Radiographic Aids in the Diagnosis of Periodontal Disease
Radiographs are valuable for diagnosis of periodontal disease, estimation of severity, determination of prognosis, and evaluation of treatment outcome.1–3 However, radiographs are an adjunct to the clinical examination, not a substitute for it.
Normal Interdental Bone
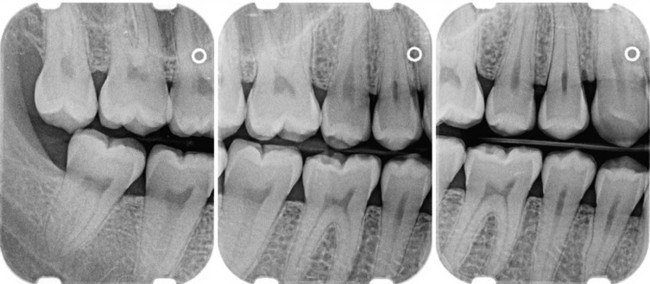
Evaluation of bone changes in periodontal disease is based mainly on the appearance of the interdental bone because the relatively dense root structure obscures the facial and lingual bony plates. The interdental bone normally is outlined by a thin, radiopaque line adjacent to the periodontal ligament (PDL) and at the alveolar crest, referred to as the lamina dura (Figure 31-1). Because the lamina dura represents the cortical bone lining the tooth socket, the shape and position of the root and changes in the angulation of the x-ray beam produce considerable variations in its appearance.

The width and shape of the interdental bone and the angle of the crest normally vary according to the convexity of the proximal tooth surfaces and the level of the cementoenamel junction (CEJ) of the approximating teeth. The faciolingual diameter of the bone is related to the width of the proximal root surface. The angulation of the crest of the interdental septum is generally parallel to a line between the CEJs of the approximating teeth (see Figure 31-1). When there is a difference in the level of the CEJs, the crest of the interdental bone appears angulated rather than horizontal.
Radiographic Techniques
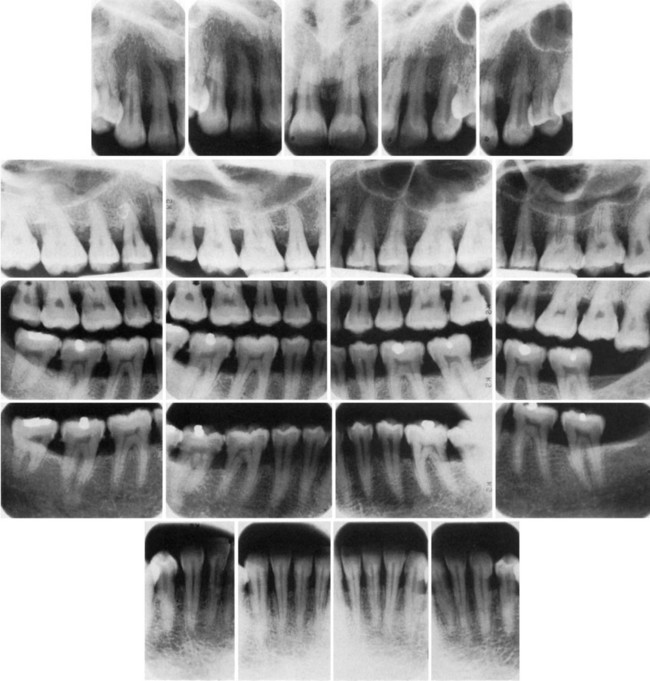
In conventional radiographs, periapical and bite-wing projections offer the most diagnostic information and are most commonly used in the evaluation of periodontal disease. To properly and accurately depict periodontal bone status, proper techniques of exposure and processing are required. The bone level, pattern of bone destruction, PDL space width, as well as the radiodensity, trabecular pattern, and marginal contour of the interdental bone, vary by modifying exposure and development time, type of film, and x-ray angulation.4 Standardized, reproducible techniques are required to obtain reliable radiographs for pretreatment and posttreatment comparisons.
Prichard5 established the following four criteria to determine adequate angulation of periapical radiographs:
1. The radiograph should show the tips of molar cusps with little or none of the occlusal surface showing.
2. Enamel caps and pulp chambers should be distinct.
3. Interproximal spaces should be open.
4. Proximal contacts should not overlap unless teeth are out of line anatomically.
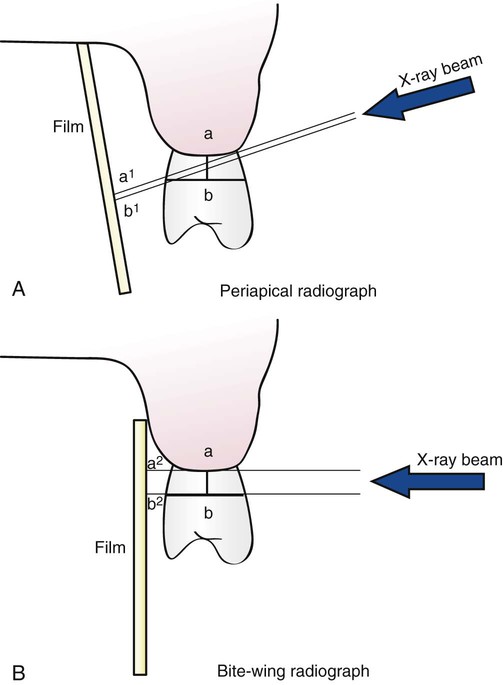
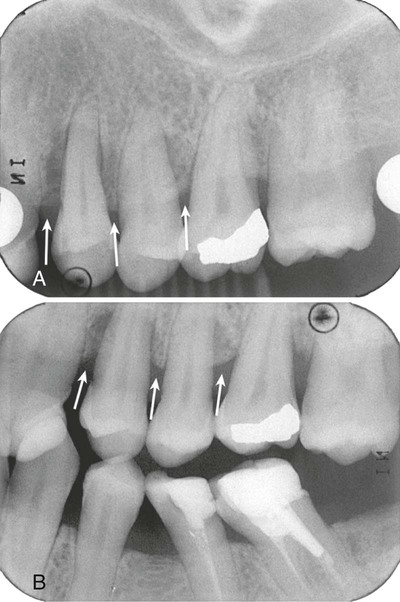
For periapical radiographs, the long-cone paralleling technique most accurately projects the alveolar bone level (Figure 31-2). The bisection-of-the-angle technique elongates the projected image, making the bone margin appear closer to the crown; the level of the facial bone is distorted more than that of the lingual. Inappropriate horizontal angulation results in tooth overlap, changes the shape of the interdental bone image, alters the radiographic width of the PDL space and the appearance of the lamina dura, and may distort the extent of furcation involvement (see Figure 31-2).
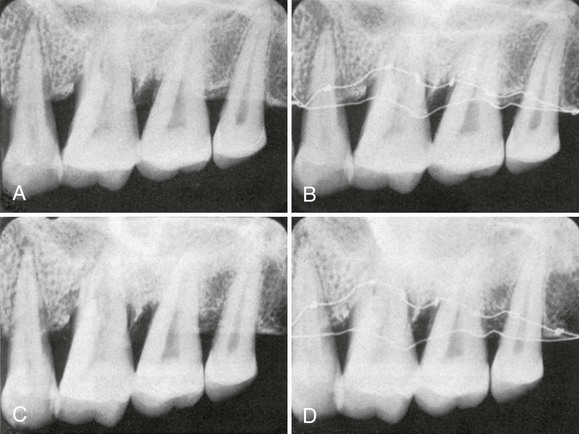
Periapical radiographs frequently do not reveal the correct relationship between the alveolar bone and the CEJ.6 This is particularly true in cases in which a shallow palate or floor of the mouth does not allow ideal placement of the periapical film. Bite-wing projections offer an alternative that better images periodontal bone levels. For bite-wing radiographs, the film is placed behind the crowns of the upper and lower teeth parallel to the long axis of the teeth. The x-ray beam is directed through the contact areas of the teeth and perpendicular to the film. Thus the projection geometry of the bite-wing films allows the evaluation of the relationship between the interproximal alveolar crest and the CEJ without distortion7 (Figures 31-3 and 31-4). If the periodontal bone loss is severe and the bone level cannot be visualized on regular bite-wing radiographs, films can be placed vertically to cover a larger area of the jaws (Figure 31-5). More than two vertical bite-wing films might be necessary to cover all the interproximal spaces of the area of interest.
Bone Destruction in Periodontal Disease
Early destructive changes of bone that do not remove sufficient mineralized tissue cannot be captured on radiographs. Therefore slight radiographic changes of the periodontal tissues suggest that the disease has progressed beyond its earliest stages.8 The earliest signs of periodontal disease must be detected clinically.
Pattern of Bone Destruction
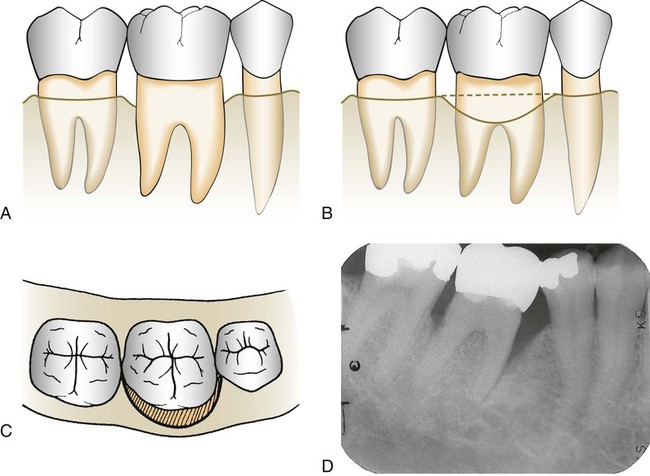
In periodontal disease the interdental bone undergoes changes that affect the lamina dura, crestal radiodensity, size and shape of the medullary spaces, and height and contour of the bone. Height of interdental bone may be reduced, with the crest perpendicular to the long axis of the adjacent teeth (horizontal bone loss; Figure 31-6), or angular or arcuate defects (angular, or vertical, bone loss; Figure 31-7) could form.
Radiographs do not indicate the internal morphology or depth of craterlike defects. Also, radiographs do not reveal the extent of involvement on the facial and lingual surfaces. Bone destruction of facial and lingual surfaces is masked by the dense root structure, and bone destruction on the mesial and distal root surfaces may be partially hidden by superimposed anatomy, such as a dense mylohyoid ridge (Figure 31-8). In most cases, it can be assumed that bone losses seen interdentally continue in either the facial or the lingual aspect, creating a troughlike lesion.
Interdental bone loss may continue facially and/or lingually to form a troughlike defect that could be difficult to appreciate radiographically. These lesions may terminate on the radicular surface or may communicate with the adjacent interdental area to form one continuous lesion (Figure 31-9).
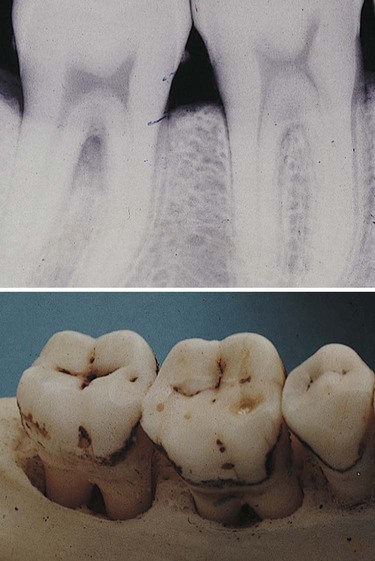
Figure 31-10 shows two adjacent interdental lesions connecting on the radicular surface to form one interconnecting osseous lesion. Along with clinical probing of these lesions, the use of a radiopaque pointer placed in these radicular defects will demonstrate the extent of the bone loss.
Periodontal bone loss should be differentiated from normal anatomy or anatomic variants that can resemble disease. For example, nutrient canals in the alveolar bone can appear as linear and circular radiolucent areas (Figure 31-11). These canals can be seen more frequently in the anterior mandible, although they can be present throughout the alveolar ridge.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses