Implant Treatment
Advanced Concepts and Complex Cases
Myron R. Tucker, Edward M. Narcisi and Mark W. Ochs
The previous chapter focused primarily on the clinical evaluation and surgical as well as prosthetic considerations for basic implant treatment. The techniques described in Chapter 14 are focused primarily on clinical situations where adequate bone and soft tissue exist and implants can be placed into a well-healed area of bone without jeopardizing anatomic structures such as the maxillary sinus or the inferior alveolar nerve. There are situations where placement of implants becomes more complex. In some cases, it may be advantageous to place an implant at the time of extraction. In many cases, the bone and soft tissue present are inadequate for implant placement and require augmentation to facilitate implant placement. This chapter will focus on considerations for types of cases that require immediate implant placement, as well as cases where preparatory bone and soft tissue augmentation may be required before implant placement. These types of surgical procedures are performed by surgeons with advanced training and experience in bone grafting and implant procedures.
Immediate Postextraction Placement of Implants
When implant placement is planned before tooth extraction, consideration should be given to the most desirable time for implant placement. The implant may be placed immediately (i.e., at the time of extraction), early (i.e., 2 months after extraction), or late (i.e., more than 6 months after extraction). Each of these times has its indications, advantages, and disadvantages.
The primary advantage of immediate placement is that this allows the overall shortest healing time and combines tooth extraction with surgical implant placement. Placing a provisional restoration at the same procedure may provide the best opportunity for maintenance of soft tissue anatomy and the best immediate and long-term esthetic results. The primary disadvantage of immediate placement is related to the difference in the anatomy of the root or roots of the extracted tooth compared with the shape and size of the implant. This is particularly true of a multirooted tooth that is being replaced by an implant. Even in the case of an incisor, the difference in the shape of the root and that of the implant creates some difficulty in implant placement. Another disadvantage is that if the implant is exposed to excessive occlusal forces, the immediate and long-term stability of the implant can be jeopardized.
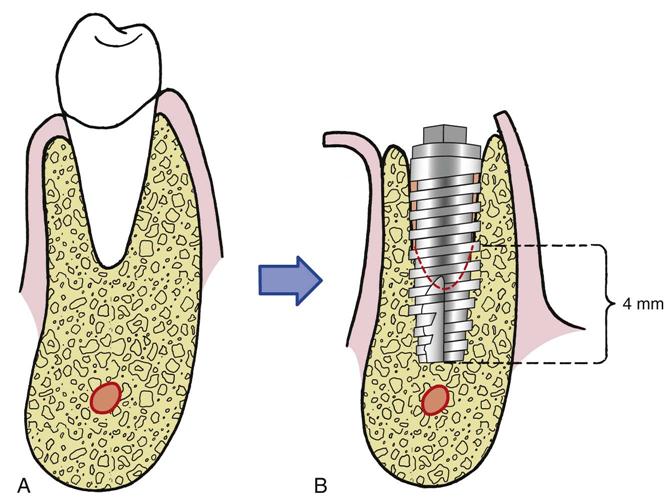
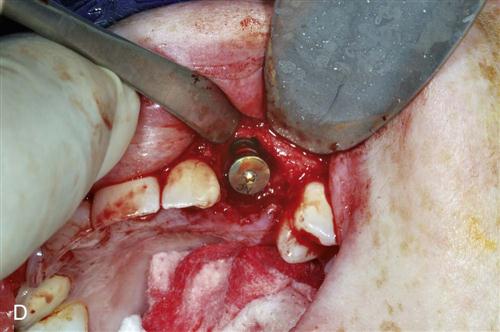
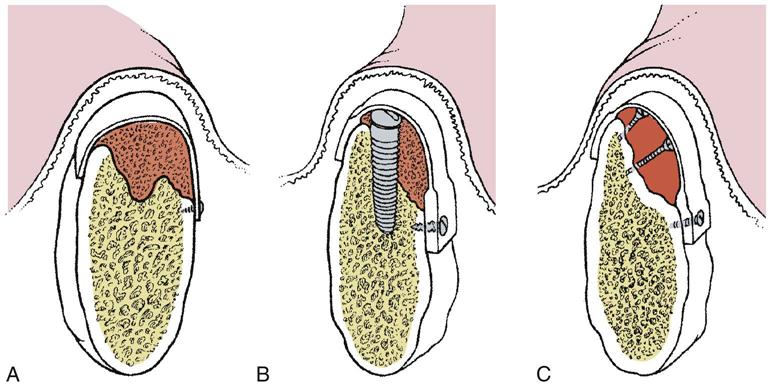
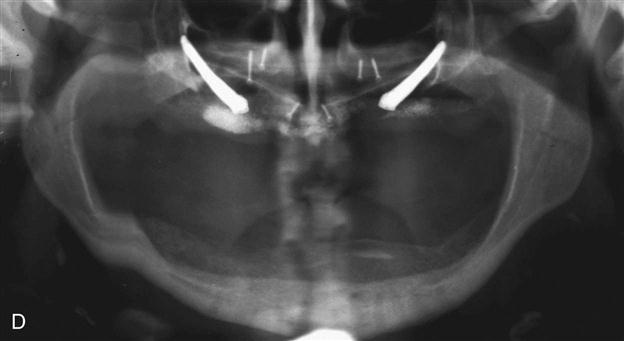
Immediate placement can be considered if the tooth to be removed is not infected and can be removed without the loss of alveolar bone. A critical component in the success of this technique is to complete the extraction of the tooth with minimal bone removal and without distorting or weakening the bony support. An atraumatic extraction technique utilizing periotomes will help minimize damage to bone and help facilitate implant placement. Initial implant stability at the time of placement is also critical to long-term success. When the implant is placed, at least 4 millimeters (mm) of the implant apex should be precisely seated in firm bone to provide this initial stability (Figure 15-1). Surgical guides are extremely helpful in placing the implant, since drilling the implant site at the correct angulation can sometimes be difficult, as the drills can be easily deflected when bouncing off the wall of the socket (Figure 15-2). The implant should be countersunk slightly below the height of crestal bone to allow for resorption of bone resulting from extraction. In the esthetic zone (maxillary anterior), the platform of the implant is ideally placed 3 mm below the free gingival margin. This allows for development of optimal emergence contour of the final restoration and soft tissue maintenance. In general, the implant is also positioned 1 mm palatal to the center of the extracted tooth root. This accounts for anticipated facial bone and soft tissue remodeling that decreases the facial crestal volume.
The gap between the implant and the residual tooth socket must be evaluated and managed according to its size. If the gap is less than 1 mm and the implant is stable, often no treatment modification is needed. If the gap is greater than 1 mm, grafting with a particulate bone material may be indicated. At present the need for this is controversial. In most cases, with flapless, atraumatic extraction techniques primary closure may not be possible or desirable. In this situation, a resorbable collagen pellet may be placed over the implant and held in place with a “figure-of-eight” suture. The surgeon may consider extending the time allowed for integration before loading.
In isolated cases, restoration at the time of implant placement may be considered. It is extremely important to ensure that the restoration is in ideal firm contact with adjacent teeth, which will help reduce unfavorable loading on the implant until it is osseointegrated.
Bone Grafting and Graft Substitutes
In many cases, areas to be restored with implants have insufficient bone for implant placement. This may be a result of extraction and bone atrophy, sinus pneumatization, previous trauma, congenital defects, or removal of pathologic lesions. In these cases, bone will need to be augmented to provide adequate support for implant placement. Several potential sources of graft material can be considered, depending on the volume and configuration of bone needed.
Autogenous Grafts
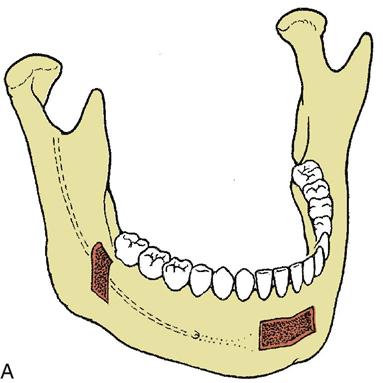
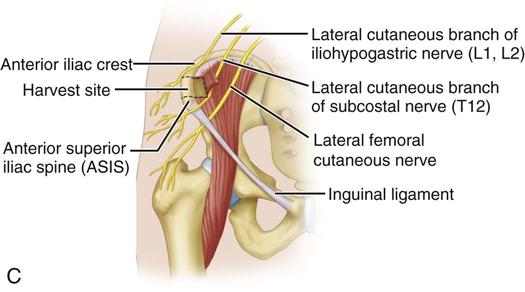
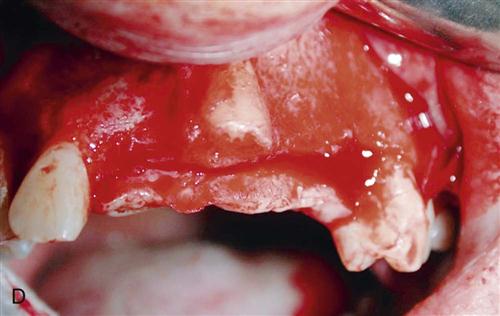
Autogenous bone can be harvested from several anatomic areas. Intraorally, bone can be harvested from the mandibular symphysis, ramus, or maxillary tuberosity areas. Bone in the tuberosity is primarily cancellous, whereas in the ramus–posterior body area of the mandible, the bone is primarily cortical. The symphysis provides the best intraoral source for a reasonable volume of cortical and cancellous bone (Figure 15-3). When more bone is required for situations such as atrophic edentulous mandible or bilateral sinus lifts, an extraoral site should be considered if autogenous bone is to be used. The most common site of graft harvest is the anterior iliac crest. Other areas where bone is sometimes harvested include the tibia, the fibula, and the calavarium.
Allografts
Allogeneic bone grafts procured from cadavers are processed to achieve sterility and decrease the potential for immune response. The sterilization process destroys the osteoinductive nature of the graft; however, the graft provides a scaffold, allowing bone ingrowth (osteoconduction). Bony incorporation, followed by remodeling and resorption, occurs during the healing phase. Granular forms of allogeneic graft material provide increased surface area and improved adaptation within the graft and are the most commonly used for augmenting alveolar ridge contour defects. The advantages of allogeneic bone grafting include the avoidance of an additional donor site, unlimited availability, and the fact that patients can undergo this type of procedure in an outpatient setting. The disadvantage is that a significant amount of grafted bone is resorbed, which results in a much smaller volume of bone for implant placement.
Xenografts
Xenografts are derived from the inorganic portion of bone harvested from a species that is genetically different from the graft recipient. The most common source of xenografts is bovine bone. The advantages and disadvantages are similar to those of allografts, including significant postgrafting resorption.
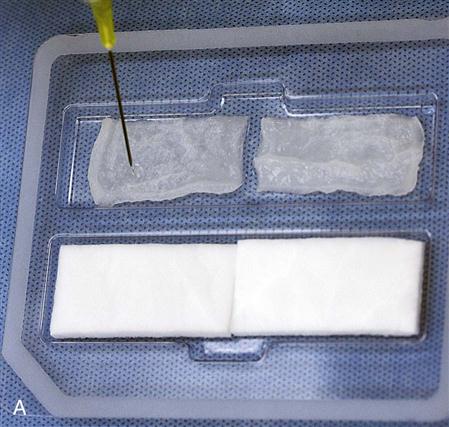
Bone Morphogenetic Proteins
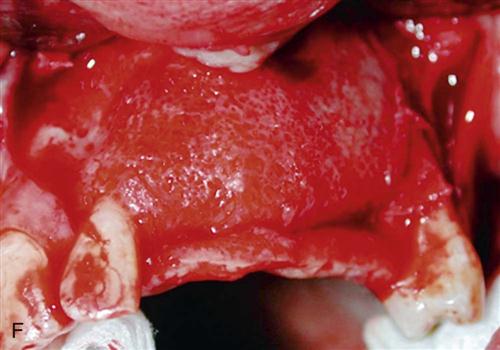
One of the most exciting recent advancements in bone grafting has been the extensive research related to bone morphogenetic proteins (BMPs). BMPs are a family of protein factors that have been isolated and applied to reconstruction of the maxillofacial skeleton. These proteins have the ability to enhance bone graft healing and, in many cases, substitute for other graft materials. Recombinant human BMP (rhBMP-2) has been isolated and has now been produced and packaged for use in grafting procedures. The BMP is placed on carriers, usually absorbable collagen sponges, to facilitate placement in the graft site. BMP can be positioned around implants within the extraction sites aiding in osseointegration. In larger defects, the BMP is usually combined with osteoconductive allogeneic materials to expand the graft volume and to help place, shape, and contain the graft material. BMP with a collagen sponge carrier can be used for sinus lifting and reconstruction of non–load-bearing bony defects (Figure 15-4). The obvious advantages include eliminating the need for donor site surgery and improved bone formation at the site of augmentation. The primary disadvantages include significant postoperative edema and the cost of the BMP.
Two problems associated with any type of grafting include containment and shaping of the graft material and prevention of fibrous tissue ingrowth during the healing phase. Placement of particulate grafts to augment alveolar ridges often requires some type of containment device or material to facilitate the ideal ridge size and shape. Materials used to contain and shape the graft can also be effective in eliminating the unfavorable invasion of soft tissue during healing.
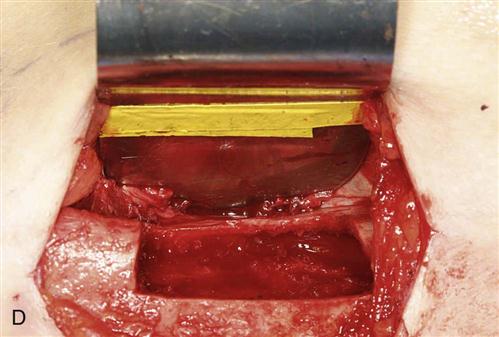
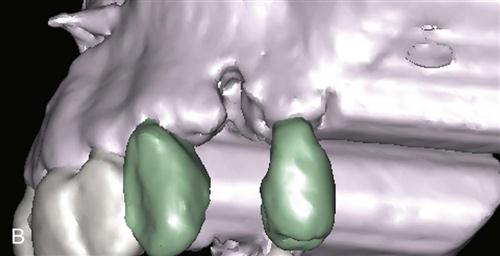
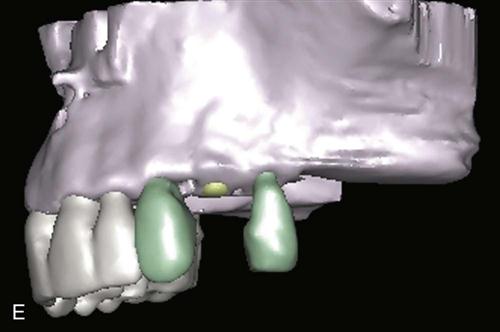
Guided bone regeneration is a process that allows bone growth while retarding the ingrowth of fibrous connective tissue and epithelium. Many bone defects will regenerate with new bone if the invasion of connective tissue from adjacent soft tissue can be prevented. Guided bone regeneration involves using a barrier that is placed over the bony defect to prevent fibrous tissue ingrowth while the bone underlying the barrier has time to grow and fill the defect (Figure 15-5). This technique is particularly useful in the treatment of buccal dehiscence, where labiobuccal (horizontal) augmentation of bone is required. Guided bone regeneration can be performed simultaneously with implant placement or before stage I. A variety of materials may serve as barriers to fibrous tissue ingrowth. Expanded polytetrafluoroethylene (Gore-Tex; W.L. Gore & Associates, Inc., Flagstaff, AZ) is the most extensively tested material. Resorbable materials are also now available, eliminating the necessity of removal. Thin, malleable titanium mesh is also a commonly used material facilitating maintenance of graft shape while eliminating extensive fibrous ingrowth. Titanium mesh trays can be created by trimming and contouring flat titanium mesh at the time of surgery, or they can be fabricated prior to surgery using diagnostic mounted dental casts or CAD-CAM (computer-aided design and computer-aided manufacturing) technology.
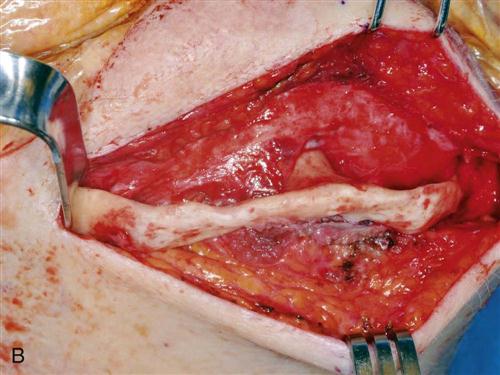
Mandibular Augmentation
Augmentation grafting adds strength to an extremely deficient mandible and improves the height and contour of available bone for implant placement in denture-bearing areas. Superior border augmentation with a bone graft is often indicated when severe resorption of the mandible results in inadequate height and contour and potential risk of fracture or when the treatment plan calls for placement of implants in areas of insufficient bone height or width. Neurosensory disturbances from inferior alveolar nerve dehiscence at the superior aspect of the mandible also can be improved with superior border grafting. Sources of graft material include autogenous bone, allogeneic bone, or both, often combined with BMP (off-label use). Historically, autogenous bone has been the most biologically acceptable material used in mandibular augmentation. Disadvantages of the use of autogenous bone include the need for donor site surgery and the possibility of the significant resorption that occurs after grafting. The use of allogeneic bone eliminates the need for a second surgical site and has been shown to be useful in augmenting small areas of deficiency in the mandible. Use of allogeneic bone seems to be most effective in augmenting the width of the alveolar ridge and is much less effective in improving the height (vertical augmentation) of a deficient mandible. Current techniques for superior border augmentation of the mandible frequently involve some combination of block grafting, supplemented with an allogeneic material such as freeze-dried bone mixed with BMP often contained in some type of mesh tray (Figure 15-6).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses