Facial Neuropathology
James R. Hupp
The dentist is frequently called upon to determine the etiology of pain in the oral-maxillofacial region. Although oral pain is most frequently of odontogenic origin, many facial pains arise from other sources. The diversity of structures in the head and neck region (e.g., eyes, ears, salivary glands, muscle, joints, sinus membranes, intracranial blood vessels) can make arriving at an accurate diagnosis challenging. Even typical toothache symptoms may occur in a healthy tooth because of referred pain or a damaged pain transmission system.
Basics of Pain Neurophysiology
Pain is a complex human psychophysiologic experience. This unpleasant experience is influenced by such factors as past pain experiences, cultural behaviors, and emotional and medical states. As the term implies, the pain experience has physiologic and psychological aspects. The physiologic aspects involve several processes: transduction, transmission, and modulation. The sum of these processes, when integrated with higher thought and emotional centers, yields the human experience of pain. Transduction refers to activation of specialized nerves, namely, A-delta (Aδ) and C-fibers, which transmit information to the spinal cord or, in the case of the trigeminal nerve, to the trigeminal nucleus.
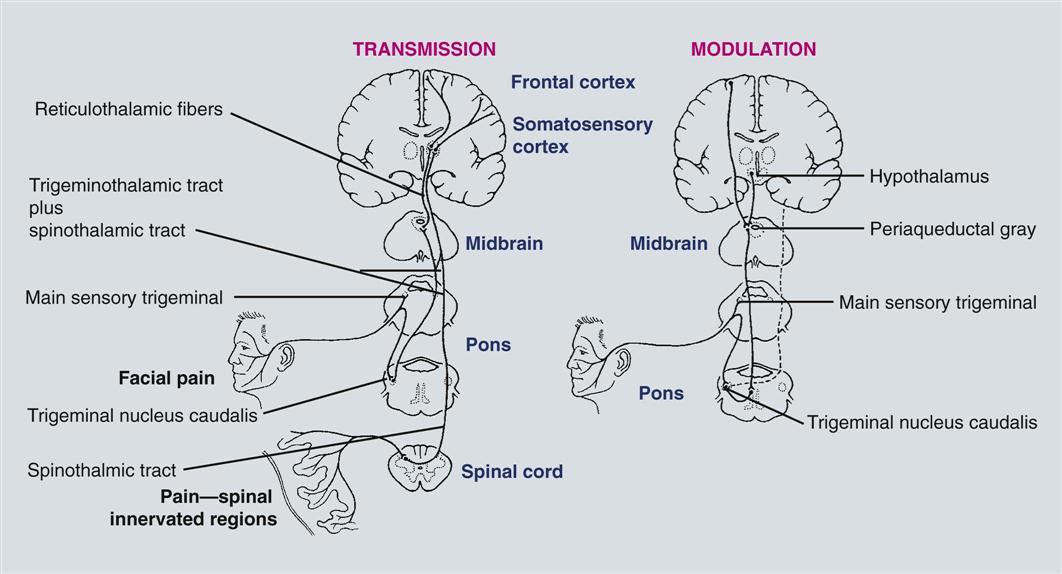
Table 30-1 lists peripheral nerve fibers and their individual characteristics. Chemical, thermal, and mechanical stimuli can activate the free nerve endings of nociceptors, the peripheral nerves indicated previously that transmit pain information. Once in the central nervous system (CNS), information regarding pain is transmitted to the thalamus and, hence, to cortical centers that process the sensory–discriminative and the emotional–affective aspects of the experience. Modulation systems are activated with pain transmission to varying degrees. The pain modulation system limits the rostral flow of pain information from the spinal cord and trigeminal nucleus to higher cortical centers. A schematic representation of these pain pathways is shown in Figure 30-1. The chemical and receptor milieu in which transmission and modulation activity occurs is complex. The primary neurochemicals for transmission pathways involve glutamate and substance P, although dozens of neurochemicals have been implicated in pain transmission. The brainstem and spinal cord are the predominant structures involved in modulation. The related primary chemicals include the endogenous opioids, along with serotonin and norepinephrine. Alterations in receptor function are now thought to be critical to the generation of many chronic painful states.
Table 30-1
Relationship between Sensory Nerve Fiber Size (Diameter) and Conduction Velocity
| Fiber Type | Diameter (micrometer) | Velocity (meters per second) |
| Aα | 13–22 | 70–120 |
| Aß | 8–13 | 40–70 |
| Aγ | 4–8 | 15–40 |
| Aδ | 1–4 | 5–15 |
| B | 1–3 | 3–14 |
| C | 0.5–1.0 | 0.5–2.0 |
Although the pain sensory system appears hardwired, the psychological influences on pain perception should not be underestimated. For the dentist, this influence is a daily part of clinical practice. All dentists are well aware of the extensive variability of the pain response that different patients display to similar procedures. For instance, for some patients, the sound of the dental drill evokes true pain perception despite the fact that the bur has not yet touched the tooth. Psychological influences are particularly important in determining perceived pain intensity and patient response to pain. When pain becomes chronic, generally defined as greater than 4 to 6 months in duration, attention to psychological influences can become particularly important when trying to manage the pain experience.
Classification of Orofacial Pains
Numerous classification systems exist for orofacial pain conditions. At the most basic level, it is appropriate to classify orofacial pains as primarily somatic, neuropathic, or psychological.
Somatic pain arises from musculoskeletal or visceral structures interpreted through an intact pain transmission and modulation system. Common orofacial examples of musculoskeletal pains are TMJ disorders or periodontal pain. Examples of visceral orofacial pains include salivary gland pain and pain caused by dental pulpitis, the tooth pulp behaving like a visceral structure. Neuropathic pain arises from damage or alteration to the pain pathways, most commonly a peripheral nerve injury due to surgery or trauma. Other causes may involve CNS injury as in thalamic stroke.
Orofacial pains of true psychological origin are so rare as not to be included in the differential diagnosis of orofacial pain for the general practitioner. Although psychological influences frequently modify the patient’s perception of pain intensity and the patient’s response to pain, an actual pain symptom generated by psychiatric disturbance (e.g., conversion disorder or psychotic delusion) is exceedingly rare. Malingering, a term used to identify behavior in which a patient consciously feigns illness or the extent of illness for personal gain, can and does occur, although the literature suggests that the incidence is low. However, a dental patient complaining of chronic pain should be presumed to have a real pain problem unless definitively proven otherwise.
The term atypical facial pain is still seen in the literature and is used as a diagnosis primarily by physicians and some dentists; therefore a medical diagnosis code (i.e., International Classification of Diseases, tenth revision, code G50.1) is associated with it. When reviewing the literature regarding atypical facial pain, a psychological cause is frequently implied. Because true psychogenic pain is rare, this term should be abandoned. For those undiagnosed facial pains, the appropriate term should be facial pain of unknown cause until a definitive diagnosis has been established. As a practical matter, these patients, unfortunately, continue to be labeled with the diagnosis of atypical facial pain for coding purposes, but the dentist should be aware that this is a “diagnosis” awaiting further clarification.
This chapter covers neuropathic facial pains and common headache disorders. TMJ disorders are discussed in Chapter 31. A glossary of pain terminology is provided in Box 30-1.
Neuropathic Facial Pains
Neuropathic pains arise from an injured pain transmission or modulation system. Surgical intervention or trauma is frequently the cause. For example, trauma to the infraorbital region may lead to numbness or pain in the distribution of the infraorbital nerve. In dental surgery, extraction of impacted mandibular third molars carries a measurable risk of nerve damage to the mandibular and lingual nerves. In the majority of these cases, damage leads to paresthesia, an abnormal sensation in the dermatome of the affected nerve. Typically, this sensation is one of mild numbness or tingling. Loss of all sensation may occur when the nerve is transected. In a subset of cases, dysesthesia—an abnormal, unpleasant sensation—can result; it is often described as a burning or sharp electric shocklike sensation. When a patient complains of burning or sharp shocklike pain in the face or mouth, pain of neuropathic origin should be included in the differential diagnosis. One should appreciate that the oral cavity is the most common site of amputation, if one recognizes amputations to include the teeth and the dental pulp (i.e., endodontics). As in phantom limb pain after extremity amputation, “phantom” sensations can also arise, albeit rarely, after pulpal trauma or extraction. Neuropathic pains may also give rise to the sensation of tooth pain, which is often a diagnostic dilemma for dentists. Referral of patients for management of these disorders to dentists focusing on orofacial pain diagnosis and management or to the patient’s personal physician or a neurologist is customary.
Trigeminal neuralgia
The prototypic neuropathic facial pain is trigeminal neuralgia (TN) (Box 30-2), literally nerve pain arising from the trigeminal nerve. Although this could refer to any neuropathic pain of trigeminal nerve origin, TN or tic douloureux (i.e., painful tic) has specific inclusion criteria. Occurring most frequently in patients over 50 years of age (incidence 8 : 100,000; female-to-male ratio 1.6 : 1), TN usually occurs with sharp, electric shocklike pain in the face or mouth. The pain is intense, lasting for brief periods of seconds to 1 minute, followed by a refractory period during which the pain cannot be reinitiated. At times, a background aching or burning pain is present. Usually, a trigger zone is present where mechanical stimuli such as soft touch may provoke an attack. Firm pressure to the region is generally not as provocative. Common cutaneous trigger zones include the corner of the lips, cheek, ala of the nose, or lateral brow. Any intraoral site may also be a trigger zone for TN, including teeth, gingiva, or the tongue. Trigger zones in the V2 and V3 distributions are most common, after which they occur alone (and in decreasing order of incidence) in the V3, V2, and V1 distributions. The pain of TN illustrates an important distinction of many neuropathic pains as opposed to somatic pains—the lack of a typical graded response to increasing stimulation. If light touch stimulation produces a pain response out of proportion to the stimulus, a neuropathic process should be considered. This also holds true for pain that has a burning or electric shocklike quality. Sometimes a background aching pain accompanies TN, making it difficult to distinguish from the pain of acute pulpitis or, possibly, periapical periodontitis. Importantly, local anesthetic block of the trigger zone arrests the pain of TN for the duration of anesthesia and sometimes longer, which can lead the dentist to mistakenly ascribe a “dental” cause to the pain complaint.
The cause of TN is not entirely clear, but the consensus is that pressure on the root entry zone of the trigeminal nerve by a vascular loop leads to focal demyelination. This demyelination, in turn, precipitates ectopic or hyperactive discharge of the nerve. The site of demyelination determines the trigeminal division involved and, hence, the clinical presentation. Other diseases such as multiple sclerosis, tumors, and Lyme disease can produce pain similar to that produced by TN. The treatment of TN is medical or surgical. Medical treatment is generally undertaken with anticonvulsants.
The classic medication for the condition is carbamazepine, but newer anticonvulsants (e.g., gabapentin and oxcarbazepine) and the antispastic baclofen are commonly used as well. Table 30-2 lists commonly used TN and neuropathic facial pain medications. Many of these medications have significant, even life-threatening, side effects; therefore, only dentists focusing on orofacial pain diagnosis and management use them in dental practice. Surgical treatment includes microvascular decompression of the offending vascular loop (so-called Janetta procedure), GammaKnife radiosurgery, percutaneous needle thermal rhizotomy, or balloon compression of the root entry zone. For the dentist, the critical issue is recognizing TN so that unneeded dental treatment or extractions are avoided. Unfortunately, when the trigger zone is located in an intraoral, dental, or periodontal site, unnecessary dental treatment is common.
Table 30-2
Common Medications for Trigeminal Neuralgia and Neuropathic Facial Pains
| Medications | Dosage (mg/d) |
| Anticonvulsants | |
| Carbamazepine (Tegretol) | 400–1200 |
| Gabapentin (Neurontin) | 600–3200 |
| Clonazepam (Klonopin) | 2–8 |
| Divalproex (Depakote) | 500–2000 |
| Oxcarbazepine (Trileptal) | 300–2400 |
| Lamotrigine (Lamictal) | 50–500 |
| Topiramate (Topamax) | 50–400 |
| Phenytoin (Dilantin) | 300–600 |
| Tricyclic Antidepressants | |
| Amitriptyline | 10–300 |
| Doxepin | 10–300 |
| Nortriptyline | 10–150 |
| Imipramine | 10–300 |
| Antispastic | |
| Baclofen (Lioresal) | 15–80 |
Pretrigeminal neuralgia
Although a rare condition, pretrigeminal neuralgia (pre-TN) may occur. The presenting condition is typically an aching dental pain in a region where clinical and radiographic examinations reveal no abnormality. Local anesthetic block of the tooth (or extraction site, if applicable) arrests pain for the duration of anesthetic’s action. A number of patients with this condition have been demonstrated to go on to have typical TN symptoms (i.e., sharp electric shock pains the area). Pre-TN responds to similar treatments as TN, beginning with anticonvulsant therapy. To avoid unnecessary dental treatment, the dentist must have a high index of suspicion for secondary diagnoses for those pains that are inconsistent with physical examination or do not respond in a predictable way after treatment. Clinical features of pre-TN are listed in Box 30-3.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses