Pit and Fissure Sealants
Scientific and Clinical Rationale
In 2006, the Centers for Disease Control and Prevention (CDC) celebrated its 60th anniversary. What began in 1946 as a wartime agency for malaria control has become the nation’s leader in public health in regards to health promotion and prevention. The establishment and growth of such an agency represents the shift in the dogma of health care from simply curative or palliative treatment to increasing emphasis on preventive medicine. In the past several decades, “the power of prevention” perspective has been permeating health care as we have begun to focus on the burdens that chronic diseases leave in their wake—decreased life expectancy, reduced quality of life, and escalating health care costs. Of particular interest to the dental profession is dental caries, a chronic disease affecting more than 90% of adults aged 20 to 64 years.1 Although chronic diseases are among the most common and costly of all health problems, they are also among the most preventable.
Epidemiology of Pit and Fissure Caries
In the past several decades, dramatic improvements in the prevention of caries have occurred due to a multitude of factors: fluoride exposure, enhanced awareness of the benefits of early care, increased access to dental care, and increased financial coverage by insurance companies, group plans, and government-funded programs of preventive and restorative dental procedures for children.2
Despite these efforts, dental caries is still the single most common chronic disease of childhood, more common than asthma and hay fever.3 The facts from the most recent National Health and Nutrition Examination Survey (NHANES) for the years 1999-2004 are arresting1:
• By age 11 years, over 40% of children have had dental caries in their primary teeth, and over 20% have had caries in their permanent teeth.
• Data from state oral health surveys suggest that in most states, over 50% of third graders have experienced dental caries, ranging from 40% (Connecticut) to 75% (Arizona).4
• Approximately 23% of children have untreated primary tooth decay and 11% have untreated caries in the permanent dentition.
• The prevalence of dental caries in primary teeth increased significantly from 24% to 28% for 2- to 5-year-olds from the time periods of 1988-1994 to 1999-2004.
• By age 17 years, nearly 78% of children have experienced tooth decay, and by age 19 years, approximately 10% have lost at least one permanent tooth to caries.
• The progressive and cumulative effects of caries continue into adulthood, with more than 95% of adults experiencing caries and with 25% of seniors being edentulous.
Though dental caries is common, the distribution of caries is unequal, with certain subgroups of the population experiencing a disproportionately greater burden of dental disease. According to the National Institute for Dental and Craniofacial Research, 20% of the population bears at least 60% of the caries.5 Dental caries is more prevalent among children living in poverty,* with poor children experiencing five times more untreated dental caries than children in higher income families.6 Minority populations are also vulnerable, as children of Mexican-American and non-Hispanic black ethnicities are more likely to experience severe and untreated caries.7 Moreover, the pattern of caries involving specific tooth surfaces has changed. In the early 1970s, smooth surface lesions accounted for almost 25% of the decayed, missing, filled surfaces (dmfs) index. Recent data indicate that approximately 90% of caries in permanent teeth of children occur in pits and fissures, and approximately two thirds of caries are on the occlusal surface alone.8 Like permanent teeth, the pits and fissures of primary teeth are also at risk because roughly 44% of carious lesions in the primary teeth affect the occlusal surfaces of molars.8
The occlusal surface is prone to caries for several reasons. First, newly erupted, immature tooth enamel has a relatively high organic content and is more permeable, which makes it more susceptible to caries attack. Second, the pit and fissure morphology provides an environment for plaque retention and bacteria proliferation. The enamel is thinner in pits and fissures and may experience accelerated demineralization. Additionally, the molars take a relatively long time to fully erupt (1.5 to 2.5 years compared with just several months for premolars).9 This prolonged eruption time may interfere with adequate oral hygiene because toothbrush bristles have difficulty reaching the occlusal surface when it is out of the plane of occlusion, and the operculum covering the distal portion of the tooth may increase plaque retention.10 In addition, fluoride is less effective in preventing caries on the occlusal surfaces versus smooth surfaces. Data from fluoridated communities show significantly higher reductions in interproximal lesions compared with pit and fissure lesions.2 Hence, targeting preventive efforts at the occlusal surfaces of molars is appropriate for attempting to decrease the caries experience for U.S. children.
Sealant Effectiveness
Unquestionably, dental sealants prevent pit and fissure caries in both primary and permanent teeth. The long-term benefit of caries reduction from using sealants on permanent teeth has been well documented as multiple studies have shown clear evidence of a reduction in caries.11–30 Recently, in an effort to meet the need for evidence-based clinical recommendations, the American Dental Association Council on Scientific Affairs convened an expert panel to address the use of pit and fissure sealants.
Beauchamp and colleagues31 provides a summary of the evidence of sealant efficacy in caries reduction:
1. Reduction of caries incidence in children and adolescents after one-time placement of resin-based sealants ranges from 86% at 1 year to 78% at 2 years to 58% at 4 years.
2. When reapplied as needed, sealants are effective in reducing occlusal caries incidence in permanent first molars of children with reductions of 76% at 4 years.
3. Sealants are retained well on primary molars at a rate of 74% to 96% at 1 year and 70% to 76% at almost 3 years.
4. Compared with teeth without sealants, teeth that receive sealants are less likely to receive subsequent restorative treatment. If restorative treatment is required, the time until the first restorative treatment is greater than that for unsealed molars, and the restoration is likely to be less extensive.32
The effectiveness of sealants in preventing caries is so well recognized in the literature that a study design with a sealant-free control group is no longer considered ethically acceptable.33 Not only have multiple independent studies concluded that sealants are effective in preventing fissure caries, three review-analyses have confirmed the caries-preventive effect.34–36
Current Sealant Utilization
In 1974, when sealants were new technology, the initial ADA sealant utilization survey found that only 39% of dentists were placing sealants.37 Although adhesive dentistry was making great strides in acceptance for restorative procedures, using sealants for prevention was still low, and thus, by 1981 the ADA’s Council on Dental Materials, Instruments, and Equipment sponsored a major conference with the title, “Pit and Fissure Sealants: Why Their Limited Usage?” By the late 1980s and 1990s, regional and national surveys indicated large increases in sealant use among dentists.38,39 A recent survey reports that 79% of dentists use sealants in their practice “very often” or “often” in permanent teeth, whereas 53% “rarely” or “never” use sealants in primary teeth.40 Regional surveys indicate that most pediatric dentists (up to 96%) and most recent graduates (90% of dentists in practice for 10 years or less) use sealants.39,41,42 However, despite the reported increased incorporation of sealants into dentists’ practices, the number of children receiving sealants is unexpectedly low.
Data from the NHANES for the years 1999-2004 suggest that the prevalence of dental sealants on permanent teeth in children aged 6 to 11 years was 30%, and for adolescents and adults aged 12 to 29 years, it was 38%.1 Both of these figures are a significant increase from the 1988-1994 prevalence at 22% and 18%, respectively. However, in the low-income population, sealant use rates still remain low and have been found to be only 22%.43,44 Dennison and colleagues45 examined an insured population and also found a low sealant utilization rate. Even though sealant placement was a covered benefit, the researchers found a sealant use rate of 8.4% for first molars and 5.5% for second molars. With the knowledge that by age 17 years, nearly 78% of adolescents have experienced tooth decay and that 90% of these caries occurs in the pits and fissures, one might expect much higher rates of sealant use.
In 2000, the Healthy People 2010 Objectives for Improving Health was issued as a set of disease prevention and health promotion goals for the United States. Healthy People 2010 set a goal for the prevalence of sealants in children and adolescents to increase to 50%. However, oral health surveys of various states suggest that many were not able to meet this goal, with at least 30 states falling below the 50% goal.4
Low usage has been attributed to lack of confidence in the bonding of sealants to enamel, concern for sealing over caries, and to the difficulty of achieving isolation.46 Survey data indicate that dentists are apprehensive about sealing over incipient caries, because 80% of respondents indicate that they choose not to seal over incipient caries.47 Fear of placing a sealant over caries was one of the most frequently voiced concerns in the survey’s comments section. However, numerous studies have demonstrated that caries left underneath intact sealants remain arrested.48–51 Sealants significantly reduce the bacteria levels in cavitated lesions because retained sealant deprives bacteria of access to nutrients; bacteria that persist under sealants cannot produce acid when isolated from carbohydrate substrate, and thus progression of the lesion is unlikely.52 Oong and associates52 found that sealing over noncavitated lesions reduced the probability of lesion progression by more than 70%.
Another significant reason cited for limiting sealant usage is the lack of reimbursement for sealant placement. Many surveys reveal that lack of insurance reimbursement for both initial placement and reapplication is a frequently reported reason for limiting sealant usage.39,40,47 Concerning the lack of reimbursement, insurance companies provide the following reasons53,54: (1) concerns about cost-effectiveness of sealants, (2) sealant exclusions in the original or current contract, (3) undefined guidelines for sealant placement, and (4) potential for inappropriate usage and fees. However, these reasons are not well-founded. Of the insurance companies that do provide sealant coverage, approximately two thirds define certain clinical conditions for reimbursement, such as age limitations and restriction of sealant placement to permanent teeth, with some specifying molars only.39 Medicaid programs have made significant strides in making sealants a covered benefit. In 1991 only 58% of Medicaid programs provided reimbursement, but by 1994 all 50 states included sealants in their Medicaid programs.42,55 Hopefully, all third-party payers will recognize the benefits of sealants and add them as a covered benefit.
How Sealants Work
Three types of materials are used as sealants: resin, glass ionomer, and polyacid-modified resins. The most commonly accepted material is the resin-based sealant because it has shown superior retention rates compared with glass ionomer sealants.56–59 The resin-based sealant utilizes the principles of adhesive dentistry because given that it is retained by micromechanical retention. For the adhesion of the sealant to the enamel to be successful, the tooth must be clean and remain dry because the resin is hydrophobic. The tooth enamel is etched with 35% to 37% phosphoric acid, which creates surface irregularities that the sealant material flows into and forms resin tags (Figure 32-1). The resin is polymerized (usually by visible light, but there are also autopolymerizing resins) and forms a thin, plastic coating over the pits and fissures of the occlusal surface. This physical barrier is the essential component in preventing the carious process (Figure 32-2).
Types of Sealants
Sealant products come in a variety of materials, colors, and viscosities. Resin-based sealants are available as unfilled, filled, clear, colored, visible light–polymerized, autopolymerizing (chemically cured), and fluoride-releasing materials. The earliest sealants were autopolymerizing, but these have largely been replaced by visible light–curing sealants. The benefits of light-cured versus chemical-cured sealants are the following2: (1) the sealant material sets in 10 to 20 seconds versus 1 to 2 minutes; (2) no mixing of resins is required, eliminating the incorporation of air bubbles; (3) the viscosity of the sealant remains constant during infiltration of etched enamel pores; and (4) the sealant material does not set until it is light activated. However, studies have shown similar retention rates and similar strengths.33,60–62
Color
Sealants are often available as clear or opaque white. The advantages to an opaque sealant are that it is easy to see during application and easy to monitor its retention at a recall visit. Assessment of a clear sealant requires tactile exploration of the sealed surface. One study that examined the visibility of clear and opaque sealants found that the error rate for identifying an opaque sealant was less than 2%, whereas for clear resin it was nearly 23%. Moreover, the most common error for the examiners was to incorrectly identify a clear resin sealant on a tooth that had not been treated.63 No apparent difference in the clinical efficacy of either type of sealant has been reported. However, as will be discussed later, sealant retention is critical for the caries-preventive effect; hence, being able to quickly and correctly assess sealant retention is clinically important.
Two newer materials are available that have color properties. Clinpro (3M ESPE, St. Paul, Minn.) is a sealant that is pink upon application and turns white when cured. This color change provides no clinical advantage and has been described as a “perceived marketing benefit.”64 However, the sealant may be chosen for its other properties. Another material that provides a color change is Helioseal Clear Chroma (Ivoclar Vivadent, Amherst, N.Y.). This material is a clear sealant containing a photochromic dye that is normally light yellow. However, the dye can change from clear/yellow to green when exposed to the correct wavelengths of blue light. This color change is clinically relevant because it may assist a provider in assessing the sealant’s retention upon recall examination; however, using a polymerizing lamp to view the color change is an added step compared with assessing an opaque sealant. The color changing sealants have similar properties to and are as caries-protective as other resin-based sealants.65–68
Filler Content
Sealants also are available with various filler content. For the most part the filler content dictates the sealant’s physical characteristics in regard to viscosity, flowability, and resistance to wear. The theory is that unfilled sealants will penetrate deeper into the fissures because of their low viscosity, create longer resin tags, and therefore be better retained. Although data from one study suggest that unfilled sealants are retained better,69 other studies have found similar retention rates with unfilled and filled sealants.70,71 Unfilled sealants have lower rates of microleakage68,72,73 and better penetration into the fissures.74,75 Another clear advantage of the unfilled sealant is that occlusal adjustment is not necessary. Because of the lack of filler, the unfilled sealant will abrade rapidly if left in occlusion. On the other hand, filled sealants require occlusal adjustment because individuals are not able to abrade occlusal interferences caused by filled sealants to a comfortable level.76 Simonsen suggests that the necessity to adjust the occlusion increases the time and cost of the procedure, and it may also prevent delegation of sealant placement to auxiliaries.64,77 However, despite this clinical disadvantage, several studies have examined the use of flowable composite as sealant.
Early studies examining flowable composite showed inferior retention and microleakage compared with unfilled sealants.72,78 However, other studies have found that utilizing a bonding agent before placing the flowable material improves fissure penetration and decreases microleakage.79,80 Two studies evaluating the clinical retention of flowable composite used as a sealant with bonding agent have concluded that flowable composite is equal to65 and possibly superior to conventional sealant materials.81 However, given the added expense of the need for a bonding agent and the need for occlusal adjustment, the conventional unfilled resin-based sealant appears to be the most appropriate preventive therapy.
Fluoride-Releasing Sealants
Based on the knowledge of the benefits of fluoride release from glass ionomer materials, dental manufacturers have also developed fluoride-releasing resin sealants. However, studies have shown that salivary fluoride levels are the same before and after sealant placement, and there is no long-lasting release of fluoride to plaque and saliva.82,83 Additionally, clinical studies have not demonstrated significant caries prevention of fluoride-releasing sealants over those benefits obtained from conventional sealants.84 The addition of fluoride to resin sealants seems to be more of a marketing benefit by manufacturers because a clinical benefit appears doubtful.64 Several studies have shown similar retention rates of fluoride-releasing sealants to those of conventional sealants.84,85 However, in a systematic review of 31 studies (9 of which corresponded to fluoride-releasing sealants), Muller-Bolla and colleagues61 found that fluoride-containing sealants have lower retention rates at 48 months or more. Furthermore, they conclude that it is erroneous to consider fluoride-containing sealants as a fluoride reservoir with long-term release of fluoride into the immediate environment.
Glass Ionomer
Glass ionomer cement sealants were introduced as an alternative to resin-based sealants because of their fluoride-releasing and recharging ability, higher moisture toleration, and easy application. It is generally accepted that the effectiveness of sealants depends on long-term retention,34 and in clinical studies, retention is considered the principal evaluation criterion because it is used as a surrogate measure of effectiveness in preventing caries.61 When compared with resin-based sealants, glass ionomer sealants have shown poor retention rates.24,34,58,86 The evidence-based recommendations endorse the use of resin-based sealants because there is limited and conflicting evidence that glass ionomer cement reduces caries incidence in permanent teeth of children.31 However, the most recent systematic review with meta-analysis found no evidence that either material was superior to the other in the prevention of dental caries.87 This review summarizes studies that show that while glass ionomer sealants are not retained as well, the caries-preventive effect is similar to resin-based sealants. Two other reviews have reached similar conclusions.12,88 The theory for the protective benefit is that glass ionomer material remains in the deepest parts of the fissures even though it is not clinically evident.89 Seppa and Forss90 suggested that fissures sealed with glass ionomer are more resistant to demineralization, even after the sealant visibly appears to have debonded. This may be a result of the combined effect of the fluoride release, which increases the microhardness of the enamel, and of the residual material in the bottom of the fissure.
Glass ionomer sealants are widely used in countries with limited access to dentistry as part of the atraumatic restorative treatment (ART) technique. (See Chapter 21 for a discussion of ART.) A recent meta-analysis concluded that the survival rate of ART sealants after 3 years was 72%, whereas the caries-preventive effect was 97%.91 Furthermore, this review indicated that high-viscosity glass ionomers are the correct glass ionomer for ART sealants, because high-viscosity sealants placed with “finger pressure” penetrate as well as resin sealants, and high-viscosity materials are better retained than those of low to medium viscosity.
Nevertheless, current recommendations from the American Dental Association Council on Scientific Affairs, recommend resin-based sealants as the first choice for dental sealants. They also suggest that glass ionomer sealants may be used as an interim preventive agent when there are indications to place a sealant but moisture control may compromise sealant placement.31
Polyacid-Modified Resin Composites (Compomers)
Polyacid-modified resin composites were introduced in the 1990s as a new class of materials designed to combine the aesthetic property of composite with the fluoride-releasing property and adhesion of glass ionomer. These materials have been nicknamed compomers. They are similar to composites in that they contain no water and are hydrophobic, set by a polymerization reaction, lack the ability to bond to tooth structure, and require bonding agents of the type used with conventional composite resins.92 Like glass ionomers, they do release fluoride; however, their fluoride release levels are significantly lower than those of glass inomer cements.92
As a sealant material, polyacid-modified resin composites underperform glass ionomer cements in terms of fluoride release and underperform conventional resin composite materials in terms of retention. Polyacid-modified resin composites show low retention rates of 5% after 48 months and 3.4% after 6 years.93,94 Mechanical preparation of the tooth increases the retention rate of these materials; however, the marginal integrity is poor, and there is considerable occlusal wear.95,96 In a review of the effects of the advances in adhesive materials on sealant protocol, Boksman97 concludes that “current research cannot support the use of polyacid-modified resin composites for use as pit and fissure sealants.”
Who Really Needs Sealants?
Caries Risk Assessment
Caries management emphasizes the need for caries risk assessment, which is the likelihood of the incidence of caries during a certain time period. It is important to analyze the risk of caries for an individual during the decision-making process for sealants. Placing fissure sealants should not be considered routine for all children, because teeth with a low risk of developing caries receive little benefit from sealant placement,20,98 and it is not cost-effective.99,100 Patients should be evaluated for overall caries risk, but individual teeth should be evaluated as well. Heller and colleagues98 studied caries progression in sound teeth with and without sealants and in teeth with incipient carious lesions (defined by dark staining of the grooves, chalky appearance, or a slight explorer catch) (Figure 32-3) with and without sealants. These researchers found that the preventive benefit for sealing sound teeth was only 4.5%, whereas sealing over incipient caries lowered the caries incidence by 41%, almost a tenfold difference. Therefore sealants are indicated when the dentist determines that the tooth or the patient is at risk of experiencing caries.31
Age at Placement
Previous studies from the 1950s and 1960s showed a peak in caries incidence occurring shortly after tooth eruption and then tapering. The theory was that the occlusal surface was most vulnerable to caries within the first few years after eruption and that the risk of developing caries after this time period dropped dramatically. However, longitudinal data from the post-fluoridation era show new carious lesions develop yearly.101,102 In 1988 Ripa and associates101 analyzed data from nearly 2000 children aged 10 to 13 years who were examined annually for 3 years to determine caries activity. The authors found that the occlusal surfaces of molars suffered relatively constant attack between ages 10 and 16 years, at a rate of 10.4% per year.101 New information indicates that fluorides may have caused a delay in pit and fissure caries resulting in occlusal surfaces that decay at a later age.103 Hence, the nature of primary caries is changing from a rapidly progressing disease of childhood to a slowly progressing disease that commences in childhood but progresses steadily in adulthood.103 In accordance, the evidence-based recommendations endorse that adults as well as children should receive sealants when the tooth or the patient is at risk of experiencing caries.31 The question of whether to place a sealant over a fissured surface should not be based on how long ago the tooth erupted but on the clinical impression of whether a sealant is necessary to prevent caries.2 Figure 32-4 is a decision-making tree for sealant placement and can be used to help dentists decide when to apply sealants.
Which Teeth Should Be Sealed?
Traditionally, noncarious first and second permanent molars with deep fissures were the candidates for sealants; however, recommendations have been extended to any tooth at risk of developing caries, including primary teeth, permanent molars with incipient, noncavitated lesions, and/or premolars.31 At-risk primary teeth benefit from sealant placement because resin-based sealants are retained well on primary molars, with retention rates in the 70% to 95% range at approximately 3 years.104,105 Glass ionomer cements are not retained well and are not recommended for use as sealant material on primary teeth.106 Given the preventive benefit to the primary molar, when the child is able to cooperate for sealant placement, sealants should be used.31
The indications for sealant placement include2: (1) deep, retentive pits and fissures, which may cause wedging or catching of an explorer (Figure 32-5); (2) stained pits and fissures with minimal appearance of decalcification or opacification (i.e., incipient caries with no cavitation) (see Figure 32-3); (3) no radiographic or clinical evidence of interproximal caries in need of restoration on teeth to be sealed; (4) use of other preventive treatment, such as fluoride therapy, to inhibit interproximal caries formation; and (5) the possibility of adequate isolation from salivary contamination. Therefore, if placing a sealant is clinically indicated on any tooth with pits and fissures, a sealant should be used to prevent caries development.
Contraindications for sealant placement include2: (1) well-coalesced, self-cleaning pits and fissures; (2) radiographic or clinical evidence of interproximal caries in need of restoration; (3) presence of many interproximal lesions or restorations with no preventive plan/treatment to inhibit caries formation; (4) life expectancy of the primary tooth is limited; and (5) no possibility of adequate isolation from salivary contamination due to either eruption status or patient behavior.
Diagnosing Occlusal Caries
Diagnosing occlusal caries can be difficult, and research has shown that dentists correctly diagnose occlusal caries in only 42% of cases.107 In 2005 Stookey108 challenged the long-held belief that probing an occlusal groove with an explorer was necessary to diagnose a carious lesion. He summarized the evidence, which suggests that the use of an explorer does not increase dentists’ ability to make a correct diagnosis, and forceful use of an explorer can actually damage the tooth. Dentists are just as likely to make a correct diagnosis of a dry tooth in terms of the presence or absence of caries using only visual inspection as they are when they use an explorer.107 Proponents of eliminating the use of an explorer raise the concern that not only is tactile examination unreliable, but that forceful explorer usage can cause enamel defects, resulting in possible caries development or progression by causing cavitation of a previously noncavitated lesion.109 In one study, dentists were asked to gently probe a sample of third molars, half of which had initial carious lesions and half of which had sound occlusal surfaces.109 The teeth were then extracted and the fissures were examined with a scanning electron microscope, and enamel defects were noted for all of the teeth with initial caries and for two of the sound surfaces. The authors conclude that probing the occlusal surface with an explorer should be replaced by meticulous visual inspection. Opponents of the explorer do not endorse eliminating its use altogether. They recommend that the explorer be used differently, mainly to eliminate plaque in the fissures and to determine surface roughness of incipient lesions108: “The tip of the explorer should be moved gently across the surface of any noncavitated area to determine the presence or absence of surface roughness as an indication of whether the underlying demineralized area reflects an active lesion.”
Advocates of the explorer point to its historical use and emphasize that it is a time-tested tool for caries detection.110 Tactile diagnosis is taught universally in dental schools, and there are specific criteria for the detection and diagnosis of pit and fissure lesions.
Caries is present when the explorer catches or resists removal after the insertion into a pit or fissure with moderate to firm pressure, and when this is accompanied by one or more of the following111:
Though there are proponents on both sides of the argument, the evidence-based recommendations published in 2008 state that “the use of explorers is not necessary for the detection of early lesions,” because the use of an explorer does not improve the validity of the diagnosis of fissure caries compared with that of visual inspection alone.31,107 Visual examination alone (of a clean, dry tooth) is sufficient to detect early lesions. Moreover, forceful use of an explorer in demineralized fissures can, in essence, cause cavitation by creating an entrance through which cariogenic microorganisms can penetrate into the softened substructure.112
Given the challenge of occlusal caries diagnosis, adjuncts can be helpful. Several new technologies have shown promise in recent literature: light-induced and infrared laser fluorescence devices (Figure 32-6, A), a device which measures changes in heat and luminescence (see Figure 32-6, B), the electronic caries detector, quantitative laser fluorescence, and transillumination.2 However, to date, no technology can substitute for a thorough visual exam and clinical judgment based on experience.
Sealing Over Incipient Caries
If sealants are applied properly and are monitored periodically, caries arrest beneath a sealant. First, sealant application significantly decreases the viable bacteria in pits and fissures. Acid etching alone eliminates 75% of the viable microorganisms.113 In a recent review of six studies that addressed the reduction in viable bacteria after sealant placement, the authors found that sealing caries was associated with a 100-fold reduction in mean total viable bacteria counts.52 Secondly, studies show that sealant placement greatly reduces the number of carious lesions that progress. In a recent meta-analysis that examined the effectiveness of sealants in preventing progression of carious lesions, Griffin and colleagues48 found that the mean annual percentage of noncavitated lesions that had been sealed and still progressed was only 2.6% versus 12.6% of unsealed early, noncavitated lesions. The authors assert that “these findings not only support the placement of sealants to manage and arrest lesions determined to be in the early carious stages, but also, just as importantly, support their placement for surfaces where caries is uncertain.” Mertz-Fairhurst and coworkers50 published a classic study in 1998 in which they examined the cariostatic effect of sealed restorations after 10 years. One of the treatment groups included teeth with frank, cavitated lesions in which the only preparation provided was placing a 1-mm wide bevel in sound enamel around the margin of the lesion. The carious tooth structure was not removed. The teeth were restored with the following technique: etch, prime, bond, place composite, and then place sealant over the restoration. Of the 85 teeth available for follow-up at 10 years, only 12 of these teeth had failed. Although this article does not advocate sealing over frank, dentinal caries, it does highlight the power of the coronal seal. Whenever a situation occurs in which the practitioner is certain that a restoration is not yet warranted but is unsure of whether the fissure is simply stained or is exhibiting signs of incipient caries, the practitioner should err on the side of placing a sealant rather than monitoring the lesion.
Practitioners who are concerned about sealing over caries will often decide to take an invasive approach by prepping the tooth “just in case.” Some will erroneously call this a preventive resin restoration (PRR) when, in fact, it is most likely a fissurotomy or enamelplasty procedure. The PRR is more appropriately termed the conservative adhesive resin restoration. (See Chapter 21 for a discussion of conservative adhesive restorations.) It is considered an ultraconservative preparation because only the small areas of caries are removed; intact pits and fissures are not opened with a bur. A restorative material (composite, glass ionomer, ama/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


 Outline
Outline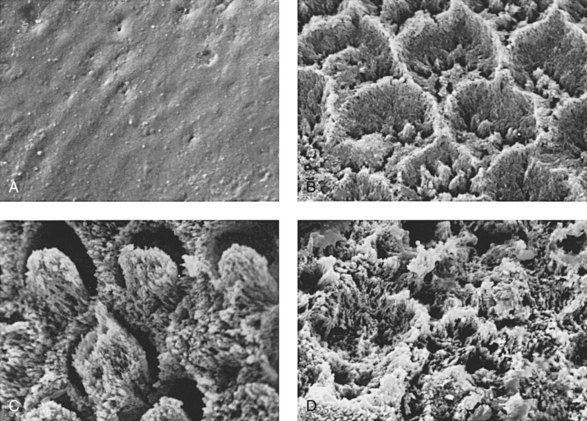
 FIGURE 32-1
FIGURE 32-1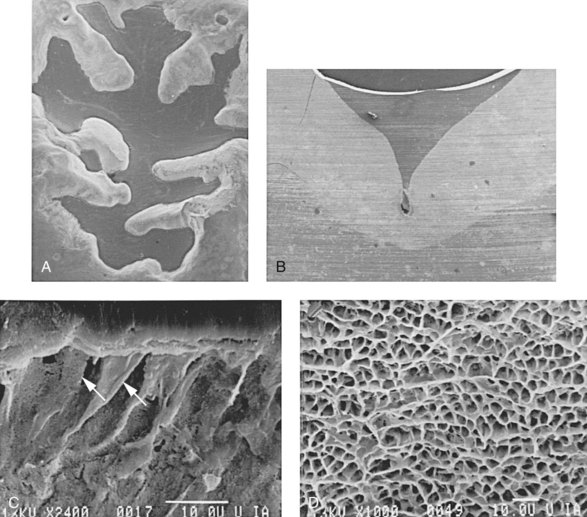
 FIGURE 32-2
FIGURE 32-2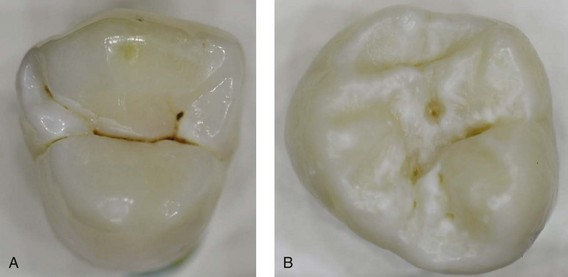
 FIGURE 32-3
FIGURE 32-3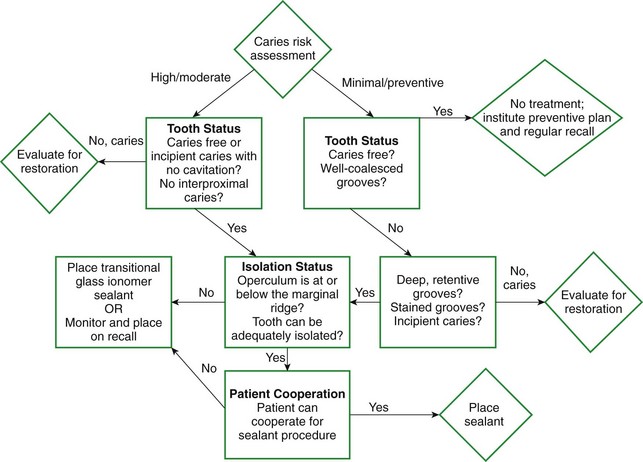
 FIGURE 32-4
FIGURE 32-4
 FIGURE 32-5
FIGURE 32-5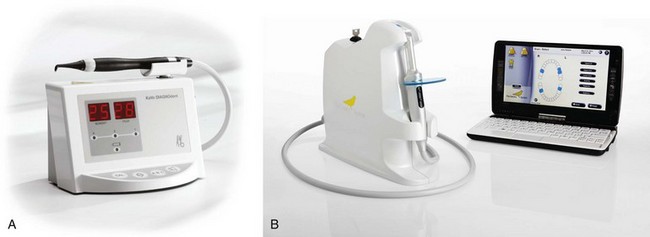
 FIGURE 32-6
FIGURE 32-6