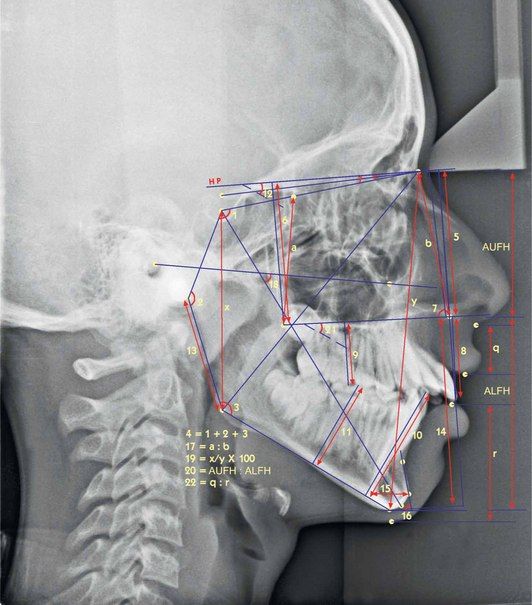
Figure 4.7 Cephalometric assessment of vertical discrepancies. 1. Saddle angle (N-S-Ar); 2. Articular angle (S-Ar-Go); 3. Gonial angle (Ar-Go-Me), upper gonial angle (Ar-Go-N) and lower gonial angle (N-Go-Me); 4. Björk’s sum = saddle angle (N-S-Ar) + articular angle (S-Ar-Go) + gonial angle (Ar-Go-N); 5. Distance between N and ANS (perpendicular to HP); 6. Distance between N and PNS (perpendicular to HP); 7. J angle-angle between palatal plane and perpendicular to N-Se passing through N’; 8. Upper incisor edge to nasal floor (NF) (perpendicular distance to NF); 9. Upper first molar mesiobuccal cusp tip to NF (perpendicular distance to NF); 10. Lower incisor edge to mandibular plane (MP) (perpendicular distance to MP); 11. Lower first molar mesiobuccal cusp tip to MP (perpendicular distance to MP); 12. MP-HP (angle); 13. Length of mandibular ramus (Ar-Go); 14. Distance between ANS and Gn (perpendicular to HP); 15. Width of symphysis measured at Pg, parallel to true horizontal; 16. Symphysis angle-angle between line passing through point B and Pog and true horizontal; 17. Ratio of posterior maxillary height (E-PNS) to anterior maxillary heights (N-ANS); 18. Angle between FH plane and y-axis (S-Gn); 19. Jarabak’s ratio posterior facial height (S-Go)/anterior facial height (N-Me) × 100; 20. Anterior upper facial height (vertical distance from N to ANS): anterior lower facial height (vertical distance from ANS to Me); 21. Angle between palatal plane (ANS-PNS) and mandibular plane; 22. Upper lip length (subnasale to stomion superior): lower lip length (stomion inferior to soft tissue menton).
Cephalometric assessment
High-angle patients are usually characterized by the following:
Low-angle patients are usually characterized by the following:
Vertical Class II types
While assessing various problems in vertical dimension, it is essential for the clinician to understand their impact on the sagittal dimension. Björk11 described morphologic method of predicting growth rotation from a single cephalogram and found seven structural signs for predicting forward or backward growth rotation.
Of these seven original signs, four of the variables when combined give the best prognostic estimate of mandibular growth rotations.24
These parameters are as follows:
Class II malocclusions with vertical discrepancies have been identified as having five vertical types25 (Fig 4.8).
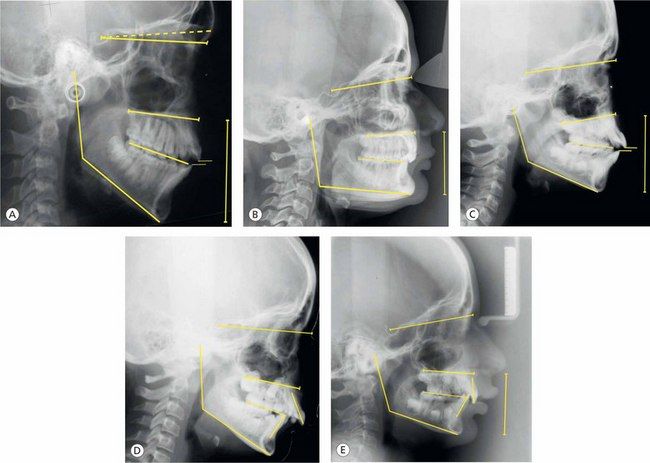
Figure 4.8 Differential diagnosis of vertical discrepancies. Class II malocclusions having five vertical types based on the research by Moyers et al25: (A) Type 1, (B) Type 2, (C) Type 3, (D) Type 4 and (E) Type 5.
Treatment planning
Establishing accurate diagnosis is an integral part of designing a successful treatment strategy. An ideal treatment plan maximizes treatment results and shortens the treatment duration. Defining treatment goals – facial, skeletal and dental – is the best way to approach treatment planning for the vertical discrepancies. At the treatment planning stage, as the clinician gets involved into an important process of reexploration of the available relevant diagnostic information, several critical factors must be considered.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses