32 POSTOPERATIVE CARE
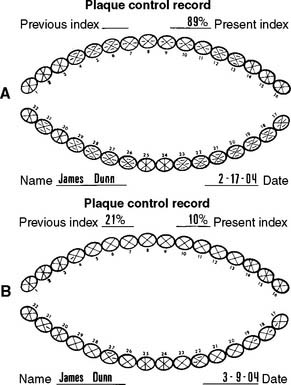
After placement and cementation of a fixed dental prosthesis (FDP), patient treatment continues with a carefully structured sequence of postoperative appointments designed to monitor the patient’s dental health (Fig. 32-1), stimulate meticulous plaque control habits, identify any incipient disease, and introduce whatever corrective treatment may be needed before irreversible damage occurs.
Patients should be instructed in special plaque-control measures, especially around pontics and connectors, and the use of special oral hygiene aids such as floss threaders (Fig. 32-2). If the pontics are properly designed (see Chapter 20), floss can be looped through the embrasure spaces on each side, and the loop can be pulled tightly against the convex pontic tissue surface. A sliding motion is then used to remove dental plaque (Fig. 32-3). Flossing under pontics is essential for improving prosthesis longevity. When dental floss is used, the mucosa beneath pontics remains healthy; without it, mild or moderate inflammation results.1 Tissue response has been shown to be independent of the pontic material.2

Fig. 32-3 The patient should be instructed in the use of floss to clean partial fixed dental prostheses.
Detecting disease around an FDP can be extremely difficult at a stage when corrective treatment is still relatively simple. For instance, partial dissolution of the luting agent may be difficult to diagnose with a subgingival margin. Caries is often detected only after irreversible pulp involvement has resulted. Caries under a crown is more difficult to detect radiographically, although bitewing images provide some information interproximally. Follow-up studies on patients with FDPs reveal that identifying risk factors and predicting the development of caries in any particular patient are complicated. However, there is no indication that caries is more likely in association with prostheses than on unrestored teeth.3
POSTCEMENTATION APPOINTMENTS
To enable the dentist to monitor the function and comfort of the prosthesis and to verify that proper plaque control has been mastered by the patient (Fig. 32-4), an appointment is generally scheduled within a week to 10 days after the cementation of an FDP. The dentist should check carefully that the gingival sulcus remains clear of any residual luting agent that may have been overlooked previously and that all aspects of the occlusion remain satisfactory.
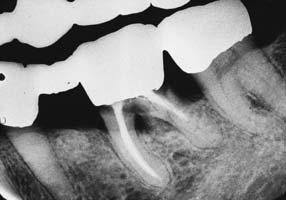
Radiolucent cements should be avoided because detecting excess luting agent radiographically is impossible if that material is effectively radiolucent. As luting agent radiopacity increases, excess cement is spotted more easily on routine radiographs; therefore, the dentist should choose a luting agent that is as radiopaque as possible. In practice, luting agents are available in a wide range of radiopacities.4–6 Figure 32-5 summarizes data from these studies.
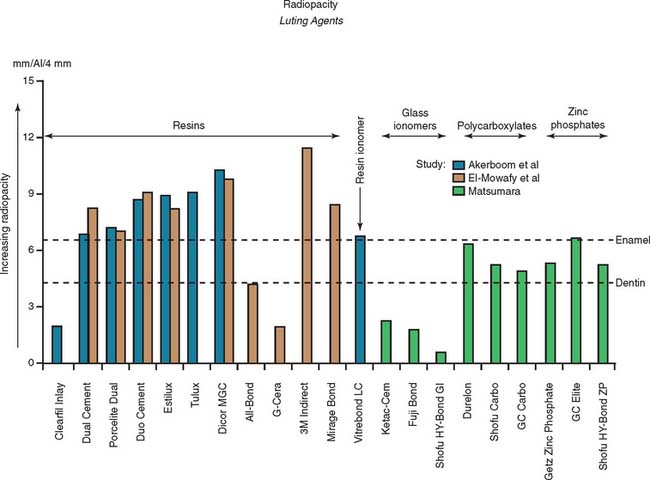
Fig. 32-5 Radiopacity of luting agents. In three in vitro studies,4–6 investigators compared the radiographic appearance of various luting agents to aluminum. The data were normalized to account for different specimen thicknesses used by the investigators. Excess luting agent is more difficult to detect if materials with lower values are chosen. In addition, margin gaps and recurrent caries are more difficult to diagnose.
The presence of fremitus (see Chapter 1) or “polished” facets on the occluding surfaces of cast restorations at the postcementation appointment should prompt a careful reassessment and correction of the occlusion. If any minor shift in tooth position has occurred, some occlusal adjustment may be necessary. If so, the patient is rescheduled to visit the following week to ensure that no further correction is needed.
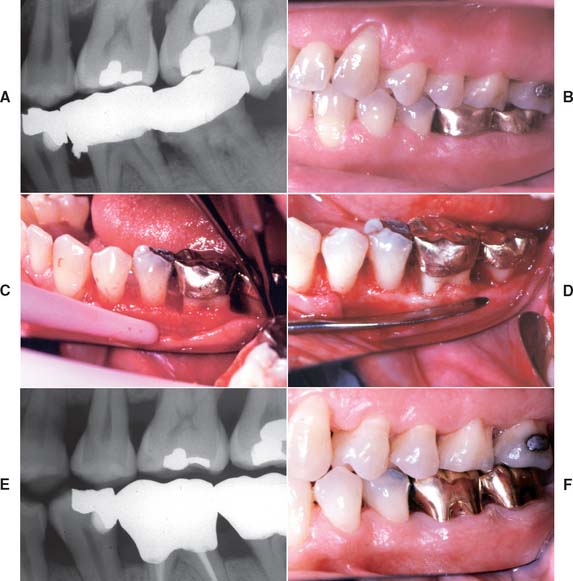
PERIODIC RECALL
Patients with cast restorations should attend recall visits at least every 6 months. Less frequent recall may lead to oversight of recurrent caries or the development of periodontal disease. Patients who have been provided with extensive fixed prostheses (Fig. 32-6) need more frequent recall appointments, particularly when advanced periodontal disease was present. The appointments can be coordinated by the restorative dentist or the periodontist. To ensure treatment continuity, it is imperative to establish in advance who will assume primary responsibility for coordinating recall appointments.

Fig. 32-6 Patients who have received extensive treatment of this nature require more frequent follow-up care.
History and General Examination
The patient’s medical history should be reviewed and updated at least annually. The patient should be examined according to the principles introduced in Chapter 1. Particular attention is paid to the soft tissues, because early signs of oral cancer may be detected at a recall appointment.
Oral Hygiene, Diet, and Saliva
Patients tend to become somewhat less diligent in their plaque control efforts when the active phase of their treatment is completed. The dentist should look carefully for any signs of deterioration in oral hygiene and assess the general effectiveness of plaque control at every recall with an objective index (Fig. 32-7). Deficiencies must be identified early, and corrective therapy should be initiated. The dentist should ask about changes in diet, particularly increased sugar consumption or “fad” diets. Excessive weight loss or gain should also be investigated. For instance, a patient who has recently stopped smoking may start ingesting large amounts of candy, which can result in an increase in dental caries.
Saliva plays an important role in caries development. Patients with xerostomia can rapidly develop extensive carious lesions.7 Diagnosing the cause of reduced saliva is imperative; the origin is often a drug side effect.8
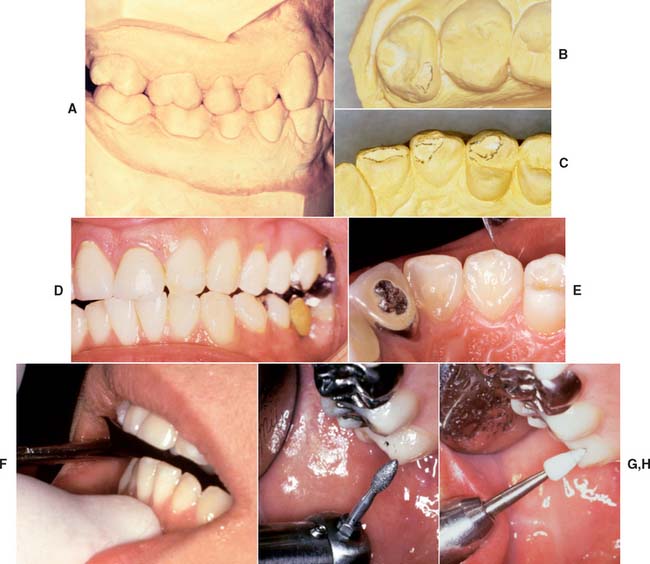
Dental Caries
Dental caries (Fig. 32-8) is the most common cause of failure of a cast restoration.9–12 Detection can be very difficult,13 particularly where complete coverage is used. At each appointment, the teeth should be thoroughly dried and visually inspected (Fig. 32-9). The explorer must be used very carefully when early enamel lesions are assessed, because a heavy-handed examination may damage the fragile demineralized enamel matrix. An intact enamel matrix is essential for procedures that induce remineralization14 (e.g., improved plaque control, dietary changes, topical fluoride applications).

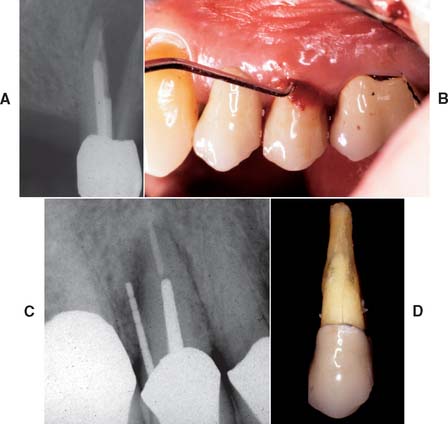
Fig. 32-8 Undetected caries beneath this partial fixed dental prosthesis resulted in serious complications.
Conservative treatment of caries at the cavosurface margin is especially problematic. The lesion can spread rapidly, particularly if the restoration has a less than optimal marginal fit. Correcting the problem with a small amalgam, composite resin, or glass ionomer restoration is sometimes possible (Fig. 32-10). If the cast restoration is supported by an amalgam or composite resin core, the extent of the caries may be difficult to determine. When there is doubt that all carious dentin has been removed, replacing the entire restoration is recommended.
Root caries
Caries of exposed root surfaces (Fig. 32-11) can be a severe problem in the age group commonly seeking fixed prosthodontic care.15–17 In the classic Vipeholm study,18 root caries accounted for more than 50% of new lesions in patients in the 50-year-old age group. Root caries incidence increased considerably with age.19 In the caries examination from phase 1 of the Third National Health and Nutrition Examination Survey, root caries affected 22.5% of the dentate population.20 Root surface caries seems to be associated with individual dental plaque scores and high counts of salivary Streptococcus mutans.21 Xerostomia that is age-related or caused by medication or radiation treatment has been implicated in the etiology of rampant caries.22–24 Other factors include the patient’s economic status, diet, oral hygiene, and ethnic background.25 Only a most vigorous effort on the part of the dentist and patient leads to resolution of the problem. Prevention is focused on diet counseling and fluoride treatment. Treatment often requires the placement of large cervical glass ionomer or amalgam restorations that wrap around the periphery of previously placed cast restorations. Such restorations are difficult to place. However, in view of the constraints, they are a preferred alternative to comprehensive re-treatment with elaborate fixed prostheses.
Periodontal Disease
Unfortunately, periodontal disease often occurs after placement of fixed prostheses,26 especially where the cavosurface margin has been placed subgingivally27–29 or the prosthesis is overcontoured.30 Inflammation is more severe with poorly fitting restorations31 (Fig. 32-12), but even “perfect” margins have been associated with periodontitis.32 At recall appointments, particular attention is given to sulcular hemorrhage, furcation involvement, and calculus formation as early signs of periodontal disease. Improperly contoured restorations should be recontoured or replaced.
Occlusal Dysfunction
The patient is examined for signs of occlusal dysfunction at each recall appointment. The patient should be asked about any noxious habits such as bruxism. An examination of the occlusal surfaces may reveal abnormal wear facets (Fig. 32-13). In particular, the canines should be inspected, because wear in this area soon leads to other excursive interferences. If a patient engages in parafunctional activity that causes tooth wear, the progression of facet formation often begins on the canines. In a slightly more advanced state of wear, additional facets can be observed on the incisor teeth, after which excursive interfering contacts result in wear facets on the posterior teeth. Abnormal tooth mobility is investigated, as is muscle and joint pain. A standardized muscle-and-joint palpation technique (see Chapter 1) is helpful. Articulated diagnostic casts should be periodically remade (Fig. 32-14) and compared with previous records so that any occlusal changes can be monitored and corrective treatment initiated.
A small number of patients may not have responded well to previous occlusal treatment or may resume parafunctional activity some time after completion of the active phase of fixed prosthodontic treatment. Although resolving the underlying etiology is preferable, a nightguard can occasionally be prescribed (Fig. 32-15). Its design is identical to that of the occlusal device described in Chapter 4 for treating neuromuscular symptoms resulting from malocclusion. However, the device is worn only at night. If the patient primarily clenches, the dentist should consider a slightly flatter anterior ramp than is ordinarily incorporated in the conventional device.
Pulp and Periapical Health
One advantage of partial-coverage restorations is that pulp health can be monitored with an electric pulp tester (Fig. 32-16), although the vitality of any tooth with a complete crown can still be assessed by thermal means. Correlating the histologic condition of a pulp directly with the patient’s response to pulp testing is difficult.33 Therefore, such results should be combined with other clinical data that result from careful patient history documentation and examination. Seeking the opinion of an endodontist is often advisable (Fig. 32-17). Radiographs provide useful information about the presence of periapical pathosis. Teeth with fixed restorations should be reviewed radiographically every few years. The use of a standardized technique enables the dentist to make an objective comparison with previous films. Although some studies have shown a high incidence of periapical disease associated with fixed prostheses,34,35 other studies have shown a low incidence of this complication.29,36,37
EMERGENCY APPOINTMENTS
Pain
A patient presenting with pain should be asked about its location, character, severity, timing, and onset. Factors that precipitate, relieve, or change the pain should be investigated, and appropriate treatment measures should be initiated (see Chapter 3).
If the patient has several endodontically treated teeth that have been restored with posts and cores and with fixed prostheses, the possibility of root fracture should be considered, especially for teeth that were internally weakened as a result of endodontic treatment in conjunction with oversized posts of suboptimal length. If a fracture has occurred, the tooth is almost invariably lost, which can significantly complicate follow-up treatment, especially if it involves an abutment tooth for an FDP (Fig. 32-18).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses