4 Infected Sites
Early in the history of implant dentistry, clinicians recommended a waiting period of 6 months following an extraction prior to the insertion of an endosseous dental implant into the edentulous site (Adell, Lekholm, et al. 1981). As discussed in the chapter on extraction site healing, this waiting period frequently results in a significantly resorbed alveolar process and can influence the ideal positioning of dental implants (Iasella, Greenwell, et al. 2003). The evolution of the immediate placement technique provided a safe and efficient method of treatment that eliminated the 6-month waiting period, maintained the alveolar housing, decreased surgical time and procedures, reduced cost and improved acceptance for the patient, and potentially provided better axial alignment, esthetics, and biomechanical prosthetics (Lazzara 1989; Parel and Triplett 1990; Shanaman 1992; Werbitt and Goldberg 1992; Schultz 1993; Watzek, Haider, et al. 1995; Missika, Abbou, et al. 1997). Despite these advantages, immediate implant placement may be considered to have several contraindications. These perceived contraindications include intimate contact to anatomical structures such as the mandibular canal, maxillary sinuses, or nasal cavity; bone loss to the root apex; inability to obtain primary stability or primary flap closure; and the presence of periodontal disease, periapical lesions, or purulent exudate (Block and Kent 1990; Wilson 1992; Arlin 1993; Rosenquist and Grenthe 1996; Grunder, Polizzi, et al. 1999; Polizzi, Grunder, et al. 2000). This last consideration, the question of whether or not an infected site contraindicates immediate implant placement, has engendered the most controversy and remains an ongoing discussion in the literature today.
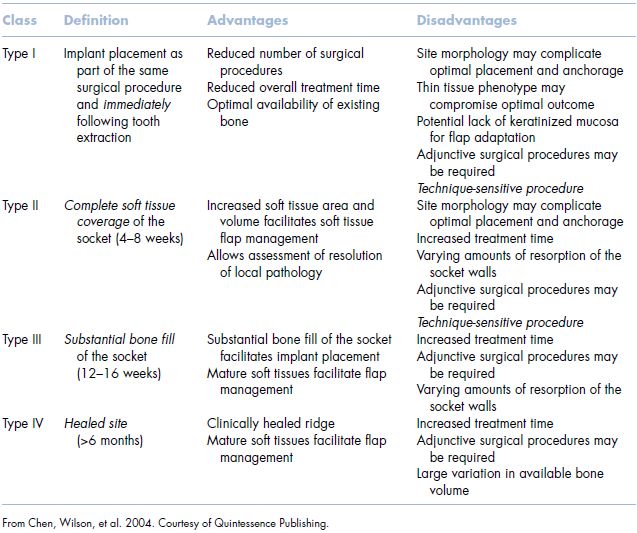
Most recently, Chen and colleagues published a report classifying implant placement protocol based on morphological, dimensional, and histologic changes that occur following tooth loss (Table 4.1) (Chen, Wilson, et al. 2004). Each classification type from I to IV offers advantages and disadvantages to treatment timing, with the evaluation of the site to ultimately be critical in the determination of treatment modalities. One significant aspect of placement timing with this classification system concerned the presence of infection at the time of tooth extraction. It was concluded that the T-1 approach (immediate placement) should not be utilized in the presence of infection. Rather, these authors recommended that the surgeon select a T-2 (early) or T-3 (delayed) protocol to achieve a more predictable outcome. This, Chen and colleagues argued, posed less risk regarding both osseointegration and ideal esthetic outcome.
Table 4.1 Implant timing classification table.
The placement of immediate dental implants in the presence of a periapical or periodontal infection has been contraindicated by other authors as well. Notably, these publications primarily focus their argument on human case reports (Lundgren and Nyman 1991; Tolman and Keller 1991; Werbitt and Goldberg 1992; Rosenquist and Grenthe 1996; Grunder, Polizzi, et al. 1999; Rosenberg, Cho, et al. 2004; Wagenberg and Froum 2006). Also of note, these studies utilized machine-screw implants and ePTFE membranes, while showing a lower success rate and higher incidence of post-operative infections.
Contrary to these reports, others have shown both with animal studies and human trials that experimentally induced periodontal or periapical lesions did not affect the ability for implants to predictably osseointegrate (Table 4.2) (Novaes and Novaes 1995; Novaes, Vidigal, et al. 1998; Marcaccini, Novaes, et al. 2003; Novaes, Marcaccini, et al. 2003; Novaes, Papalexiou, et al. 2004; Papalexiou, Novaes, et al. 2004). Case reports as well as prospective randomized controlled studies in humans with periapical lesions have shown success rates of 92–100%. Siegentholer et al. treated seventeen patients consecutively having periapical lesions using immediately placed roughened surface implants (Siegenthaler, Jung, et al. 2007). In this study, GBR using deproteinized bovine bone and a resorbable collagen membrane was utilized in treating the apical fenestrations and HDD. All implants were loaded at 3 months and observed for 12 months with a 100% success rate. These authors concluded that a critical aspect of the treatment was assessing the diameter of the periapical lesion. If the lesion exceeded the diameter of the planned implant, then there was a need to obtain primary stability in an apical direction. In these situations, the use of CT diagnostics to view the root morphology and osseous lesion may assist the clinician in treatment planning for either an immediate or delayed placement protocol.
A series of animal studies involving the placement of immediate implants in the dog model with periodontal disease also indicated that chronic infection should not be a contraindication for this treatment method. In one study reported by Novaes et al. (2003), five dogs were treated using a split mouth design in which one quadrant served as a control, and the other quadrant underwent ligature-induced periodontitis. After 3 months, the mandibular premolars were removed in both sites, and implants having a roughened surface were immediately placed. The animals were sacrificed after a healing period of 12 weeks, and the specimens were analyzed histologically. Both test and control groups showed good bone-to-implant contact with a percentage of 66% and 62.4%, respectively. This difference was found to be statistically insignificant. The authors concluded that periodontally infected sites may not be a contraindication for immediate dental implants if adequate pre- and post-operative care is taken, such as the use of broad spectrum antibiotics, thorough plaque control, achievement of primary stability, and the selection of appropriate biomaterials.
SUMMARY
A significant quantity of literature has been published pertaining to the placement of immediate dental implants; however, there is a paucity of peer-reviewed articles, by comparison, related to immediately placed dental implants into infected sites. Nearly all reports contraindicating this technique are human case reports that have employed similar treatment modalities, namely machined implant surfaces and ePTFE membranes. By today’s standards, both of these biomaterials are considered outdated, having been replaced with roughened surfaced implants and bioresorbable membranes posing less risk to the patient, increased predictability, and fewer complications. A number of evidence-based animal and human studies indicate immediate implants having a roughened surface and utilizing collagen membranes when necessary, placed in extraction sockets exhibiting either periodontal or periapical lesions, do not lead to an increased rate of complications and can have similar success rates as those placed in non-infected areas. Of primary concern is the ability to achieve primary mechanical stability at the time of placement by engaging bone apically or along the lateral walls of the extraction site. Treatment planning for immediately placed dental implants in infected sites should assess esthetic risk factors as described by Morton et al. to minimize or prevent unfavorable outcomes (Morton, Martin, et al. 2004). The availability of CT radiography may offer the clinician greater insight to treatment planning these cases for immediate versus delayed placement especially in situations where the ability to achieve primary stability is in question (Figures 4.1–4.62).
Table 4.2 Infected site immediate placement.
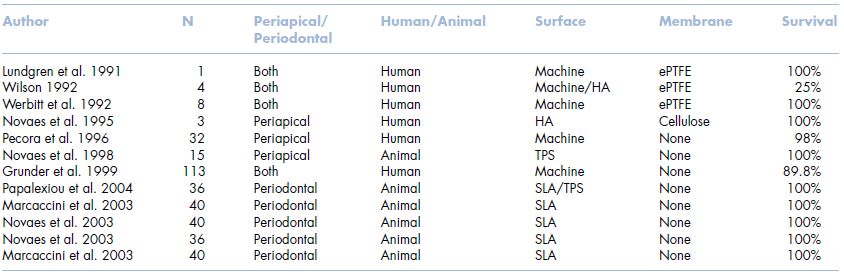
Figure 4.1 Buccal view pre-op tooth #9—note fistula.

Figure 4.2 Pre-op radiograph tooth #9.

Figure 4.3 Occlusal view pre-op tooth #9.

Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


