Chapter 3
Optimal Use of Dental Implants for Cosmesis: Creating Aesthetic Outcomes with Dental Implant Restorations
Introduction
A beautiful smile can be a true enhancement of facial cosmetics. For the smile to be perceived as a thing of beauty, certain parameters must be met. Proper proportions must be satisfied: tooth-to-tooth, tooth-to-gingiva, tooth-to-lip, and tooth-to-face and/or jaw.
The role of the dentist and implant surgeon is to diagnose, and plan and execute treatment in a manner that provides appropriate balance of these proportions; and to provide highly esthetic prosthetic restorations for single- and/or multiple-implant sites in the anterior esthetic zone of the patient’s smile, such that restorations mimic nature and blend in with adjacent natural teeth when present.
The purpose of this chapter is to provide clinical guidelines for creating esthetic restorations utilizing endosseous implants. The use of dental implants throughout the dentition, and more specifically in the more esthetically demanding maxillary and mandibular anterior region of the mouth, attempts to correct alterations in form and function due to the undesirable effects of caries, periodontal infections, or traumatic injury to the teeth and their supporting tissues. The process, which involves a true interdisciplinary approach, can be very delicate when involving the management of bone and soft tissue and the design of crown forms with carefully constructed physiological contours. The focus on this chapter will be on single and multiple implant-supported fixed restorations that will have an influence on cosmesis of the esthetic region of the mouth.1
Implant Esthetics
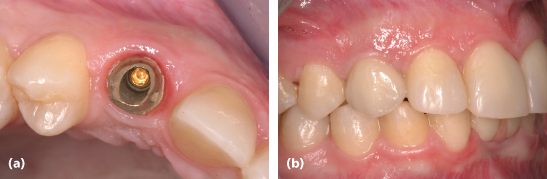
Esthetics and osseointegration were developing on parallel paths during the mid-1980s to the early 1990s and have emphasized the importance of the integrated team approach to achieve the ultimate periodontal and restorative result. When crowning or veneering existing teeth, maintaining the papilla between two teeth is somewhat predictable,2 whereas between a tooth and an adjacent implant (see Figure 3.1) is less predictable.3,4 Concern for the loss of or reduction in height of the papilla between two adjacent implants has created the most difficult esthetic dilemma.5 Therefore, the concepts of selective extraction of teeth, socket preservation, and augmentation at the time of tooth extraction appear to be invaluable in the restoration of form, function, and esthetics.6–11
Figure 3.1 (a) All-zirconia implant abutment. (b) Emergence profile/physiological crown contour of implant restoration. Note the thin facial tissue contour with slight discoloration from implant body. (c) Diminished height of interimplant-tooth papillae, with evidence of dark interproximal triangles.

Esthetics plays a major role in our diagnostic and therapeutic endeavors today. However, long-term clinical assessments have shown that its real value will play out optimally when it is achieved in concert with all the functional needs of the dentition.
Form and Function
Providing an Improved, Stabler Anterior Esthetic Outcome
Posterior bite collapse is the result of the loss of one or more posterior teeth, with drifting of adjacent teeth, extrusion of opposing teeth and the creation of uneven marginal ridge relations and adjacent cementoenamel junction (CEJ) levels, and concomitant uneven bony crests. These events establish an environment where the self-protective capacity of the teeth is compromised, resulting in the development of angular bony crests frequently predisposing to infrabony pocket formation and posterior interproximal caries. The occlusal vertical dimension is supported by the posterior occlusion but with posterior tooth loss, the forces of occlusion are often stronger or heavier on the remaining anterior teeth. In addition, the remaining anterior teeth must provide anterior guidance, disarticulating the posterior teeth through excursive movements of the mandible. This will have a significant impact on their long-term function and viability.12
When posterior bite collapse has occurred, the restoration of form and function is more difficult to accomplish. Posterior occlusion must be reestablished, the occlusal vertical dimension restored, and the anterior incisal guidance developed in concert with the posterior cusp height. This should allow for disarticulation of the posterior teeth during excursive movements of the mandible.
Ultimately, this will establish a more “outcome-based” approach to occlusal therapy. For example, when the patient is periodontally susceptible and the posterior teeth in the same arch are seriously compromised or missing, the remaining anterior teeth may be stressed unfavorably, demonstrating varying degrees of mobility.12 Placing posterior implants with fixed/splinted crown and bridgework is the preferred treatment for this patient type.12 The restoration of the posterior occlusion at the correct occlusal vertical dimension can significantly decrease or eliminate the mobility patterns present in the anterior teeth and thereby help to stabilize them. This situation arises frequently and by offering the functional posterior support, one can often preserve the natural architectural form of the anterior teeth and gingiva and improve esthetics by crowning or veneering the teeth alone. Of course, there are situations where one or more of these anterior teeth may be too weak or compromised to support normal function. Herein begins the dilemma of their replacement with endosseous implants and the desire to create the most esthetic, cosmetic result for the patient.
To understand the complexity of the treatment that must be undertaken to create esthetic implant and tooth outcomes, this chapter is divided into the following: constructs of the restoration, and preservation/augmentation and resection. They will provide you with a much more in-depth way of diagnosing and planning treatment to achieve high-level predictable outcomes.
Constructs of the Esthetic Implant Restoration
First, the behavior and maintenance of the height of the marginal soft and hard tissue and interproximal papillae around teeth and implants will be reviewed. This requires an appreciation of biological tissue dimensions for both teeth and implants, so that we may successfully predict a desired outcome. The soft tissue and underlying hard tissue morphology will be studied for purposes of developing the most physiological contours for the emergence of the crown forms for teeth and implants. Second, we will look closely at the various choices of dental crown materials to create beautiful tooth reproductions supported by the underlying endosseous implants and their respective abutments. Third, over the years, dentists have experienced a variety of endosseous implant designs, thread pitches, internal or external connections, surface textures, and implant-to-implant abutment connections. Each of these design features has an influence on the interfacial bone connection and the final soft tissue topography circumscribing each implant crown. One can start to see how the implant crown restoration may be influenced in multifold ways that will affect esthetic outcomes. Last, the study of the implant restoration often involves teeth that may have been lost at an earlier time in the esthetic zone and the residual ridge may have retreated such that the bone and gingival complex may be 0.5–5+ mm apical to the adjacent regions housing natural teeth. This section will conclude with an appreciation of how to design and construct implant prostheses to achieve cosmetic as well as functional outcomes for these severely compromised single- or multiple-tooth residual ridge sites.
Restoration of Teeth
Esthetic Treatment Approach
When a patient’s needs are primarily restoratively focused, such as veneering or crowning one or more teeth, gingival aesthetic guidelines will be a significant component of the overall effort. In order to properly address the esthetic requirements of the patient, it is necessary to envision the desired outcome before performing the procedure.
Esthetics is fundamentally about tooth form, and it is therefore most predictably realized with the assistance of an intraoral diagnostic composite “mock-up” to simulate the improved incisal tooth form, lip line esthetics, and gingival topography (see Figure 3.2). Molds of the improved intraoral anatomical form of the teeth should be poured in stone, and then enhanced further in the dental laboratory with the application of wax. Based on the mock-up, the wax patterns should be completed to the desired occlusal scheme with careful attention to the functional guidance features of the anterior teeth. The wax patterns are then processed in acrylic or a composite resin material to fabricate provisional restorations to be used intraorally. Silicone impressions are fabricated by the laboratory and then returned to the clinician to be used to verify proper tooth reductions.13 The outcome of the diagnostic mock-up is the development of an intraoral esthetic blueprint. This results in dentist verification, improved laboratory communication, and patient affirmation.
Figure 3.2 (a and d) Pretreatment view of incisal plane, gingival topography, and incisal plane relative to lip line. (b and e) Diagnostic composite mock-up to demonstrate enhanced tooth form, incisal plane, and their relationship to the mandibular lip line. (c and f) Final ceramic crowns with improved incisal plane and relationship to lip profile.

Periodontal Biotypes
Ochsenbein and Ross,14 Weisgold,15 and Olsson and Lindhe16 suggested two distinct types of periodontium found in humans. Becker and colleagues17 reported that there are three periodontal biotypes: flat, scalloped, and pronounced scalloped. Measuring from the height of the bone interproximally to the height at the direct midline, their findings were as follows: flat = 2.1 mm; scalloped = 2.8 mm; and pronounced scalloped = 4.1 mm. Note that the distance in the pronounced scalloped is approximately twice as great as in the flat type. Normally, the distance from the CEJ to the crest of bone on the direct facial in a healthy periodontium of a young adult is approximately 2 mm, with the gingival margin being located on the enamel (slightly coronal to the CEJ). However, in the pronounced scalloped type, the distance between the CEJ and the bone on the direct facial is usually 3–4 mm. This results in the gingival margin being located at the CEJ, or quite often, on the cementum; that is, in the pronounced scalloped type, the gingival margin is, in a sense, located on the root in health. This type of periodontium, because of its thinness and friability, is more likely to recede than the flat type. There is no question that the most favorable gingival and esthetic restorative result occurs in the flat type, not in the pronounced scalloped type.
Tarnow and colleagues2 observed that in healthy mouths the gingival papilla filled the space between teeth 100% of the time when the distance from the contact point of adjacent teeth to the interproximal crest of bone was 5 mm or less. When the distance was 6 mm, the papilla did not fill the space completely in approximately 50% of the patients, and when it was 7 mm or more, it did not fill the space in about 75% of the cases. The pronounced scalloped periodontal biotype (because of its triangular-shaped tooth) usually has a distance between 6 and 7 mm. Hence, under normal conditions, this is the tissue type that usually has some interproximal recession with the formation of “black triangles” between adjacent teeth. Further clinical insults to soft tissue, such as tooth preparation, excessively rapid orthodontic tooth movement, tooth extraction, scaling and root planning, and injudicious retraction of soft tissue may increase the gingival recession, thus further compromising the esthetic result.
The extraction of an anterior tooth usually results in resorption of bone on the facial and interproximal surface. In addition, a decrease in the faciolingual dimension of the interproximal areas is common. These findings are more obvious in the scalloped type of periodontium, and even more so in the pronounced scalloped type. This may create an esthetic dilemma for both the patient and the dentist. Complicating the matter is that the morphology of the roots of the anterior teeth is usually more tapered both faciolingually and mesiodistally than those found in the flat-type periodontium. The results of extracting an anterior tooth with a scalloped-type periodontium are (1) greater loss of interproximal hard and soft tissues; (2) more palatally positioned interproximal papillae; and (3) a wider mesiodistal dimension between the adjacent teeth (because of the taper of their roots). The outcome is a large noticeable black triangle, which is often treated by closing the space with a wider crown or laminate placed on the adjacent teeth, or with the use of pink porcelain to simulate the lost gingiva.1 Often these options are not satisfactory.
The incorporation of one single-tooth implant and crown, together with adjacent natural teeth or with a series of all ceramic crowns or veneers for the adjacent natural teeth, creates a great challenge for the clinician and dental ceramist.6 Endosseous implant installation requires careful staging, in accordance with the healing time frames associated with tissue maturation. The addition of bone and soft tissue at or after tooth extraction, or tooth lengthening by restorative and/or surgical measures to achieve esthetic outcomes, requires even greater interdisciplinary planning. Let us study them as we address their issues in the sections below.
Implant-To-Implant Distances
Romeo et al.,18 in a study involving 48 subjects, noted that when the interimplant-tooth distances were between 2.5 and 4.0 mm, the papilla was significantly present. Also, the subjects with a thick biotype correlated with frequency of papilla presence (see Figure 3.3).
Figure 3.3 (a) Gold implant abutment with collar following the papilla form. (b) Thick tissue biotype wherein implant crown supports the interproximal papillae and the papillae fill the implant-tooth interproximal spaces completely.
In studying interimplant distances, Degidi et al.19 demonstrated that in immediately placed and immediately restored implants, implants with an interimplant distance of greater than 2 mm lost less bone laterally. Vertical bone loss was greater when the interimplant distance was less than 2 mm. They concluded that to guarantee an esthetic outcome in immediately placed and immediately restored implants side-by-side, the contact point of the crowns should be placed at 3–4 mm and never greater than 6 mm from the peak of the interproximal bone. Also, the implants should be placed adjacent each other at a distance greater than 2 mm and less than 4 mm.
Diagnostic Evaluation
Diagnosis, treatment planning, and treatment sequencing continue to be significant challenges for the general dentist and specialist in the management of the partially edentulous patient. A comprehensive dental/periodontal examination must first be performed. This will ensure that all members of the treating team have addressed each problem area and have collated their respective treatments into the overall therapeutic program.
The clinical evaluation consists of caries, periodontal, endodontic, orthodontic, orthognathic, occlusal, and temporomandibular joint exams, as well as a comprehensive physical evaluation or medical history. To facilitate this diagnostic evaluation, a full-mouth series of periapical radiographs of teeth and residual ridges must be obtained. A panoramic radiograph, a cephalometric radiograph, and a dental cone beam computed tomography (CBCT) scan are suggested when there is a need to help assess the bone quality and quantity, and supplement conventional dental radiography.
Impressions should be taken and models correctly articulated. In most situations, it is suggested that two sets of the original casts be obtained, one to be kept as a permanent record and the other to be used as part of the treatment planning. After gathering the necessary data, the information must be collated into a comprehensive treatment program.
Amsterdam and Weisgold20 has stated that although the situation truly requiring periodontal prosthesis traditionally has been one of advanced dental disease, it became apparent that with certain modifications, its philosophy, concepts, principles, and techniques could be applied to any therapeutic endeavor involving the natural dentition when implants need to be employed as well. As such, esthetically demanding implant restorations require thoughtful planning and sequencing à la periodontal prosthesis, with great respect for soft and hard tissue maturation.
Diagnostic and Surgical Templates
A diagnostic template with radiographic markers, such as the surgical template, may be fabricated to assist the surgeon and restorative dentist in analyzing the available bone to place the implants. This may be accomplished by using CBCT radiography in concert with barium sulfate-coated diagnostic templates before implant surgery.21
The surgical template, a guide to surgical implant placement, is fabricated from either a diagnostic wax-up or, preferably, a stone model of the functioning provisional restoration.
After placing the provisional restoration intraorally, impressions are made of both the prosthesis and the underlying edentulous ridges and tooth preparations. Stone models are made and an acrylic shell of the restoration is cured on a model of the remaining prepared or unprepared tooth, or both. Locations and axial alignments are carefully planned with the surgeon and are carved into the acrylic template to anticipate implant placement.
Although a lingual or palatal approach is commonly used to design the surgical guide, a facial approach also may be considered. This will provide the surgeon with an accurate visualization of the ideal implant sites, the desired path of abutment emergence, and the axis orientation in relation to the final prosthesis. The ability to perform surgical procedures demands direct access, which is provided by removal of the provisional interim restoration. The surgeon can orient the surgical template by securing it to the existing teeth, and prepare the osteotomy to properly position the implants.
Significant progress in biotechnology, radiology, and computer technology have allowed for more accurate diagnosis and treatment planning. This has resulted in construction of three-dimensional bone models, stereolithography,22 and navigational surgery to position endosseous implants with greater precision.
The Implant Restoration
Today feldspathic all-ceramic materials are being replaced by leucite-reinforced ceramics and, most recently, by the use of polycrystalline ceramics for the fabrication of tooth-supported and implant-supported restorations. These materials are densely sintered alumina (AL2O3) and partially stabilized zirconia (ZrO2), and they are utilized to fabricate implant abutments and the substrate cores for implant crowns. The alumina core may have better optical properties that provide it with some esthetic advantage. The zirconia core has twice the flexural strength, but it may be more opaque, unless reduced to 0.3 mm in the gingival one-third of the core, where the crown margin extends subgingivally.23
The survival rate and success rate of alumina abutments and zirconia abutments from clinical studies have been very high (see Figure 3.4). Adatia et al.24 demonstrated that all zirconia implant abutments tested resisted fracture until they reached forces that exceeded the incisal forces that occur in the anterior part of the mouth.24
Figure 3.4 Left: Zirconia implant abutment with internal hex and conical seal design; right: zirconia-based implant crown.
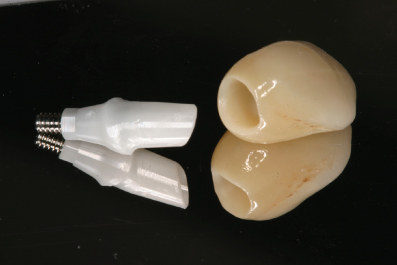
One of the key concerns for long-term maintenance of the polycrystalline all-ceramic computer-aided design/computer-aided manufacturing (CAD/CAM)-produced implant abutment and implant crown cores has been the cementation of these restorations to each other in a subgingival environment that may trap cement and create difficulty to access and remove it completely. The problem of cement retention in the soft tissues below the collar of an implant abutment can result in an inflammatory response that may jeopardize the interproximal papilla or the height of the free gingival margin facially or lingually/palatally.
These issues speak volumes to the concern for deep placement of the endosseous implant relative to the CEJs of adjacent teeth. Where possible, it may be wiser and safer to consider creating a one-piece screw-retained implant abutment with crown. The abutment crown core is then fabricated in zirconia and the crown form is veneered with feldspathic-like porcelain or leucite-reinforced porcelain and then screw-retained palatally or lingually. Newer pressable lithium disilicate monolithic material without a polycrystalline ceramic core can also be used but will require crown cementation with careful subgingival isolation.
Due to the risk of leaving cement subgingivally, implant abutment collar designs attempt to create a rise and fall to their respective gingival topography such that they are positioned only 0.5–1.5 mm subgingivally for ease of cement retrieval (see Figure 3.5).
Figure 3.5 (a) Zirconia abutment with concave neck above implant connection. The concave form theoretically provides more space for soft tissue subgingivally. (b) Zirconia abutment with gingival collar approximately 1 mm subgingivally. (c) Zirconia-based implant crown with appropriate physiological contour.

Excruciating care must be exercised to remove this cement or prevent it from penetrating deep subgingivally by isolating the tissue from the subgingival recesses of the implant abutment collar during cementation. Utilizing a retraction cord to block out this space from being infiltrated by cement is absolutely essential.
Abutment Shape
The subgingival collar height can and should support the papillae allowing for the implant crown to extend the contour through the soft tissue with a form that fills the interproximal contact areas.
Care must be taken to avoid overcontouring the subgingival abutment contour as this may flatten the height of the papillae by pressure strangulation (see Figure 3.6).
Figure 3.6 Note how the wider metal ceramic (baked to) abutments (c) are broadly contoured, squeezing the interproximal papillae and shortening the papilla heights even before implant crown placements. The narrower implant abutments (b) provide for more relaxed papillae, which can be manipulated and modified by the contours of the implant crowns.

Several individuals have developed restorative techniques whereby they modify implant transfer copings at the time of fabricating an implant-level impression. They remove the provisional abutment crown from the implant body, seat the transfer coping for a fixture-level implant impression, and immediately add acrylic or a flowable composite to the base of the transfer coping to develop the subgingival contour that has been created with the temporary restoration. This information is then transferred to a master model to be reproduced in the final restoration.
Platform Switching of Abutments
Of great significance is the concept referred to as platform switching or platform shifting. Typically, after implant insertion and loading, there is a degree of crestal bone loss by remodeling resorption.25 In the past few years, implant bodies and implant abutments have been modified in their configurations based on the concept of maintaining a biological dimension26,27 of connective tissue and epithelium above the crest of bone in an effort to lessen the often observed crestal bone loss. When the horizontal relationship of the outer perimeter of the implant and a smaller diameter implant abutment is mated together, there appears to be a reduction in the loss of crestal bone circumscribing the head of the implant body.
As a result, and following the success of earlier implant systems, most of the major implant manufacturers have reengineered their respective implant systems to create internal abutment connections, with internal conical interfaces and antirotational features, and with implant abutments that are narrower in width than the diameter of the implant head, such that they create a horizontal platform for the overlaying connective tissue and epithelium with less potential compromise to the underlying interfacial bone-to-implant relationship.
Tarnow et al.28 assessed the height above the bone crest of the interimplant papilla. The multicenter study probed 136 anterior and posterior sites transmucosally in individuals who had implant-supported prostheses for a minimum of 2 months. The mean implant papilla height was 3.4 mm, with the vast majority of measurements between 2 and 4 mm.
Gastaldo et al.29 sounded the bone crest and measured to the base of the contact point between implant crowns. Complete soft tissue fill occurred only when the di/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


