27 FIBER-REINFORCED COMPOSITE FIXED PROSTHESES
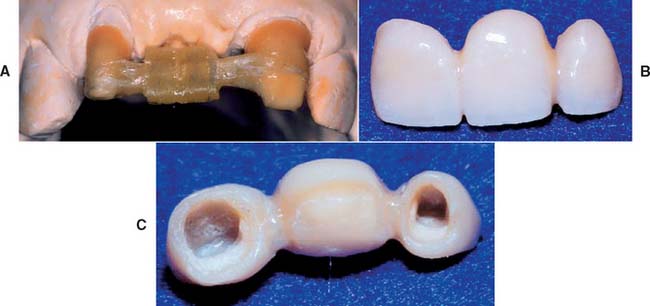
Fiber-reinforced fixed prostheses are an innovative alternative to traditional metal-ceramic restorations. They should be considered for certain patients because they provide a conservative approach to replacing missing teeth and overcome some of the drawbacks of conventional prostheses. The restoration consists of a fiber-reinforced composite (FRC) substructure veneered with a particulate composite material. The substructure provides strength, and the veneer, because it is laboratory processed, exhibits better physical properties and esthetics than do direct placement composite restoratives (Fig. 27-1). The following topics are included in this chapter:
ADVANTAGES AND DISADVANTAGES
As discussed in Chapter 24, the most common fixed prostheses are composed of a metal substructure veneered with a ceramic material. The substructure provides mechanical integrity, whereas the ceramic imparts the necessary esthetics. The metal-ceramic prosthesis has an excellent clinical service record but continues to exhibit several drawbacks. Although the metal substructure is strong and durable, there are biologic concerns, especially when base metal alloys (commonly used in clinical practice) are selected. They may undergo corrosion1–3 and/or may elicit an allergic reaction from some patients.4–8 Certain constituents of some base metal alloys may cause acute and chronic health hazards for laboratory personnel.9,10 In addition, the metal framework is opaque with a dark oxide layer, which is not esthetically pleasing. This must be covered with a porcelain veneer to produce a lifelike appearance.
Porcelain is a brittle material and can fracture, which is a leading cause of restoration failure.11–14 When this occurs, porcelain can sometimes be repaired with acrylic or composite resin15–18 bonded with silane coupling agents or 4-methacryloxyethyl-trimellitic anhydride (4-META) to promote adhesion (see Chapter 32). Porcelain is also abrasive to opposing enamel and can severely damage unrestored opposing teeth.19–23 Porcelain has been implicated in severe occlusal wear, particularly when it is not glazed or highly polished (see Chapter 19). In one survey, less wear on opposing teeth was cited as the single major need for change in posterior tooth-colored crowns.24
Because of these problems and concerns, alternatives to metal-ceramic materials continue to be explored. All-ceramic and all-particulate composite prostheses have been described in the dental literature.25,26 Recorded problems include low resilience and toughness, which result in clinical failure.
As with the porcelain surfaces of metal-ceramic prostheses, the surfaces of the all-ceramic prostheses are abrasive to tooth enamel and can potentially damage unrestored opposing teeth. Conversely, the composite materials have historically exhibited less than adequate occlusal wear resistance and color stability over time, but newer composites continue to improve with regard to these characteristics. Light-, heat-, and vacuum-polymerized laboratory-processed particulate composite materials are now commercially available and are made of new polymer formulations with improved filler particle distribution.27 These improved materials demonstrate better physical properties, such as hardness and wear resistance. However, particulate composites are brittle and need the support of a substructure with good flexure properties.
FRCs have good flexure strength and other physical characteristics that make them suitable fixed prosthesis substructure materials.28–30 In addition, the FRC substructure is translucent and requires no opaque masking. This allows a relatively thin layer of particulate covering composite and excellent esthetics. FRCs have been used to make two-phase all-polymer prostheses composed of an internal glass fiber–reinforced composite substructure covered by a particulate composite (Fig. 27-2).
AVAILABLE MATERIALS
FRC materials are categorized according to the following characteristics:
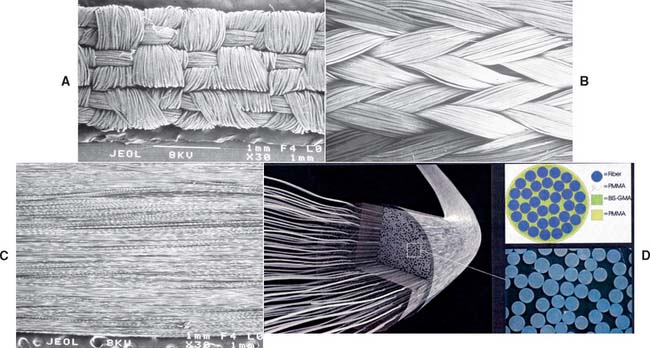
The most commonly used fibers in dental applications are glass, polyethylene, and carbon. Fiber architectures in dentistry include “unidirectional” patterns, in which all fibers are parallel, and braided and woven patterns. Commercially available non–resin-impregnated materials include polyethylene weaves (e.g., Ribbond* and Construct†) and glass weaves (e.g., GlasSpan‡). These products need to have the resin added to the fibers by hand. Resin-preimpregnated materials include everStick and StickNET,§ which are hand formed and available in both unidirectional and woven-glass forms; FibreKor,‖ which is hand formed and available as a unidirectional glass material; and Splint-It,¶ which is also hand formed and available in both unidirectional and woven glass forms (Fig. 27-3).
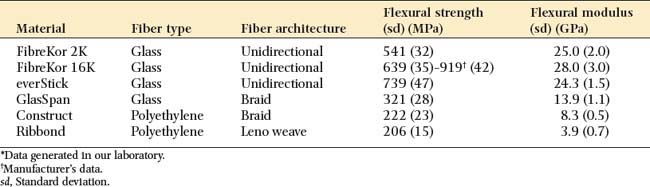
Different FRC materials exhibit different handling and mechanical properties. Fiber type, fiber orientation, and the quality of fiber impregnation with the resin matrix have a substantial effect on handling characteristics and physical properties. As seen in Table 27-1, glass materials with a unidirectional architecture exhibit flexural properties that are superior to the polyethylene materials with a woven or braided architecture. These glass materials have a flexural strength that is more than twice the strength of polyethylene materials and a flexural modulus almost eight times as great.16 Because of their good handling characteristics, the braided and woven polyethylene products may be useful for other dental applications (e.g., operatory fabrication of periodontal splints).
INDICATIONS
Indications for selecting a fiber-reinforced polymer prosthesis include the following:
These materials can be used anywhere in the mouth where esthetics is important. The lack of metal or opaque materials provides good translucency and a very natural appearance. This natural appearance at the cervical aspect of the prosthesis retainer eliminates the need to hide margins subgingivally, where they may create periodontal problems for the patient. Supragingival margins of this polymer prosthesis blend in easily with the nonprepared tooth structure apical to the tooth preparation finish line, just as the overall prosthesis blends in with the adjacent natural teeth. Resin composite luting materials that bond to the internal aspect of the polymer prosthesis retainers and to the dentin and enamel of the abutment teeth improve retention of the prosthesis. This feature may provide crucial retention of a polymer prosthesis on abutment teeth that cannot be made to exhibit optimum geometric retention form; however, the bonding process requires careful control of moisture and soft tissues.
An early prosthodontic application of an experimental thermoplastic unidirectional FRC31–33 was the fabrication of a single tooth replacement bonded fixed dental prosthesis (FDP).34 These prostheses were formed in the laboratory and then bonded to the teeth (Fig. 27-4).
CONTRAINDICATIONS
Contraindications to selecting an FRC fixed prosthesis include the following:
Patient selection criteria are summarized in Box 27-1. Composite resin luting materials and an adhesive cementation technique can be used only in situations in which the operator can maintain a contamination-free field. Rubber dam isolation is ideal and should be used whenever possible. At this time, FDPs that replace more than two teeth are not recommended because the material’s ability to support longer edentulous spans has not been documented. An increased susceptibility to wear or fracture may occur in patients who brux or clench, and surface degradation of the particulate composite is likely to be a problem in alcoholic patients. Because there are no clinical data to substantiate how the FRC fixed prosthesis would perform when subjected to these conditions, it should not be considered until more information is available.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses