Pulp Therapy for the Young Permanent Dentition
The Dentin-Pulp Complex Concept
Vital Pulp Therapy for Teeth Diagnosed with Normal Pulp or Reversible Pulpitis without Pulp Exposure
Vital Pulp Therapy for Teeth Diagnosed with Normal Pulp or Reversible Pulpitis with Pulp Exposure
The Dentin-Pulp Complex Concept
The most important, and most difficult, aspect of pulp therapy is determining the health of the pulp or its stage of inflammation. Consequently, an intelligent decision regarding the best form of treatment can be made. Permanent teeth in children and adolescents have a more cellular pulp with better healing potential than in adults,1 and their degree of root development will affect the treatment plan.
Immature permanent teeth are those in which root development and apical closure have not been completed. These teeth can be present in children from 6 years of age until 3 years after the eruption of the third molars. After apical closure, these teeth are classified as mature teeth. It should be kept in mind that the apposition of secondary dentin in the pulp chamber and the root canal is a continuous process. Physiologic secondary dentinogenesis represents the deposition of dentin after completion of the crown and root formation. It continues, at a much slower rate, throughout the life of the tooth.2 It is extremely important to maintain pulp vitality whenever possible, because young permanent teeth have wide root canals, and dentin apposition can prevent fracture. Root fracture is a common finding after traumatic injury in endodontically treated teeth with wide root canals.3 The aim of all treatment planning for young permanent teeth is to preserve pulp vitality, providing conditions for continuous root development and physiologic dentin apposition. The pulp and the dentin are closely related and are usually looked upon as one unit, the pulp-dentin complex.4 All procedures performed in the dentin will have an effect on the pulp.
Reactions to Caries and Operative Procedures
The molecular and cellular changes that take place during primary dentinogenesis are mimicked during the dentin-pulp reactions to injury. Kuttler5 proposed the concept of tertiary dentin formation, encompassing a wide range of responses, from the secretion of a regular, tubular dentin to a very dysplastic atubular dentin. These responses are the result of different cellular and molecular processes, and they express reactions ranging from mild to severe stimulus. Tertiary dentin has been classified as either reactionary or reparative dentin, the former being secreted by surviving postmitotic odontoblasts in response to a mild stimulus. Reparative dentin is secreted by a new generation of odontoblast-like cells differentiated after the death of the original postmitotic odontoblasts.2
The dentin matrix is considered to be a reservoir of growth factors and cytokines sequestered during dentinogenesis. During caries progression these molecules may be released from the dentin degraded by bacterial acids with other components of the extracellular matrix, inducing the formation of reactionary dentin.6 Some of the bioactive molecules are transforming growth factor β1 (TGF-β1), fibroblast growth factors (FGFs), and epidermal growth factors (EGFs). These chemotactants are hypothesized to provide the signals involved in the recruitment, proliferation, and differentiation of the cells to the site of pulp injury to initiate tissue regeneration and dentin bridge formation.
Reparative dentinogenesis encompasses a complex sequence of biological events, involving stem/progenitor cells recruitment and differentiation before matrix secretion at the site of the injury. It was demonstrated in a few in vivo studies that ethylenediamine tetraacetic acid (EDTA) solubilized dentin matrix components, shows morphogenetic activity, and can induce reparative dentinogenesis.7
In addition to the caries process, various factors associated with the method of cavity preparation and restoration can influence the tertiary dentin response. The size of the cavity, the residual dentin thickness (RDT), the etching of the cavity, the type and method of application of the restorative material, have an effect on the type and quality of the tertiary dentin. Several studies have reported that the alterations in the pulp related to the previously mentioned factors are more important than those related to the restorative materials.8–11 RDT is apparently the most significant factor determining the secretion of reactionary dentin. Maximal reactionary dentin was observed in a study where the RDT in the cavities was between 0.5 mm and 0.25 mm. Reduced reactionary dentin and reduced odontoblastic survival were observed in teeth with an RDT less than 0.25 mm. 11 In these deep cavities, little more than 50% of the odontoblasts survived, whereas in shallow cavities, odontoblastic survival was about 85% or greater. Despite the cutting of the odontoblastic process, the cells responded by secreting reactionary dentin.
Clinical Pulpal Diagnosis
Patient History
Medical and dental history should always be carefully documented. In order to make the most accurate diagnosis, information must be obtained from several sources, with thorough clinical and radiographic examinations. Belanger12 refers to the importance of assessing the type of pain described by the child, whether it is spontaneous or is precipitated by a stimulus. Sensitivity to pressure may indicate that the pulpal inflammation has extended to the periodontal ligament. However, this sensitivity may also be the result of a much more innocuous situation such as a sealant placed in excess or a high restoration causing hyperocclusion.12 Children often complain of “toothaches” during the eruption of the first permanent molars. In these cases the dentist should carefully ascertain whether the complaint is due to a pericoronitis or to biting on an operculum, rather than to pain resulting from a pulp condition. Food impaction can also mimic the symptoms of an irreversible pulp condition. In cases of trauma, both patient and parents should be asked about the timing and nature of the injury, and whether previous treatment or traumatic incidents have occurred.
Clinical Examination
Both extraoral and intraoral examinations are important for the detection of the pulpally involved tooth. Extraoral examination should focus on swelling, local lymphadenopathy, and extraoral sinus tract. Intraoral examination should focus on the tooth suspected as the origin of pain, but all the teeth on the same side should be inspected carefully, because referred pain can occur. The examination includes observation of the soft tissues for redness, swelling, or sinus tract. Examining tissues by palpation and percussion, determining periodontal involvement, and assessing tooth mobility should follow. Special attention should be paid to fractured restorations or those with marginal breakdown, as these may also be indicators of pulp involvement.13 Composite restorations are especially vulnerable to secondary caries at the gingival margins.14 Additional tests should include thermal and electric pulp test (EPT) of the involved tooth and of an appropriate control tooth. The presence of extraoral or intraoral sinus tract requires the performance of a tracing radiograph in order to trace the origin of the infection.15 When the originating tooth is detected, root canal treatment should be performed. Sensitivity to palpation in the vestibule may be indicative of an acute apical pathologic process. Emphasis should be placed on soft tissue swelling or bony expansion in the area, which may indicate the presence of Garré osteomyelitis.16
Pain to percussion does not indicate the state of the pulp inflammation; rather, it is an indication of inflammation in the periodontal ligament. This inflammation is most often a result of pulp inflammation that extended into the periodontal ligament (PDL) or a sequel of dental trauma.17 Periodontal probing is part of the intraoral examination; bone loss can be a consequence of periodontal or pulpal disease. Increased mobility should be evaluated by comparison with the adjacent and contralateral teeth. Thermal and electric pulp tests are commonly used to test pulp vitality. In young permanent teeth, these tests should be carefully interpreted, as immature teeth may not react to stimulation because of the incomplete development of the innervation system.18,19
Pulp diagnosis is based upon clinical examination and cannot be verified histologically. For practical reasons the state of the pulp is classified as reversible (treatable) or irreversible (untreatable) pulpitis.20 Diagnosis of reversible pulpitis indicates that the inflammation should resolve and vital pulp therapy is a potential treatment option. Treatment options range from indirect pulp treatment, to direct pulp capping, to partial or cervical pulpotomy. It depends on the progress of the inflammatory process within the pulp and the degree of root development. Clinically, the difference between reversible and irreversible pulpitis is frequently determined on the basis of the duration and intensity of the pain. Prolonged response to cold stimuli, spontaneous pain, or referred pain will lead to a diagnosis of irreversible or untreatable pulpitis; these teeth will need root canal treatment.
Vital Pulp Therapy for Teeth Diagnosed with Normal Pulp or Reversible Pulpitis without Pulp Exposure
Caries Excavation and Protective Liner
The progress of a carious lesion into the dentin begins with acid demineralization produced by bacteria, followed by a more extensive tissue breakdown caused by bacterial enzymatic activity. The demineralized dentin has been referred to as “affected dentin,” and the broken-down part is known as “infected dentin.”21 It has been suggested that during caries excavation only the infected dentin should be removed, the affected dentin being left permanently. Clinically, it is difficult to differentiate between the different layers of carious dentin. As a practical approach, the remaining dentin should feel hard when examined with an explorer.4
A chemical-mechanical approach to caries excavation using dyes has been developed. With this method, sound and carious dentin are clinically separated, and only carious dentin can be removed, resulting in a more conservative preparation. When a bur is used, healthy tissue is frequently removed. It has also been reported that this method contributes to patient comfort, as it has been said to be painless, requiring less drilling and local anesthesia. The main drawback of this technique is the time needed to complete the procedure, because it is much more time-consuming than the use of a bur.22
The American Academy of Pediatric Dentistry (AAPD)23 recommends placement of a protective barrier on the floor of the preparation between the restorative material and the pulp-dentin complex. A protective barrier is recommended in deep preparations, and the preferred materials are glass ionomer cements or calcium hydroxide liners. There is sufficient evidence to show that pulp reaction to dental materials is transitory, and overt inflammation occurs only after bacteria or their by-products have reached the pulp.24–26 When bacteria and bacteria-produced irritants have been removed by caries excavation and a bacteria-tight restoration has been placed, new bacteria are prevented from reaching the deeper portion of the dentin, and the inflamed pulp will have a great opportunity to heal.
Indirect Pulp Treatment
The main objective of indirect pulp treatment is to maintain the vitality of teeth with reversible pulp injury or teeth with deep caries that might otherwise need endodontic therapy if the decay was completely removed (AAPD).23 The rationale for this treatment is based on the observation that postmitotic odontoblasts can be induced to upregulate their secretory activities in response to reduced infectious challenge.27 This results in the deposition of tertiary dentin, which increases the distance between the affected dentin and the pulp, and in the deposition of peritubular (sclerotic) dentin, which results in decreased dentin permeability.
Clinically, indirect pulp treatment is defined as the procedure in which nonmineralizable carious tissue is removed, and a thin layer of caries is left at the deepest site of the cavity to prevent pulp exposure.25,28 It is important to remove the carious tissue completely from the dentinoenamel junction and from the lateral walls of the cavity to achieve optimal interfacial seal between the tooth and the restorative material, thus preventing microleakage. Several clinical studies have demonstrated a high percentage of success utilizing this technique.29–32 The indication for indirect pulp treatment should be limited to teeth without signs of irreversible pulpitis. In this procedure, the deepest layer of the remaining carious dentin should be covered with a liner. The materials used for these procedures are calcium hydroxide liners and glass ionomer liners, with good results in clinical studies.29–32
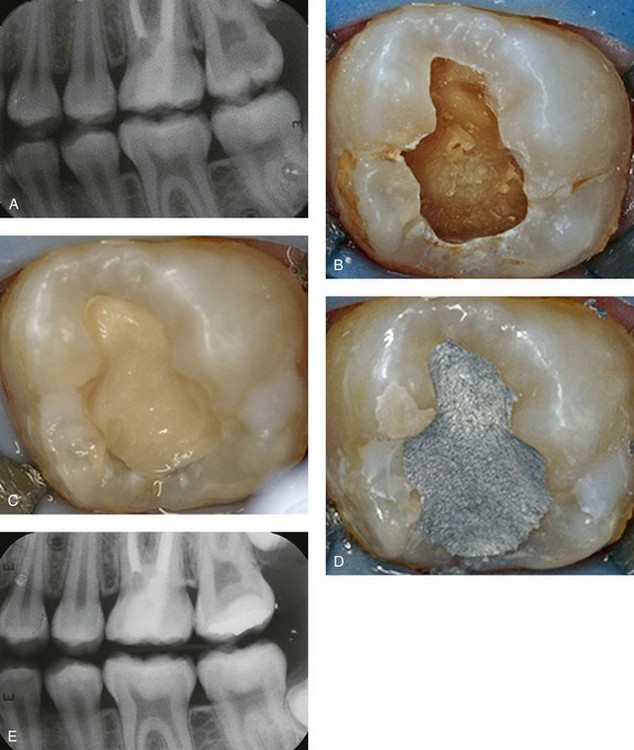
The dilemma lies in the assessment of how much caries to leave at the pulpal or axial floor. The carious tissue that should remain at the end of the cavity preparation is the quantity that, if removed, would result in overt exposure. In case of doubt, deep carious lesions may be managed by stepwise excavation performed in two visits that may result in fewer pulp exposures compared with direct complete excavation. At 1-year follow-up, there was a statistically significant higher success rate with stepwise excavation than with one-visit treatment. 33,34 At present, there is enough evidence of good clinical and radiographic success without reentering, if the restoration is maintained leakage free.35–37 Both approaches require knowledge of tooth anatomy, clinical experience, and a good understanding of the process of caries progression. If the tooth is too broken down to allow for a proper restoration, placement of a crown should be considered. Figure 33-1 demonstrates the indirect pulp treatment technique using a calcium hydroxide liner.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


 Outline
Outline FIGURE 33-1
FIGURE 33-1