3
Pulmonary Disease
I. Background
Description of Disease/Condition
The prime function of the lungs is respiration to oxygenate tissues and remove carbon dioxide. Obstructive lung diseases are characterized by decreased expiratory flow rates and include asthma, chronic obstructive pulmonary disease (COPD), and cystic fibrosis (CF). Restrictive lung diseases are characterized by a decrease in the compliance of the lungs, the chest wall, or both, and are often due to pulmonary fibrosis or neuromuscular diseases affecting the respiratory muscles.
Asthma
Asthma is a chronic, potentially life-threatening, inflammatory disorder of the airways associated with airway hyperresponsiveness to stimuli resulting in bronchial edema and narrowing of bronchial airways. It is marked by episodic exacerbations that lead to recurrent episodes of wheezing, breathlessness, chest tightness, and coughing that result in variable and often reversible airflow limitation.
COPD
COPD is a term used to describe preventable respiratory disorders that involve airway obstruction that is not fully reversible. Examples of COPD are chronic bronchitis, peripheral airway disease (bronchiolitis), and emphysema. These often present with overlapping symptoms, the most characteristic being cough and sputum production that may precede the development of chronic and progressive dyspnea.
CF
CF is an autosomal recessive disorder. Most carriers are asymptomatic. CF is a disease of exocrine gland function that primarily involves the upper and lower airways, pancreas, and gastrointestinal and reproductive systems. CF is diagnosed by measuring electrolyte levels in sweat, particularly chloride. Production of abnormally thick mucus in the lungs leading to chronic respiratory infections and pancreatic enzyme insufficiency leading to malnutrition are common occurrences.
Restrictive Lung Diseases
Restrictive lung diseases are characterized by a decrease in the total volume of air that the lungs are able to hold. It can be caused by a decrease in the elasticity of the lungs themselves, weakness of the chest wall muscles during inhalation, or conditions that increase the size of the abdomen and limit movement of the diaphragm.
Tuberculosis (TB)
TB is an infectious and communicable disease caused by Mycobacterium tuberculosis. Its transmission is person to person through the inhalation of infectious respiratory droplets that become airborne when a person with active TB disease of the lungs speaks, coughs, sneezes, or sings.
Obstructive Sleep Apnea1 (OSA)
Obstructive sleep apnea syndrome (OSAS) is characterized by partial or complete upper airway obstruction during sleep, causing apnea and hypopnea, coupled with daytime symptoms, most often excessive sleepiness.
- Apnea is the cessation of airflow at the nose or the mouth for at least 10 seconds.
- Hypopnea is a 30–50% reduction in airflow for at least 10 seconds and oxygen desaturation of at least 2–4%.
- The apnea-hypopnea index (AHI) is the number of apneas and hypopneas per hour of sleep.
- OSAHS is obstructive sleep apnea/hypopnea syndrome.
- Mild cases have an AHI of 5–14.
- Moderate cases have an AHI of 15–30.
- Severe cases have an AHI >30.
Patients with moderate to severe OSA have significantly increased mortality. Even mild-to-moderate OSA (AHI 5–15/hour) increases the risk for hypertension, stroke, myocardial infarction and injury due to motor vehicle accidents.
Lung Cancer
Lung cancer forms in tissues of the lungs, usually in the cells lining air passages. The two main types are small cell lung cancer and non-small-cell lung cancer.
Lung Transplantation
Lung transplantation can prolong and improve the quality of life for patients with severe end-stage pulmonary disease. The majority of lung transplants are performed for patients with severe COPD/emphysema, idiopathic pulmonary fibrosis, CF, and pulmonary arterial hypertension.
Pathogenesis/Etiology
Asthma
Exposure to a trigger produces release of histamine and cytokines that result in bronchospasm, hypersecretion of mucus, and diminished ciliary motion.
There are two main types of asthma, categorized by the trigger stimulus:
- Extrinsic (or allergic) asthma
- Accounts for over 50% of asthma (>90% in children)
- Triggered by activation of mast cells and histamine degranulation following exposure to allergens such as dust, pet dander, mold, and pollen
- Intrinsic (or nonallergic/idiopathic) asthma
- Tends to occur after the age of 30
- Triggered by respiratory irritants (e.g., tobacco smoke and air pollution), respiratory infections, exercise, cold air, anxiety and stress, and gastroesophageal reflux disease (GERD)2
A subtype of intrinsic asthma is induced by aspirin and other nonsteroidal anti-inflammatory (NSAID) medications. This is not an allergic reaction but appears to be the result of these medications’ effect on cyclooxygenase.3
About 10% of asthma sufferers will have both extrinsic and intrinsic triggers. Symptoms are frequently worse at night or in the early morning. Pulmonary function testing generally shows airflow limitations that reverse with bronchodilator therapy.
COPD
COPD is a progressive disease associated with an abnormal inflammatory response to noxious agents, such as tobacco smoke or occupational/environmental pollution. Chronic inflammation causes narrowing of the small airways that decreases airway flow and destroys lung parenchyma and alveolar walls. This leads to decreased elastic recoil, diminishing the ability of the airways to remain open during expiration. Airflow limitation and lung function are best measured by spirometry, which measures the amount (volume) and/or speed (flow) of air that can be inhaled and exhaled. Classification of the severity of impairment is listed in Table 3.1.
Table 3.1. Classification of COPD Severity
Adapted from Global Strategy for the Diagnosis, Management and Prevention of COPD, Global Initiative for Chronic Obstructive Lung Disease (GOLD).8
| Stage | Pulmonary Function Test Findings | Symptoms |
| I: Mild | Mild airflow limitations | +/− Chronic cough and sputum production; patient unaware of abnormal lung function |
| FEV1/FVC <70% | ||
| FEV1 ≥80% predicted | ||
| II: Moderate | Worsening airflow limitations | Dyspnea on exertion, cough, and sputum production; patient usually seeks medical care because of symptoms |
| FEV1/FVC <70% | ||
| FEV1 between 50% and 80% predicted | ||
| III: Severe | Further worsening of airflow limitations | Increased SOB, reduced exercise capacity, fatigue, repeated exacerbations impact quality of life |
| FEV1/FVC <70% | ||
| FEV1 between 30% and 50% predicted | ||
| IV: Very severe | Severe airflow limitations | Cor pulmonale (right heart failure), quality of life impaired, life-threatening exacerbations |
| FEV1/FVC <70% | ||
| FEV1 <30% predicted or FEV1 <50% predicted plus chronic respiratory failure |
FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; FEV, forced expiratory volume; SOB, shortness of breath.
Worldwide, the most significant cause of COPD is cigarette smoking:
- Approximately 20% of current smokers and 14% of former smokers have some degree of clinically significant COPD.4
- The degree of severity of COPD increases as the number of cigarettes smoked per day and the duration of smoking increases.
- Smoking cessation, even when significant airflow limitation is present, can lead to improvement in lung function and can slow or halt disease progression.
There are genetic factors that modify risk:
- A hereditary deficiency of alpha-1 antitrypsin, commonly seen in people of northern European descent, leads to accelerated development of emphysema and decrease in lung function in both smokers and nonsmokers, although smoking increases the risk significantly.5
Bacterial colonization may play a significant role in airway inflammation and the pathogenesis and progression of COPD. Respiratory tract infections have been associated with acute exacerbations of this condition.
COPD is characterized by a specific pattern of inflammation involving neutrophils, macrophages, and lymphocytes.
Bronchitis
- Airflow obstruction is the result of chronic inflammation of the bronchioles resulting in
- hyperplasia of the mucous-producing glands,
- edema of the mucosa,
- secretions resulting in narrowing of the airways.
- The lungs become poorly ventilated leading to hypoxemia, cyanosis, CO2 retention, and polycythemia.
Emphysema
- Airflow obstruction that hinders expiration develops when there is an irreversible enlargement of the bronchioles and the alveoli.
- Inflammatory mediators attract activated neutrophils that release proteases that break down connective tissue components and lead to destruction of alveolar walls resulting in enlarged air spaces and loss of elastic recoil of the lungs.
COPD results in progressive dyspnea and hypercapnia with increasing exacerbations and debilitation. COPD and its comorbidities must be treated continuously to control symptoms, improve quality of life, reduce exacerbations, and possibly reduce mortality. Death results mainly from cardiovascular diseases and respiratory failure in advanced COPD.
Restrictive Lung Diseases
Common causes include idiopathic pulmonary fibrosis, radiation fibrosis, scleroderma, sarcoidosis, eosinophilic pneumonia, scoliosis, myasthenia gravis, muscular dystrophy, and obesity. These underlying diseases are often progressive.
TB
The lungs are the most common site of TB infection. Once an airborne droplet containing TB bacillus is inhaled, it travels through the lungs to the terminal bronchi and alveoli. In hosts with healthy immune systems, the majority of the bacilli are destroyed. The ones not immediately destroyed can enter the bloodstream and spread throughout the body infecting other sites, or remain in the alveolus. Within 2–6 weeks, the bacilli are engulfed by macrophages that form a barrier shell, called a granuloma that keeps the bacilli contained and prevents systemic dissemination, resulting in latent TB infection (LTBI).
Asymptomatic LTBI occurs in 90% of those infected with the bacilli, with only a 10% lifetime chance of progressing to TB disease. Patients with LTBI are not infectious and cannot spread organisms to others. Progression from LTBI to TB disease occurs when the immune system cannot prevent the TB bacilli from multiplying. Coinfection with HIV is the strongest risk factor for progressing to active TB disease, and TB is one of the leading causes of death among people infected with HIV worldwide. Other risk factors for developing active TB disease include diabetes, chronic and end-stage renal failure, hematological malignancies, and malnutrition.6
OSA
OSA is caused by a narrowed upper airway and increased collapse of the muscles and soft tissues. As the muscles and tongue relax during sleep, they can partially occlude the opening to the airway and cause increased resistance to airflow. Risk factors include obesity, smoking and alcohol use, having hypertension, or any anatomical deviation that narrows the dimensions of the upper airway including deviated nasal septum and enlarged turbinates, elongated soft palate and uvula, retrognathic mandible, enlarged tongue, and redundant parapharyngeal folds. Sleep apnea can affect multiple family members, suggesting a possible genetic basis.
Lung Cancer
Most lung cancers fall into three pathological types: squamous cell carcinoma, adenocarcinoma, and small-cell (oat-cell) carcinoma. Thoracic symptoms can include cough, hemoptysis, wheezing, and pleural pain. Extrathoracic signs and symptoms are due to metastasis, which is common to the liver, adrenal glands, brain, and bone. Nonspecific signs include anorexia, weight loss, weakness, and fatigue.
Epidemiology
Asthma
Prevalence, hospitalizations, and fatal asthma exacerbations have all increased in the United States over the past 20 years. Centers for Disease Control and Prevention (CDC) statistics show 34 million or 1 in 9 Americans have been diagnosed with asthma during their lifetimes, with 12.3 million having experienced an asthma attack in the previous year. In 2008, asthma was responsible for 1.6 million emergency department visits and almost half a million hospitalizations.7
COPD
It is the fourth leading cause of chronic morbidity and mortality in the United States, and is projected to rank fifth in 2020 in burden of disease worldwide.8
CF
CF is the most common lethal inherited disease among Caucasians (occurring in the United States in 1:3200–3500 newborns)9 and the most common cause of obstructive airway disease in patients under 30 years. End-stage lung disease is the principal cause of death 90% of the time9 with the average life expectancy around 37 years.
TB
The CDC recently estimated that one-third of the world’s population is infected with TB, with 9 million developing active TB disease each year, and nearly 2 million TB-related deaths annually. Most of these cases are in Southeast Asia and Sub-Saharan Africa. In the United States, TB has shown a steady decline, with the number of reported TB cases in 2010 (11,182) the lowest recorded since 1953.10
OSA
An estimated 18 million Americans have sleep apnea. It affects all ages, although the incidence is highest in middle-aged persons. It is more common among men. The incidence and prevalence depend on the criteria used to define the syndrome. As many as 40–60% of all adults age 60 or older have some form of sleep-related breathing disorder, most commonly snoring, which is a significant risk factor for OSA. In a random sample of employed Americans aged 30–60 years, 9% of women and 24% of men had AHI scores of 5 or higher accompanied with complaints of daytime sleepiness.11The incidence of OSAS in children is 1–3%.
Lung Cancer
Lung cancer is the leading cause of cancer deaths in the United States, with over 160,000 deaths annually, and the second leading site of new cancers for both genders after prostate cancer for men and breast cancer for women.12 Smokers are 10–20 times more likely to get lung cancer. Smoking is the principal cause of about 90% of lung cancer in men and almost 80% in women, followed by asbestos and silica exposures. Most patients are clinically asymptomatic until late in the disease course, resulting in a mean survival time of 9 months after diagnosis.
Lung Transplantation
A total of 30,673 lung transplants were done worldwide between 1995 and 2010.13 Lung transplant patients have the highest mortality rate of organ recipients. Survival rates for all types of lung transplants are 79% at 1 year, 64% at 3 years, 53% at 5 years, and 30% at 10 years.13
 Coordination of Care between Dentist and Physician
Coordination of Care between Dentist and Physician
Many dental patients with these pulmonary diseases can receive the full range of dental treatments with minor adjustment, but in those patients with more severe disease, the consequences of airway obstruction and the subsequent hypoxic state may require modification for safe delivery of dental care. Important aspects of care coordination include the dentist gaining an understanding of the pulmonary disease severity, importance of controlling oral bacteria that can be aspirated, awareness of triggers and medications to avoid, and the potential spread of infectious pulmonary conditions. Dentists also play a role in the management of OSA by fabrication of oral appliances.
 II. Medical Management
II. Medical Management
Identification
Obstructive and restrictive lung diseases have different etiologies, but often have overlapping symptoms. A thorough medical history coupled with a comprehensive physical exam, review of systems and review of current and past use of tobacco products are the key to accurate diagnosis of pulmonary diseases. A nonspecific sign of significant cardiopulmonary disease is clubbing of the fingers and bluish fingernails as shown in Fig. 3.1.
Figure 3.1 Clubbing of the fingers in a 22-year-old with advanced cystic fibrosis.

Medical History/Physical Examination
Asthma
Asthma has a wide spectrum of clinical severity. The intensity of airflow obstruction determines the severity of an acute event and the frequency and severity of airflow obstruction between episodes determines the severity of the disease. Symptoms used to assess level of asthmatic control are shown in Table 3.2.
Table 3.2. Assessment of Asthma Control
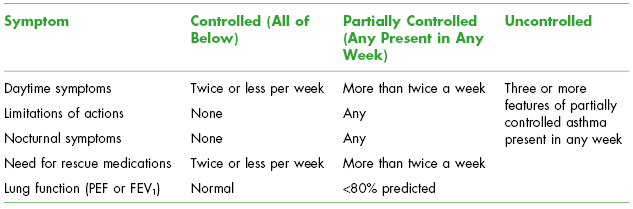
PEF, peak expiratory flow.
Most patients have mild to moderate asthma and function normally with minimal to no symptoms between attacks, although individual attacks can still produce moderate to severe symptoms. See Table 3.3 for the classification of asthma severity. Attacks occur in paroxysms with rapid onset of chest tightness and airflow obstruction, dyspnea with decrease in forced expiratory volume in 1 second (FEV1), coughing, wheezing, tachypnea, and tachycardia. Status asthmaticus is a prolonged, severe asthma attack that does not respond to bronchodilator therapy leading to fatigue, cyanosis, tachycardia, and pulsus paradoxus (decrease in systolic blood pressure >15 mmHg with inspiration), and ultimately resulting in respiratory failure and death if not reversed.
Table 3.3. Classification of Asthma
Adapted from the National Asthma Education and Prevention Program.2
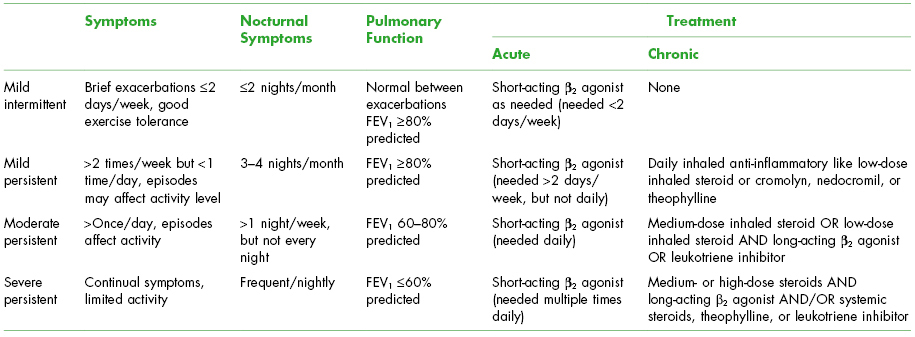
Features that are associated with increased risk of adverse events include poor clinical control and/or frequent exacerbations despite high-dose medications, presence of nocturnal symptoms, need for emergency room visits, low FEV1, and cigarette smoking.
COPD
COPD has an insidious onset. Clinical features include chronic cough that eventually progresses to dyspnea on exertion. For the diagnosis and assessment of COPD, spirometry is the gold standard. The presence of FEV1/forced vital capacity (FVC) <70% confirms the presence of airflow limitation that is not fully reversible, with FEV1 serving to quantify the degree of airflow impairment. Both chronic bronchitis and emphysema show marked decrease in the FEV1/FVC ratio.14
Arterial blood gas analysis looking at levels of hypoxia and hypercapnia can be used to individualize the diagnosis, prognosis, and treatment regimen. In chronic bronchitis, chest radiographs may show prominent vascular markings and bronchial thickening, while in emphysema, there are marked signs of hyperinflation (flattened diaphragm on the lateral chest film and an increase in the volume of the retrosternal air space) and a relatively small heart.
Two clinically distinct types of COPD patients exist, although many patients with COPD have elements of both diseases:
| Chronic bronchitis (blue bloaters) | Emphysema (pink puffers) |
| Overweight | Thin with barrel chest |
| Productive cough/mucopurulent sputum | Dry cough/little sputum |
| Inspiratory/expiratory wheeze | Expiratory wheeze |
| Mild dyspnea | Severe dyspnea |
| Frequent infections | Infrequent infections |
| Enlarged heart | Enlarged chest and small heart |
| Severe hypoxia/hypercapnia | Mild hypoxia/hypocapnia |
| Polycythemia | Normal hematocrit |
| Cor pulmonale common | Cor pulmonale rare |
| Respond to bronchodilators | Poor response to bronchodilators |
Restrictive Lung Diseases
Symptoms include cough, dyspnea on exertion, wheezing, and chest pain. Pulmonary function tests show a decreased FVC and normal FEV. Patients with early interstitial restrictive lung disease may have normal arterial blood gas values, and cyanosis does not occur until the process is advanced. On physical exam, there is decreased chest wall movement, increased use of accessory muscles, and rapid, shallow breathing.
TB
Symptoms:
- LTBI: asymptomatic
- Active TB disease: general malaise, weakness, weight loss, fever, night sweats, and lymphadenopathy
- Pulmonary TB disease: chronic cough (present for more than 3 weeks), chest pain, and hemoptysis
- TB infections of other organs: symptoms specific to the organ affected
| Latent TB infection (LTBI) | TB disease |
| M. tuberculosis in the body | |
| Tuberculin skin test (Mantoux or purified protein derivative [PPD]) usually + | |
| Chest X-ray normal | Chest X-ray abnormal |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


