Sagittal discrepancies
The correction of sagittal discrepancy has been considered a common goal for the patient and the orthodontist. A large proportion of clinical situations is not a single entity and is often associated with significant skeletal and dental imbalances in sagittal plane. Traditionally, orthodontic assessment and diagnosis is mainly based on Angle’s sagittal classification of malocclusion.1 Since the dentofacial abnormalities exist in sagittal, transverse and vertical planes, contemporary orthodontic assessment and interpretation must include their understanding in all three dimensions. While studying the various abnormalities in anteroposterior plane, it is also important to identify vertical discrepancies, as their presence impacts the sagittal dimension.
This chapter deals with the systematic approach to the diagnosis and treatment planning of various sagittal discrepancies based on redefined treatment goals, treatment options at various stages of development and their resolution with appropriate treatment mechanics and long-term stability.
The sagittal discrepancies essentially include Class I, Class II and Class III malocclusions; however, defining any one of these malocclusions is difficult because this arbitrary categorization consists of various abnormalities. In their original interpretation and understanding, these abnormalities represent the anteroposterior relationship between the maxillary and the mandibular first permanent molars as described by Edward H. Angle.1 Therefore, this approach does not recognize the dysplastic skeletal sagittal relationship of the maxilla and mandible to each other and to the cranial base. It is critical to identify and assess vertical discrepancies and understand their role in anteroposterior malrelationships. Equally important has been the proper understanding of the functional adaptation to the sagittal and vertical discrepancies. This leads to a posterior and occasionally anterior condylar displacement or autorotation of the mandible due to deficient posterior or excessive anterior facial height.2
The traditional approach to the diagnosis of sagittal discrepancies based on the molar relationship or the habitual occlusion does not reveal the abnormalities in the vertical dimension and in the condylar position in the fossa, dictated by the occlusal guiding forces and the neuromuscular adaptation. Therefore, a contemporary approach should address all these areas in differentially diagnosing variety of sagittal discrepancies. The diagnosis, treatment planning and the orthopaedic and orthodontic management of various Class II and Class III clinical situations and their interaction with the vertical dimension form the basis for this chapter.
Development of a sagittal problem
Various factors play an important role in the development of sagittal discrepancies. Identifying and understanding the involvement of specific causative factors is essential in developing an effective treatment plan. Growth disturbances, tooth size, crowding or spacing of teeth, height of palate and length and width of arch are all influenced by heredity. These, in turn, significantly contribute to the development of Class II and Class III malocclusions. An injury to the maxilla during growth can produce retardation of growth resulting in Class III relationship, while trauma during pregnancy or birth injury damaging the condyle can lead to Class II relationship. Congenital defects like cleidocranial dysostosis, leading to retruded maxilla and prognathic mandible; cerebral palsy resulting in loss of muscular coordination; Down’s syndrome (Mongolism); hypothyroidism leading to underdevelopment of mandible and Pierre Robin syndrome resulting in micromandible are all responsible for the development of Class II malocclusion. Class II relationship is also caused by certain local factors like anomalies in number of teeth – missing teeth and supernumerary teeth; anomalies of form and position – large teeth, ectopic positions and transpositions and tootharch disproportion – spacing and crowding. Abnormal pressure habits like thumb sucking and tongue thrusting significantly contribute to the development of sagittal discrepancies. In patients with nasal obstruction, tongue is held in forward position to keep the airway patent leading to short and constricted maxilla and long and expanded mandible. Disturbances in eruption sequence and timing can often result in occlusal interferences leading to a pseudo Class III malocclusion. Certain other factors, like extracted or missing teeth and their nonreplacement, result in drifting of adjacent teeth, thereby developing a dental sagittal discrepancy.
Diagnosis of sagittal discrepancies
Since sagittal discrepancies consist of various components and are often associated with abnormalities in other planes of space, their accurate diagnosis is a key element in the design of any successful treatment plan. It is essential to obtain adequate information about patient’s problem through the analysis of high-quality diagnostic records in order to improve diagnostic capabilities. However, increased amount of patient data requires thorough analysis and makes the process of interpretation a complex process. Therefore, a systematic approach to diagnosis is the key to redefining treatment goals and treatment planning of various sagittal discrepancies and their resolution with appropriate treatment mechanics to ensure long-term stability.
Class II malocclusion
‘Class II’ is a broad term designated to a set of various abnormalities that could be either simple or most complex. It is not a single clinical entity, rather it consists of various components of the craniofacial complex having variations in size, shape and position.3 In order to plan an appropriate treatment, the clinician should localize and quantify any skeletal and dental contributions, sagittal and vertical variations and the role of abnormal function and habits to the development of Class II malocclusion. There are many different types of Class II patients with significant variations in skeletal, dental and soft tissue morphology.
Clinical examination and functional assessment
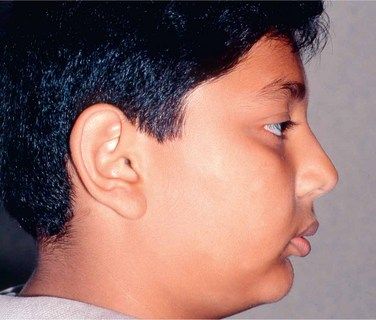
Improvement in facial profile is the most important factor considered by most patients seeking orthodontic treatment. Therefore, the focus of orthodontic treatment should be to achieve pleasing facial profile and soft tissue characteristics rather than just cephalometric norms. In the past few years, the scope of orthodontic assessment and treatment has been expanded, and the ability of the orthodontist to remarkably improve the patient’s facial appearance has also been considerably enhanced.4 During the process of clinical examination, while evaluating patient’s profile, it is important to study total profile, lip projections and nasolabial angle (Fig 3.1).
Functional assessment
Functional assessment is performed during the clinical examination for planning treatment for Class II malocclusions, especially in growing patients.
The above-mentioned parameters are of particular interest in establishing soft tissue or facial aesthetic goals, as the face is considered to be the determinant of orthodontic treatment.
Morphologic characteristics
As a clinician, it is critical to identify and locate the structures at fault with the help of cephalometric analysis, which are mainly contributing to the development of Class II malocclusion (Fig 3.3). Their understanding is essential to establish treatment goals and plan a treatment to resolve them. The first simple step is to find out whether it is dental or skeletal Class II malocclusion. Dental Class II malocclusion is caused by tooth migration, which may be confined to the entire arch or a segment of the arch following a missing tooth or abnormally displaced teeth. Skeletal Class II malocclusion could be as a result of prognathic maxilla and normal mandible, retrognathic mandible and normal maxilla or a combination of both – prognathic maxilla and retrognathic mandible. This is just a broad understanding of Class II malocclusion, whether it is dental or skeletal, and identifying the component involved. The Class II patient should be further analyzed cephalometrically to ascertain the involvement of vertical discrepancy or whether it is purely horizontal in nature.
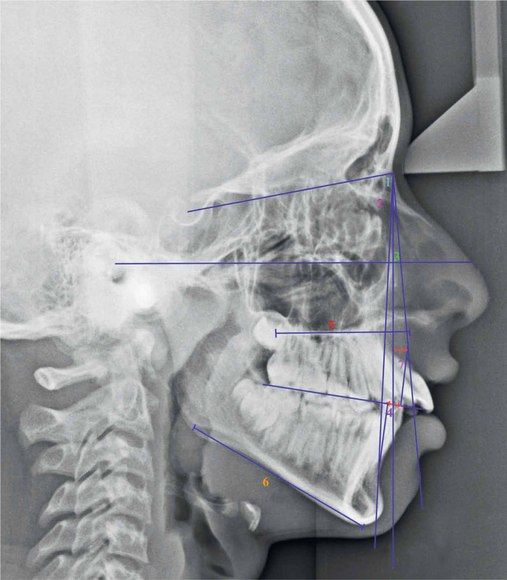
Figure 3.3 Cephalometric assessment (Class II malocclusion). 1, SNA; 2, SNB; 3, ANB; 4, Wits appraisal; 5, Maxillary length; 6, Mandibular length; and 7, Point A – nasion perpendicular. (For a detailed sagittal cephalometric assessment refer to Figures 1.35–1.39 in Chapter 1.)
Björk5 divided Class II malocclusions into forward and backward rotators and suggested that forward rotators are more common and easier to treat than the backward rotators. Classification of Class II malocclusion to group together cases having predominantly similar features is useful for the clinician to design a common treatment. These can be broadly classified as following horizontal types.6
Horizontal types: There are many variations in horizontal types of Class II malocclusions ranging from those having normal skeletal features but Class II dental characteristics to distinctly different skeletal types (Fig 3.4).
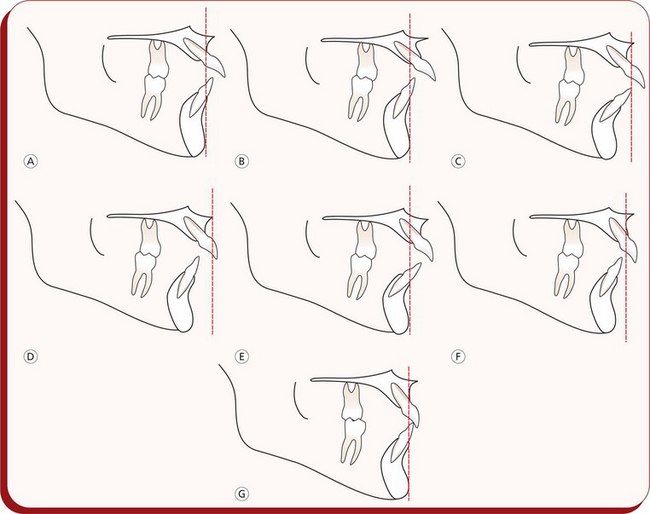
Figure 3.4 Horizontal morphologic characteristics of Class II malocclusion based upon the study by Robert Moyers. (A) Maxillary dental protraction. (B) Midface prognathism. (C) Maxillary retrognathism, dental protraction and mandibular retrognathism, dental protraction. (D) Mandibular retrognathism, maxillary retrognathism and maxillary dental protraction. (E) Maxillary prognathism and dental protraction. (F) Mandibular retrognathism. (G) Normal maxillary and mandibular dental and skeletal relationships.
Functional class II with a distally forced bite
This is a functionally created Class II malocclusion, having normal postural rest position but a forced mandibular retrusion in habitual occlusion. The path of closure of the mandible is abnormal or forced; quite often, associated with an infraocclusion of buccal segment teeth leading to an excessive overbite.
In addition to this, it is important for the clinician to predict the Class II malocclusion as forward or backward rotator. Four of the variables – mandibular inclination, shape of the lower border of the mandible, inclination of the symphysis and intermolar angle, when combined, give the best prognostic estimate of mandibular growth rotations.7
Class III malocclusion
Class III malocclusion generally manifests at an early age, and it is one of the difficult clinical situations to treat. The factors responsible for development of Class III malocclusion are different from those in Class II situation. As compared to Class II relationships, most Class III problems have a strong hereditary component.8,9 Environmental influences like habits and mouth breathing also play an important role in the development of Class III malocclusion. A growth stimulus from the constant distraction of the mandibular condyle in patients with abnormal mandibular posture can result in excessive mandibular growth.10 Class III malrelationships are often associated with morphologic and functional consequences. Patients with Class III problems may present with an impairment of dentofacial aesthetics and occasionally with psychological issues. This clinical situation may lead to incorrect loading of the teeth; chewing and speech functions may be altered. The prosthetic rehabilitation of the case may be difficult.
Like Class II malocclusion, Class III malocclusion is not a single clinical entity, rather it consists of various components of dentofacial complex.11 In a broader perspective, it is generally considered to be a manifestation of mandibular prognathism or midface deficiency or a functional forward shift of the mandible on closure to occlusion. Therefore, it could be skeletal Class III, dental Class III or ‘pseudo’ Class III, all resulting from a variety of combinations.
It is critical for the orthodontic professional to localize the disharmonious elements contributing to the Class III malocclusions. Other affected areas in the dentofacial complex of individuals having Class III malocclusions also include larger mandibular plane angles, larger gonial angles, longer mandibles and compensations of the dentition with maxillary dentoalveolar protrusion and mandibular dentoalveolar retrusion.12 While evaluating the Class III relationships, it is important to identify whether the problem is dental, caused by the improper inclination of the maxillary and mandibular incisors; functional, caused by the occlusal interferences; or skeletal, caused by the discrepancies of the maxilla and mandible. Therefore, the evaluation of a patient with Class III morphology should have a prescribed protocol to include (1) assessment of general facial morphology, (2) identification of abnormal components, (3) the vertical position of the mandible in posture and occlusion and (4) the position and angulation of the maxillary and mandibular incisors.
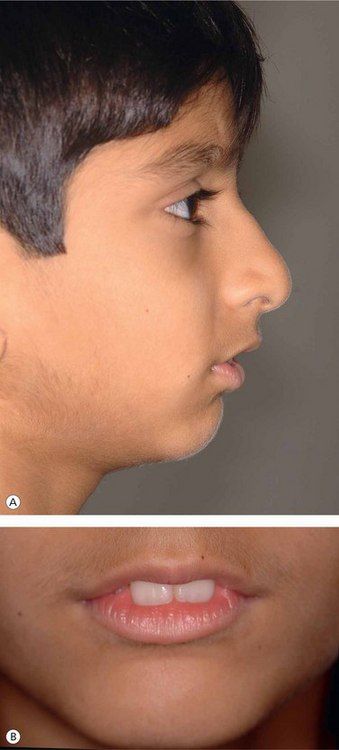
It is important to follow a well-organized and systematic approach to the diagnosis of patients with Class III malocclusion to determine the following variations in the Class III skeletal profile13 (Fig 3.5).
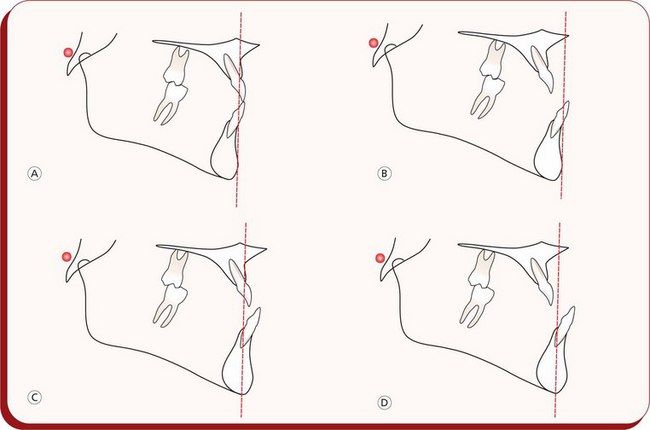
Figure 3.5 Variations in Class III skeletal profile. (A) Normal maxilla and mandible. (B) Maxillary retrusion and normal mandible. (C) Normal maxilla and mandibular prognathism. (D) Maxillary retrusion and mandibular prognathism.
Assessment of facial profile
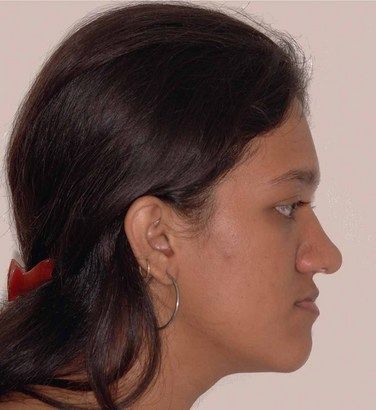
An evaluation of the facial profile should include an analysis of facial proportions, midface position, chin position and vertical proportions.14 This assessment is done to determine whether the patient’s profile is straight, convex or concave (Fig 3.6). Patients with maxillary deficiency usually exhibit a concave profile and flattening of the infraorbital rim and the area adjacent to the nose. It is essential to note that the facial convexity decreases as the patient matures.
Functional assessment
In patients with Class III malocclusion, it is critical to assess the relationship of the mandible to the maxilla to identify whether a centric relation (CR) and centric occlusion (CO) discrepancy exists. This is important because the anterior position of the mandible may be guided by abnormal tooth contacts that shift the mandible forward.
Patients having normal facial profile, Class I skeletal pattern and Class I molar relationship in CR with forward shift of the mandible on closure will exhibit concave profile, Class III skeletal and dental profile in CO. This clinical situation is called pseudo Class III malocclusion. However, patients with no shift of the mandible on closure are most likely to have a true Class III malocclusion. The key diagnostic feature in differentially diagnosing pseudo and skeletal Class III malocclusions is the gonial angle measurement that is usually more obtuse in skeletal Class III.15
Dental assessment
It is essential to assess the position and angulations of maxillary and mandibular incisors and the resultant interincisal relationship. The Class III relationship may be associated with an edge-to-edge relationship, a negative overjet or a positive overjet (Fig 3.7). If it is associated with a negative overjet, the clinician should proceed to functional assessment to differentiate between true and pseudo Class III malocclusion. If the Class III molar relationship is associated with a positive overjet or an edge-to-edge incisal relationship, a compensated Class III malocclusion is suspected. A compensated Class III malocclusion is a clinical situation where maxillary and mandibular incisors compensate for the existing skeletal Class III discrepancy.
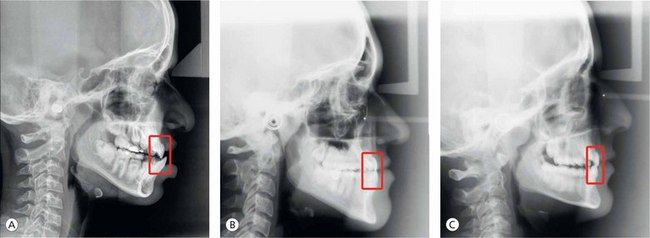
Cephalometric assessment
Patients with Class III malocclusion may present with a variety of combinations of skeletal and dentoalveolar components often associated with vertical and transverse discrepancies. Proper understanding of these components is essential to establish appropriate treatment plan so that the underlying cause of the discrepancy can be treated effectively.
Cephalometric analysis is a valuable diagnostic tool that drives the clinician to pinpoint the components responsible for the development of Class III malocclusion. While analyzing the anteroposterior relationship of maxilla and maxillary incisors and mandible and mandibular incisors, it is important to assess the vertical and transverse discrepancies associated with Class III malocclusion. The traditional approach to analyze patients with Class III malocclusion is to use ANB discrepancy. The patients with skeletal Class III malocclusion usually exhibit negative ANB angle with a smaller SNA angle and a larger SNB angle. However, individual variations in cranial base flexure and anteroposterior displacement of nasion often alter the ANB discrepancy.16 Therefore, alternative cephalometric measurements and analysis like Wits appraisal, effective maxillary and mandibular length and nasion perpendicular to ‘A point’ can be used to assess the anteroposterior relationship of the maxilla and mandible (Fig 3.8).
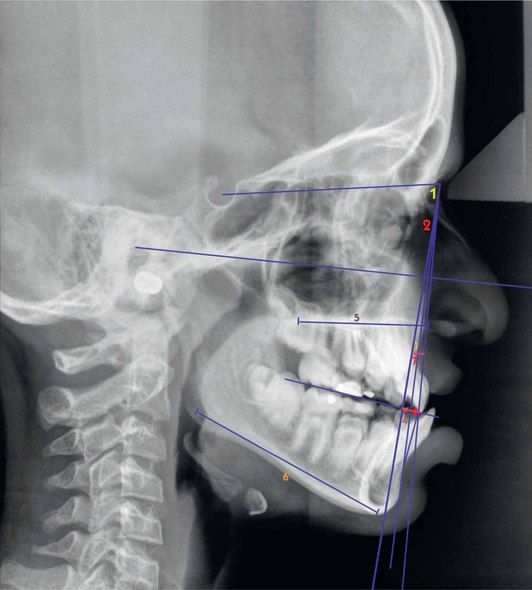
Figure 3.8 Cephalometric assessment (Class III malocclusion). 1, SNA; 2, SNB; 3, ANB; 4, Wits appraisal; 5, Maxillary length; 6, Mandibular length; and 7, Point A – nasion perpendicular. (For a detailed sagittal cephalometric assessment refer to Figures 1.35–1.39 in Chapter 1.)
Treatment planning
Establishing accurate diagnosis is the key element in formulating a successful treatment plan. The practitioner should focus on the development of an individualized treatment plan to improve the treatment results and shorten the treatment duration. The best way to approach treatment planning for a specific malocclusion is to define treatment goals as to what needs to be accomplished by treatment. These include facial, skeletal and dental goals. Making the most of available diagnostic information including the patient’s chief complaint forms a basis for establishing treatment goals. This often drives the clinician to an important process of a re-exploration of the diagnostic information and consideration of some important factors.
Treatment of sagittal discrepancies
There is no universal treatment approach that can address all sagittal discrepancies. As described earlier, Class II and Class III malocclusions are not a single clinical entity, rather they consist of various components. Quite often, they are associated with vertical or transverse discrepancies. Therefore, to design a treatment plan for a particular patient, the clinician should identify and locate the components involved.
There are various treatment methods and numerous appliances available to deal with different types of sagittal discrepancies depending upon the configuration of the malocclusion and the age of the patient. It should be noted that the response of the patient to a prescribed treatment plan is a major factor to be considered in achieving the desired result. Even similar malocclusions respond differently to similar treatment approach, and such differential response should be continually monitored to determine the need for necessary therapeutic alterations.
Treatment of class II malocclusions
There are several treatment strategies available to deal with different types of Class II situations. It is essential for the practitioner to select the appropriate treatment strategy depending upon the recognition of various elements contributing to the existing clinical problems. In other words, the treatment approach should be individualized. There are many Class II cases that require one or a discretionary combination of the various available treatment strategies. These include movement of teeth and alveolar processes, guidance of eruption and alveolar development, differential restraint and control of skeletal growth, differential promotion of skeletal growth, translation of parts during growth, training of muscles and surgical translation of parts.6
For the purpose of discussion, various Class II malocclusions can be grouped into the following categories:
Treatment of dentoalveolar class II malocclusion
Dentoalveolar Class II malocclusion patients present with normal skeletal jaw relationship and Class II molar position caused by mesial movement of maxillary molars with respect to mandibular molars during developmental stage (Fig 3.9). The unilateral Class II situation may exist due to mesial migration of maxillary permanent first molars following missing or abnormally positioned maxillary second bicuspids or premature loss of deciduous second molar on the affected side (Fig 3.9A and D). Patients with this abnormality are also associated with other parameters like varying degrees of overbite, overjet, crowding, rotations, etc. Not only the severity of Class II molar relationship but parameters like varying degrees of overbite, overjet, crowding, rotations, etc. also determine the complexity of treatment involved. After it has been established that the Class II malocclusion is dental in nature, the clinician should assess the position of all dental units in sagittal, vertical and transverse dimensions to define treatment goals and select appropriate treatment strategy. The contemporary orthodontic treatment illustrates that such patients will have numerous treatment goals and individualized treatment mechanics designed to address those goals. Specific treatment plans for individual patients fall into five major categories: growing patients, nongrowing patients, sagittal discrepancies, vertical discrepancies and transverse discrepancies.
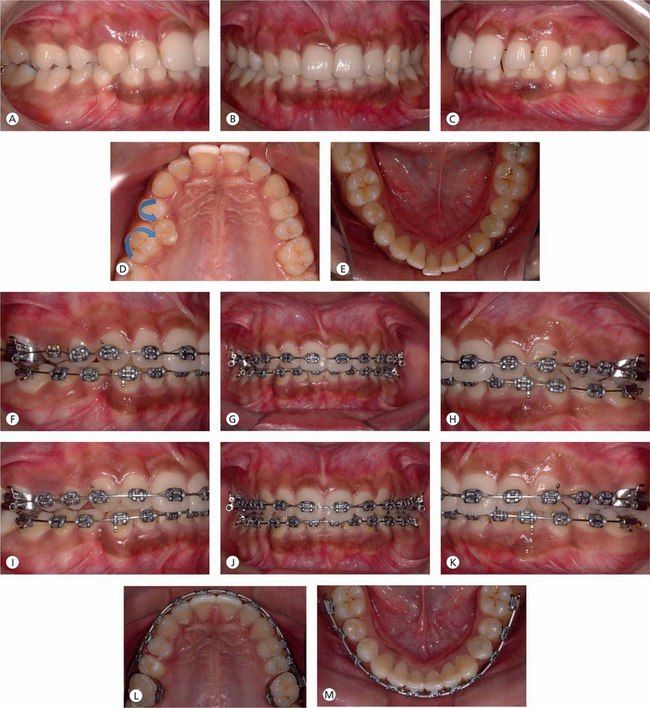
Figure 3.9 (A–E) Pretreatment intraoral photographs showing Class II molar relationship on right side, Class I molars on the left side and deep overbite. The Class II relationship on right side is due to mesiopalatal rotation of the first molar and distopalatal rotation of the first premolar as a result of palatal displacement of the second bicuspid. (F–H) After mesiobuccal rotation and distalization of the first molar to correct molar relationship and gain adequate space for the palatally placed second bicuspid, the second bicuspid is being moved into proper occlusion. (I) Establishing proper torque and fine-tuning the position of the maxillary right second bicuspid with finishing wires. (J–M) Midlines are corrected and proper occlusal relationship and coordinated upper and lower archforms are achieved.
Biologic variables: The basic strategy in the management of dentoalveolar Class II malocclusion is to achieve normal molar and incisal relationships, maintaining the existing normal skeletal relationship and the vertical dimension. Efficient tooth movement is ultimately the result of optimal biologic response to the orthodontic force system. The physiologic activity of alveolar bone resorption and deposition to produce tooth movement is induced by the mechanical stimulus through the delivery of orthodontic force systems. It is important that the force levels produced by orthodontic appliances are optimal, which will promote the most efficient treatment response without any damage to the teeth and the supporting structures (Table 3.1). The clinician should avoid excessive orthodontic force levels to prevent periodontal ligament necrosis and associated pain and bring about efficient tooth movement. It is essential to update on the knowledge of the force levels delivered to teeth through the medium of the appliance to understand optimal forces.26–28 These optimal force values depend on the type of the tooth and the size of the tooth.
Table 3.1
Optimal forces for orthodontic tooth movement
| Type of tooth movement | Force (g) |
| Tipping | 50–75 |
| Bodily movement (translation) | 100–150 |
| Root uprighting | 75–125 |
| Rotation | 50–100 |
| Extrusion | 50–100 |
| Intrusion | 15–25 |
Force values vary according to the size of the tooth; smaller values for incisors and higher values for posterior teeth.
Source: Proffit WR, et al. Contemporary orthodontics. 1993.
Dentoalveolar problems: Early treatment: The sagittal dental discrepancies in the primary dentition, seen in children having sucking habits, are expressed in the form of anterior displacement of upper incisors and posterior displacement of lower incisors. At this stage of development, if the sucking habit stops before the eruption of permanent teeth, it is usually self-correcting and therefore does not require any orthodontic intervention.
The mixed dentition phase is a very critical developmental stage. During this phase, children should be carefully examined and assessed for existing and potential or developing discrepancies. There are many treatment options available, depending upon the severity of the problem. The discrepancies in their severe form are best treated with two phases of treatment: phase 1 in the mixed dentition and phase 2 during the early permanent dentition period. It has been universally recognized that/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses