Rationale for Periodontal Treatment
What Does Periodontal Therapy Accomplish?
The effectiveness of periodontal therapy is made possible by the remarkable healing capacity of the periodontal tissues. Periodontal therapy can restore chronically inflamed gingiva so that, from a clinical and structural point of view, it is almost identical with gingiva that has never been exposed to excessive plaque accumulation1 (see Part 8).
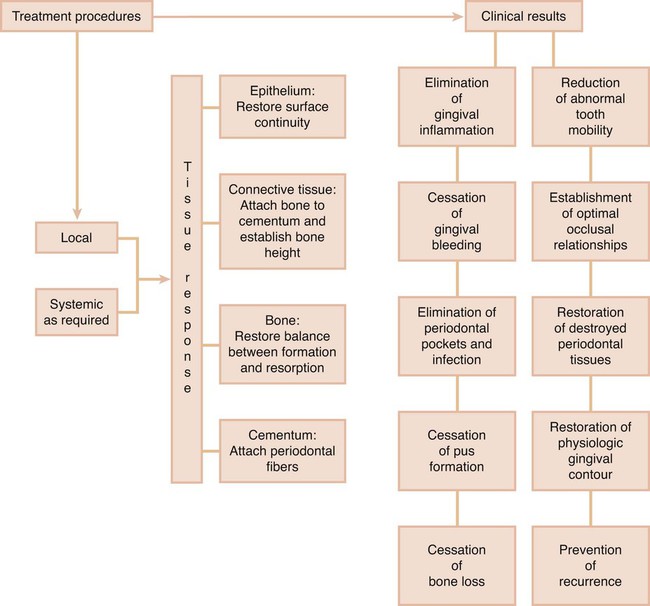
Properly performed, periodontal treatment can eliminate pain, exudate, gingival inflammation,2 and bleeding. It can also reduce periodontal pockets, eliminate infection, arrest the destruction of soft tissue and bone,3 and reduce abnormal tooth mobility.4 Other benefits are to establish optimal occlusal function, restore tissue destroyed by disease, reestablish physiologic gingival contour, and prevent the recurrence of disease, which will all help to maintain the natural dentition5 (Figure 34-1).
Local Therapy
Abnormal forces on the tooth can increase tooth mobility. The thorough elimination of plaque and the prevention of its formation can help maintain periodontal health, even if traumatic forces are allowed to persist.6, 7 However, the elimination of trauma may increase the chances for bone regeneration and the gain of attachment.8 Although this point is not widely accepted,9 it appears that creating occlusal relationships that are more tolerable to the periodontal tissues increases the margin of safety of the periodontium to the buildup of plaque, in addition to reducing tooth mobility. It should be remembered that total plaque elimination as obtained in experimental studies may not be possible in human subjects.
Systemic Therapy
Systemic therapy may be employed as an adjunct to local measures for specific purposes such as controlling systemic complications from acute infections or chemotherapy and preventing harmful effects of posttreatment bacteremia. The control of systemic diseases that aggravate the patient’s periodontal condition is always a consideration so proper precautions can be instituted during therapy (see Chapters 37, 38, and 39).
Systemic therapy for treatment of the periodontal condition in conjunction with local therapy is indicated in patients with aggressive periodontitis. In these diseases, systemic antibiotics are used to eliminate the bacteria that invade the gingival tissues and can repopulate the pocket after scaling and root planing (see Chapters 40 and 47).
In addition, periodontal manifestations of systemic diseases (see Chapter 28) are treated primarily by other local measures.
In the late twentieth century, the concept of host modulation was introduced as a medical approach to periodontal treatment. The classic 1979 paper by Nyman, Schroeder, and Lindhe10 reported that it was possible to block periodontal bone loss in animals with the aspirin-like drug indomethacin. Evidence was then presented that some nonsteroidal antiinflammatory drugs (NSAIDs), such as flurbiprofen and ibuprofen, can reduce the development of experimental gingivitis,11 as well as the loss of alveolar bone in periodontitis.12–15 These drugs are propionic acid derivatives and act by inhibiting the cyclooxygenase pathway of arachidonic acid metabolism, thereby reducing prostaglandin formation. These NSAIDs can be administered by mouth16 or applied topically.13
Another drug that has a strong inhibitory effect on bone resorption is alendronate, a bisphosphonate, which is currently used to treat metabolic diseases in humans, such as Paget disease or hypercalcemia of malignancy, which result in bone resorption. Experimental studies in monkeys have shown that alendronate reduced the bone loss associated with periodontitis.17,18
Host modulation is still in its experimental stages, and protocols for its clinical use have not been established. However, current studies indicates that future treatment modalities may attempt not only to control the bacterial cause of the disease but also to suppress the self-destructive components of the host inflammatory response12 (see Chapter 49).
Factors That Affect Healing
In the periodontium, as elsewhere in the body, healing is affected by local and systemic factors.
Local Factors
Healing is improved by debridement (removal of degenerated and necrotic tissue), immobilization of the healing area, and pressure on the wound. The cellular activity in healing entails an increase in oxygen consumption, but healing of the gingiva is not accelerated by artificially increasing the oxygen supply beyond the normal requirements.19
Systemic Factors
The effects of systemic conditions on healing have been extensively documented in animal experiments but are less clearly defined in humans. Healing capacity diminishes with age,20,21 probably because of the atherosclerotic vascular changes common in aging and the resulting reduction in blood circulation. Healing is delayed in patients with generalized infections and in those with diabetes and other debilitating diseases.
Healing is impaired by insufficient food intake; bodily conditions that interfere with the use of nutrients; and deficiencies in vitamin C,22,23 proteins,24 and other nutrients. However, the nutrient requirements of the healing tissues in minor wounds, such as those created by periodontal surgical procedures, are usually satisfied by a well-balanced diet.
Healing is also affected by hormones. Systemically administered glucocorticoids such as cortisone hinder repair by depressing the inflammatory reaction or by inhibiting the growth of fibroblasts, the production of collagen, and the formation of endothelial cells. Systemic stress,25 thyroidectomy, testosterone, adrenocorticotropic hormone (ACTH), and large doses of estrogen suppress the formation of granulation tissue and impair healing.20 Progesterone increases and accelerates the vascularization of immature granulation tissue26 and appears to increase the susceptibility of the gingiva to mechanical injury by causing dilation of the marginal vessels.27
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses