Pain and Anxiety Management
CHAPTER OBJECTIVES
Upon completion of the chapter, the reader should be able to:
1. Identify the physiologic mechanism of pain.
2. Appreciate the many variations of pain reactions among individuals.
3. Recognize methods for assessing and measuring pain.
4. Appreciate the relationship between pain and anxiety.
5. Recognize methods for assessing and measuring fear and anxiety.
6. Define the American Society of Anesthesiologists (ASA) levels of minimal, moderate, deep, and general analgesia-sedation.
7. Recognize the spectrum of pain and anxiety management options.
According to the American Pain Society (APS), pain is the leading public health problem in the United States and is the most common complaint by people seeking medical care.1 This organization also cites that pain is the reason why more than 50 million days of work are lost each year.1 It is estimated that $100 billion are spent in the United States annually for pain-related costs.1 This economic impact on the nation’s population affects all of our citizens directly or indirectly. Statistics also show that as many as 35 million people in the United States avoid the dental office because of their fear,2 and dental phobia affects 10 to 12 million people.3 Fear and pain are interrelated. People will endure severe pain before seeking professional care often because of the fear that is associated with pain.4 Individuals may find themselves in an emergency situation facing significant problems as a result of not having sought treatment at an earlier time when treatment could have increased the possibility of a favorable outcome. Smith and Heaton reviewed more than 200 articles and 19 studies regarding dental anxiety5 in 2003. Their results suggest that the prevalence of dental anxiety has not changed dramatically over the years even though there has been an increase in general anxiety in the United States.5 It appears dental anxiety exists globally as well.6 The subject of dental anxiety has been an ongoing topic for decades.
Managing a patient’s pain and anxiety provides an environment that benefits both patient and clinician. Obviously, if you, the clinician, know that your patient is relaxed and comfortable, you can provide better service with less stress (Figure 3-1). Effectively managing pain preoperatively, intraoperatively, and postoperatively is often the most challenging aspect of practice. Success, as a professional, is often defined by how one manages this aspect of patient care.
Many options are currently available for pain and anxiety relief. Some options in certain situations will prove more advantageous than others. But for many procedures, several methods could be used. Nitrous oxide/oxygen sedation will not manage all of your patients’ fear and anxiety, especially if it is severe, but it can certainly be useful for a majority of patients exhibiting mild to moderate preoperative apprehension.
1 Mechanism of Pain
A. Definition
As defined by the International Association for the Study of Pain, “pain is an unpleasant sensory and emotional experience arising from actual or potential tissue damage.1 The experience includes the perception of an uncomfortable stimulus and the response to that perception.”7
B. Principles of Action
1. The objective of pain is to provide damage protection to tissue by alerting the central nervous system (CNS) before or during a potentially damaging occurrence.
a. Pain receptors (nociceptors) are the first to receive a stimulus. These receptors are nonspecialized, bare nerve endings that record the occurrence, intensity, duration, and location of the sensation.8
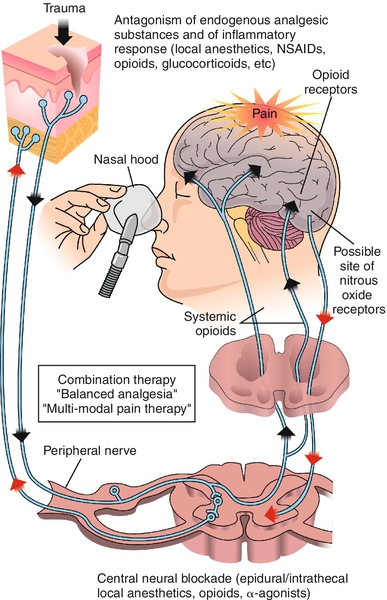
2. The theory of pain modulation suggests that impulses are altered along the way by an endogenous opioid system9 (Figure 3-2).
3. Exogenous morphine binds to an opiate receptor, which accounts for its analgesic properties. Morphine is the drug to which endogenous opiates and other opioid drugs are compared.9
4. Research has attempted to determine the effect of N2O on the endogenous opioid system. Gillman10 proposes that analgesic concentrations of N2O may act directly on the opioid receptor and/or activate the release of endogenous opiates.
5. There is a physiobiochemical relationship between N2O and opioids. Naloxone hydrochloride (Narcan) can produce reversal effects of opioid drugs. This drug is most commonly used in opioid overdose situations.11 Oxygen alone will replace N2O and thereby recover its effects.
6. Endogenous endorphins, enkephalins, and dynorphins have been discovered as substances that bind to the opiate receptors, resulting in pain modulation.8,9 Activation of the endogenous opioid system can be accomplished by pain and/or stress.12 Research of the endogenous opioid system continues.
7. Reactions to pain vary among individuals and can vary in the same individual from day to day. Many factors can influence pain reactions. Examples of these factors may be categorized as physical, mental, biochemical, psychogenic, social, physiologic, cultural, and emotional.7 The American Pain Society Task Force on Pain in Infants, Children, and Adolescents suggests that pain is subjective and multifactorial. They suggest that behavioral components are mixed with other factors, including environmental, developmental, and sociocultural factors.13 In a statement about the assessment and management of acute pain in young people, the American Academy of Pediatrics (AAP) and APS state that suffering occurs when pain is overwhelming or chronic.13
C. Assessing and Measuring Pain
1. A variety of scales are intended to objectify the levels of pain to allow clinicians to act appropriately and alleviate discomfort. In many cases the scales have been helpful to facilitate self-reporting; however, some have not been useful.14–17
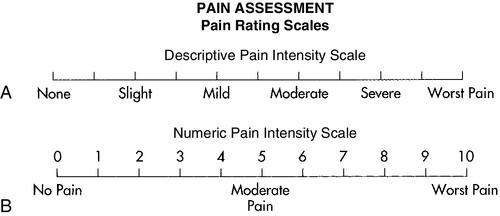
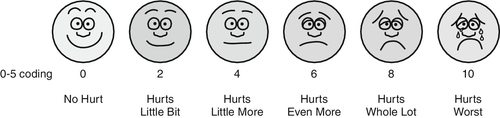
2. A common scale (represented as either vertical or horizontal) depicts pain in equal segments across the continuum from 0 (no pain) to 10 (unbearable). This visual analog scale can be used generally with any age group17,18 (Figure 3-3). Several other measures have been used; versions of various scales depict a range of facial images from comfortable to painful (Figure 3-4) for visually oriented populations such as children. Numeric scales prove useful when treating chronic pain, because they can serve as baseline references over time. Pain scales are deliberately simple to allow people to express themselves when their attention span is decreased and cognitive skills are impacted.
3. Even the simplest attempt to convey understanding of a patient’s pain is appreciated. For example, try to use a word for pain from the patient’s native language. Some examples are listed in Box 3-1. Word pronunciations can be found for many languages at the following website: www.forvo.com.
4. Asking patients about the extent of their pain communicates empathy toward those individuals. Problems occur when healthcare professionals are presumptuous about how a patient should or should not feel.
5. Practitioners rely on a variety of continuing education and clinical experiences to guide them toward successful management of pain. Inherent in this process is the ability to adapt to and change specific patient complaints. This process is dynamic and continuous; each experience should develop better decision-making skills for the future. Healthcare professionals gain confidence with successful decisions, which ultimately benefits the patient.
2 Understanding Fear and Anxiety
A. Definitions
1. Anxiety: “A nonspecific feeling of apprehension, worry, uneasiness, or dread, the source of which may be vague or unknown. A normal, rational reaction when one’s body, lifestyle, values, or loved ones are threatened.”7 Anxiety may be accompanied by restlessness, tension, tachycardia, and dyspnea.18
2. Fear: “A feeling of fright or dread related to an identifiable source recognized by the individual.”7
3. Phobia: “Any persistent and irrational fear of something specific, such as an object, activity, or situation that results in avoidance or desire to avoid the feared stimulus.”7 “Fear that is recognized as being excessive or unreasonable.”18
B. Interaction Between Fear and Pain
Fear and pain are so interrelated that they are often hard to separate. Both have physiologic and emotional components.19 As pain increases, anxiety is heightened; as anxiety increases, pain becomes enhanced and, therefore, less tolerable.8 In a medical setting, children cite fear of pain to be a significant obstacle.20 When fear or pain is an issue, both must ultimately be managed.
C. Assessing and Measuring Fear and Anxiety
1. Objectively quantifying a patient’s fear or anxiety poses a dilemma similar to pain. There are several methods of assessing fear. Physiologic and behavioral signs often are overt indicators of fear (“white knuckle syndrome” is depicted in Figure 3-5). A simple interview with a patient will uncover otherwise unspoken concerns. Similar to scales used with pain, many measurement devices indicate fear and anxiety. The literature is abundant with suggested indicators.21–24 Although modified, a classic, five-item anxiety questionnaire developed by Norman Corah asks patients to identify the level of anxiety associated with imm/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses