Implants for the maxillary edentulous patient
![]() Additional illustrations can be found on the companion website at www.blockdentalimplantsurgery.com
Additional illustrations can be found on the companion website at www.blockdentalimplantsurgery.com
Preoperative planning and assessment
1. General health of the patient
Debilitated patients often have soft bone and do not heal as well as healthy patients. Patients with diabetes with sugar levels above 120 mg/dL may not form bone on implants as well as those in better control.1–5 Female patients older than age 50 years and older men may have low bone density, which must be taken into consideration and evaluated preoperatively by examining the bone density in the jaw.
2. Goals of the patient, such as the need for removal of the palatal portion of the prosthesis, increased stability when chewing, and desire for a fixed prosthesis
Ask the patient to complete this sentence: “At the end of my treatment I want. . . ” The answer will direct the clinician to the treatment. The patient may desire a functional set of teeth that she does not remove. She may desire her maxillary denture to be stable while chewing. She might want to look and function as if she had her original teeth in her original nondiseased status. The goals of the patient are critical to understand to guide treatment planning.
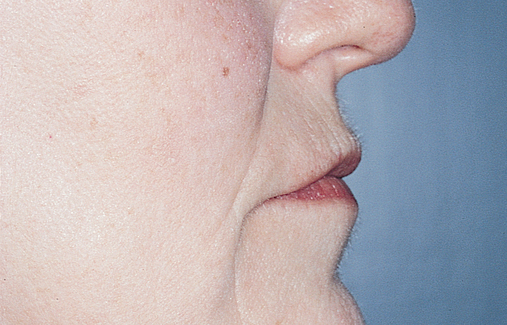
3. Esthetic requirements to restore the soft tissue profile of the patient
Patients need to show teeth at rest commensurate with their age. Whereas younger patients show 2 to 3 mm of central incisor at rest, 80-year-old patients may not show their central incisors at rest. Most have their smile lines at the level of the gingival margin of a normal length central incisor (10.5–11.0 mm). The use of pink material to restore gingival horizontal and vertical deficiency, whether porcelain or acrylic, needs to be considered. Most patients have adequate support of their nasal labial profile with appropriate set teeth, but a few may require additional support from their prosthetics.
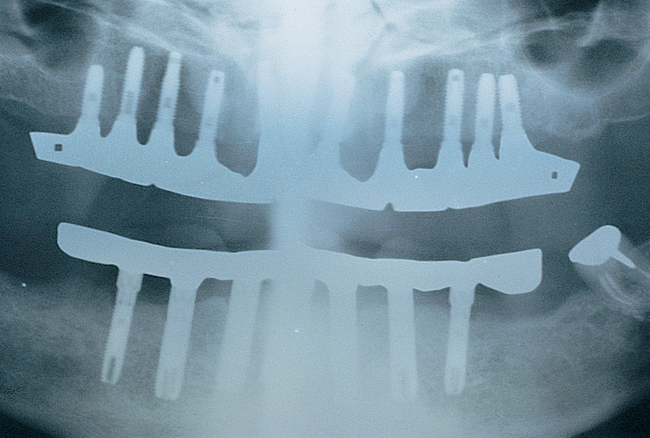
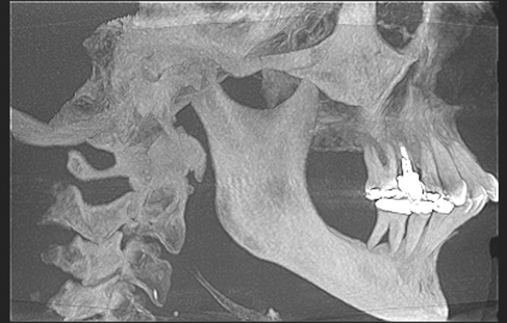
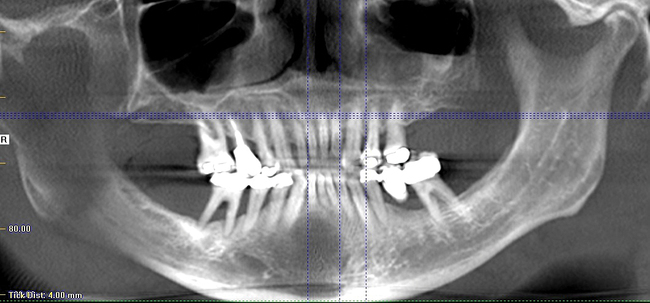
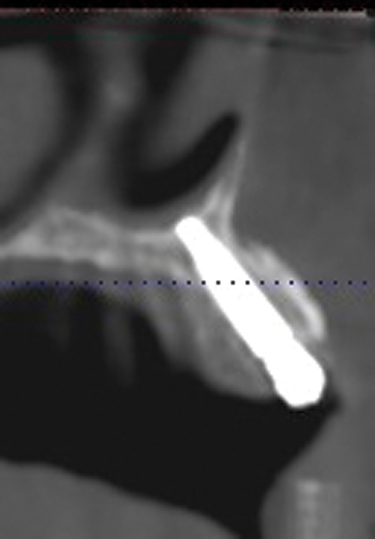
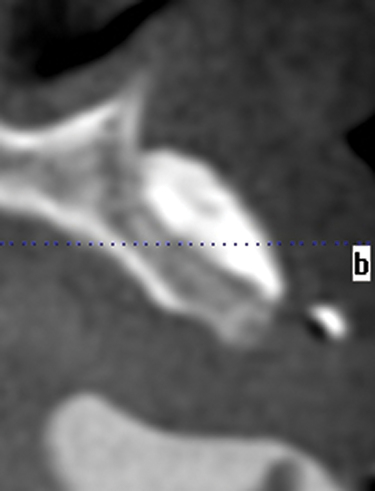
4. Availability of bone in the anterior and posterior maxilla
Implants must be placed into bone. Implant-supported restorations require bone in specific regions depending on the prosthetic plan. The surgeon needs to consider bone height and width and provide the team with a strategy to provide the patient with the ultimate restoration that achieves his or her goals. Cone-beam scans are critical to evaluate bone quantity and quality.
As milling methods improve, many removable, fixed removable, and fixed milled restorations have similar costs. Hybrid type prostheses are slightly more expensive than milled bar and clip prostheses. Crown and bridge prosthetics with ceramics are more expensive than hybrid restorations. In general, all options should be presented to the patient who then can decide which treatment to seek. Laboratory fees do vary from laboratory to laboratory, but the time to fabrication of the prostheses also varies. This variation from the laboratory phase and time in the chair accounts for diversity in the prosthetic fee schedule. The surgical fee depends on the number of implants placed and less on the actual prosthesis.
6. Consent for bone grafting of deficient sites, including consideration of the morbidity of the harvest site
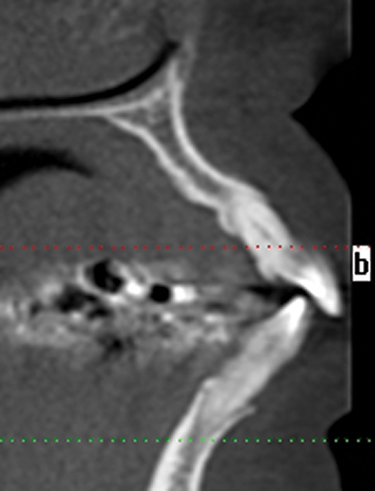
1. Condylar morphology to rule out erosion and vertical dimension problems
2. The mandibular plane angle can be appreciated, indicating the patient’s vertical dimension and presence of overclosure of the mandible because loss of posterior occlusion or loss of bone.
3. The skeletal position of the maxillary ridges in regards to the mandibular ridge or teeth
4. The status of the sinuses, including ethmoid, frontal, sphenoid, and maxillary. The presence of intrasinus polyps, congestion, or other pathology can be easily identified and treatment planned accordingly.
5. The thickness of the alveolar bone in all areas of the maxilla. In addition to thickness, the presence of bone on the piriform rim can be discerned. The quality of the bone can be determined.
6. The location of the incisive canal is easily seen.
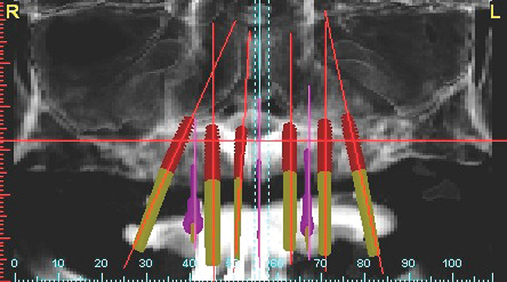
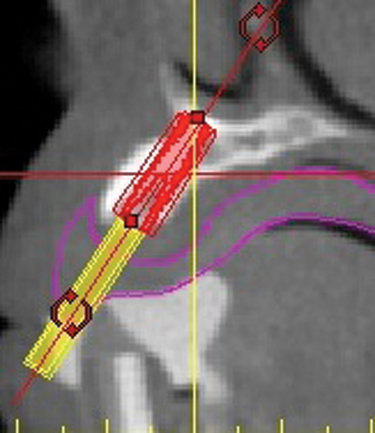
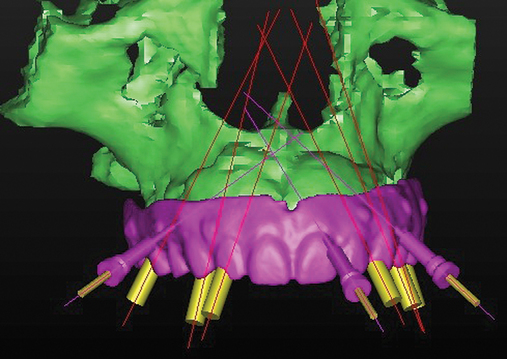
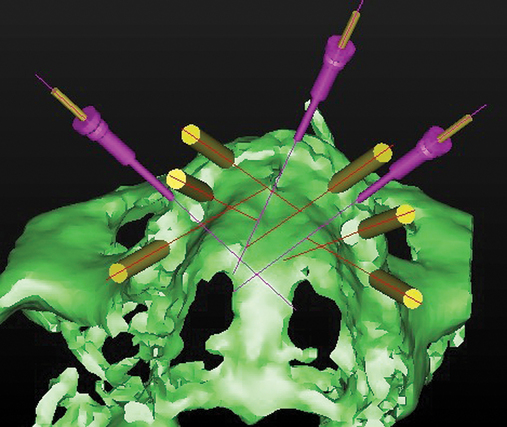
7. By combining the cone-beam scan with computed tomography (CT) planning software, the need for bone reduction can be determined and a model made if necessary. The specific implant diameter and lengths can be determined. The type of abutments can be determined. CT surgical guide stents can be fabricated, as well as a milled acrylic prosthesis of the provisional prosthesis for simple prosthesis conversion.
1. Greater than 10 mm of vertical bone height in the anterior and posterior maxillae
2. Greater than 10 mm of vertical bone height in the anterior maxilla but less than 10 mm of bone height in the posterior maxilla
3. Less than 10 mm of vertical bone height in the anterior maxilla, with greater than 10 mm of vertical bone height in the posterior maxilla
4. Less than 10 mm of vertical bone height in the anterior and posterior maxillae
A prosthetic plan is completed, with the aid of the restorative dentist, after the amount of bone has been determined. Parel’s classification of the edentulous maxilla is useful for conceptualizing the prosthetic plan (Box 3-1).
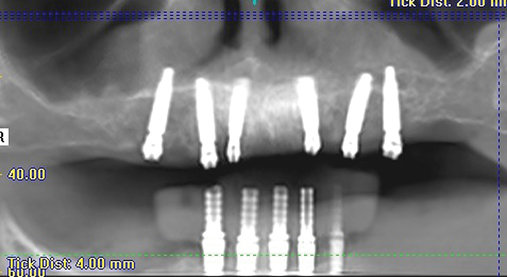
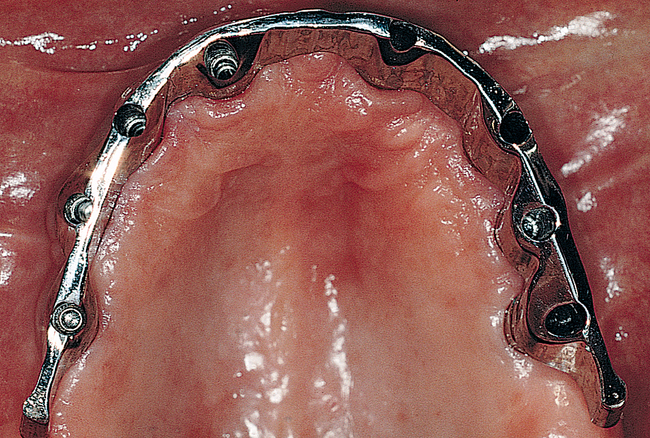
For the class 2 maxilla, a fixed crown and bridge prosthesis, a fixed-removable (e.g., spark erosion or milled) prosthesis, or a type of removable overdenture prosthesis may be prescribed. The fixed implant-borne and fixed-removable prostheses require at least six to eight endosseous implants to support a maxillary implant-borne prosthesis. Cross-arch stabilization is recommended, especially if the opposing occlusion includes natural teeth or has limited mandibular posterior teeth. Zygomatic implants are the exception (see Chapter 5). These traditional fixed or fixed-removable prostheses require posterior maxillary vertical bone height for implants placed in the first molar region, or the patient should have adequate bone to angle the most posterior implant to provide the abutment at the first molar location. Cantilevers are not recommended in the maxilla. The removable tissue-borne prosthesis requires four implants placed into the anterior maxilla to support a bar, which has retentive vertical stress-breaking attachments. Edentulous maxillary prostheses usually are fabricated with cross-arch stabilization of the left and right implants. Using four individual implants with studlike attachments is financially less expensive, but long-term clinical data are not available for evidence-based support for this treatment plan.
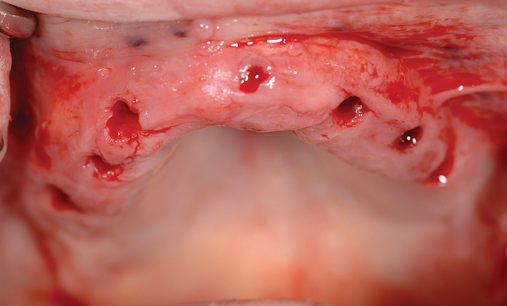
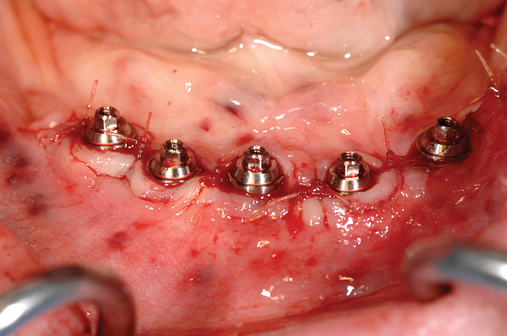
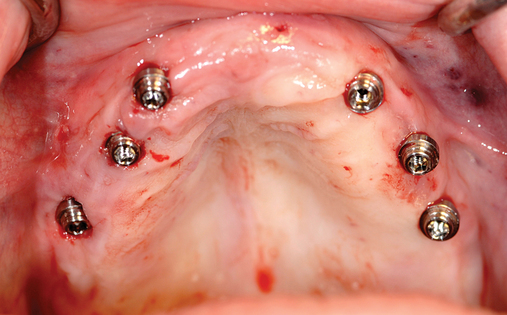
Placement of four implants into the anterior maxilla
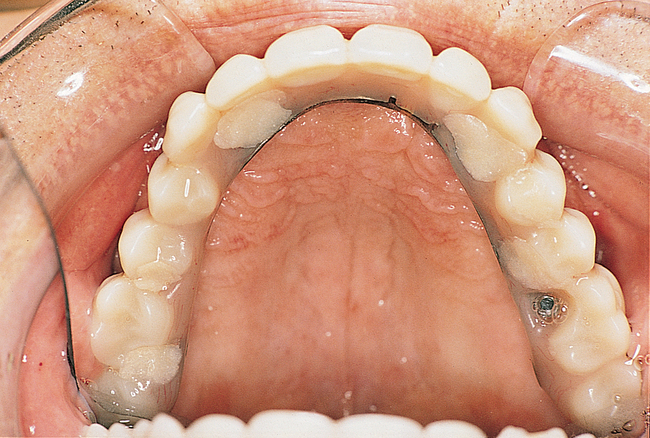
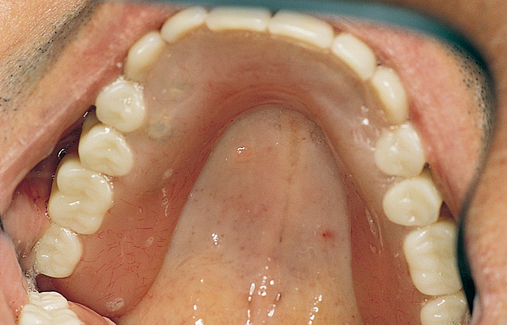
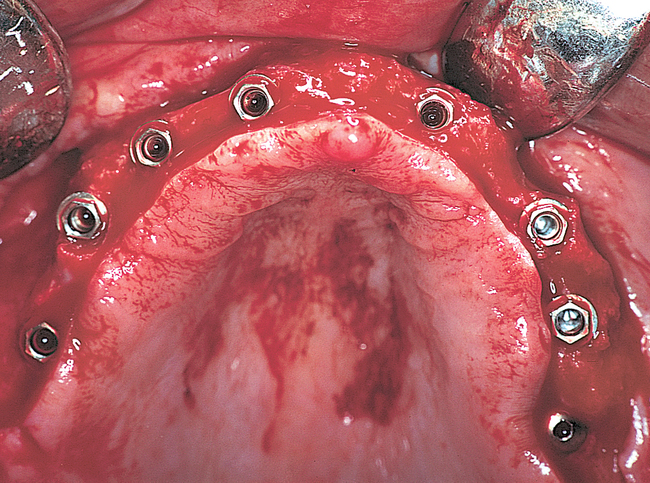
For a patient with adequate anterior vertical bone height and a treatment plan for anterior implants to provide overdenture support, four implants can be placed. Placement of at least four implants is recommended for an implant-supported overdenture in the maxilla because fewer than four maxillary implants will not predictably resist the forces6 placed on them (Figure 3-1). Two implants are contraindicated to retain a maxillary overdenture.
At surgery, the surgeon should understand the prosthetic plan and recognize the ideal locations of the implants. Often these implants can be placed slightly palatal to the crest to engage more of the palatal bone, providing a thicker width of labial bone (see Figure 3-1). A local anesthetic is infiltrated into the labial and palatal regions of the anterior maxilla. Incisions for implants placed into the anterior maxilla usually are placed over or slightly palatal to the crest. Vestibular incisions are avoided in the anterior maxilla because they can shorten the vestibule and increase the patient’s postoperative discomfort.

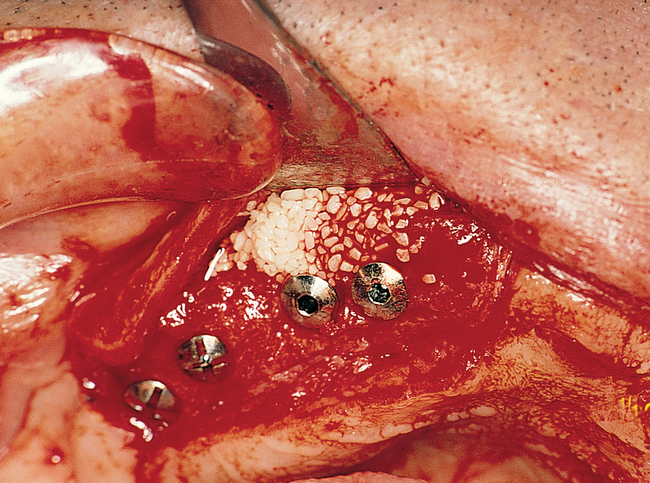
Subsequent graduating-sized drills initiate and expand the implant site until the final drills are used. If the ridge is excessively narrow, the ridge may require grafting before implant placement. Usually the ridge has sufficient width for placement of the implants. If the ridge is thin and does not expand as the bone is examined superiorly, the use of osteotomes or ridge splitting in a ridge less than 3 mm is not predictable. For these cases, onlay grafting is indicated and should be discussed with the patient. (See Chapter 4 for examples of onlay grafting of the anterior maxilla.)
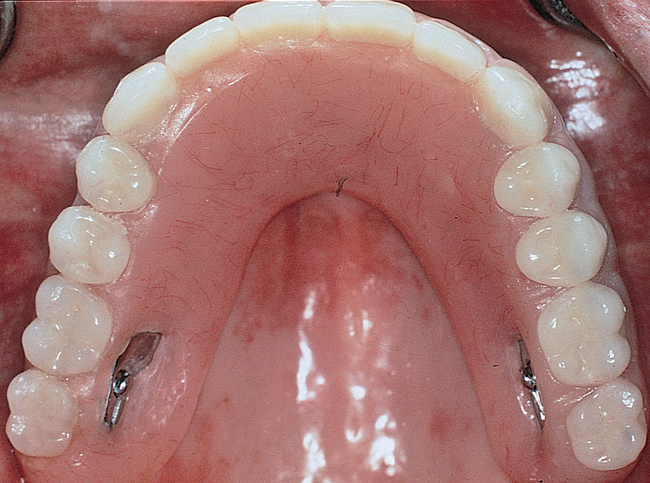
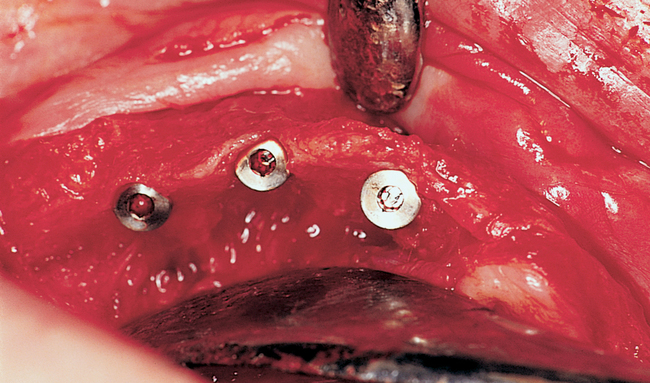
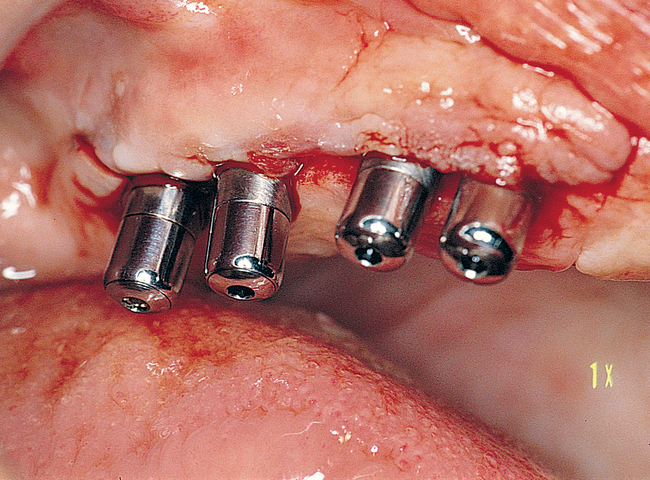
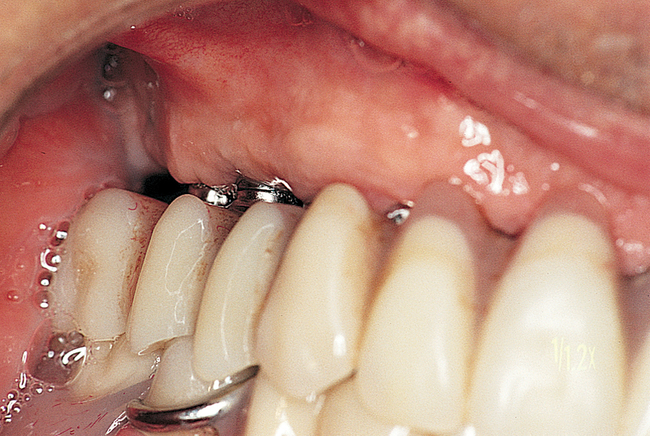
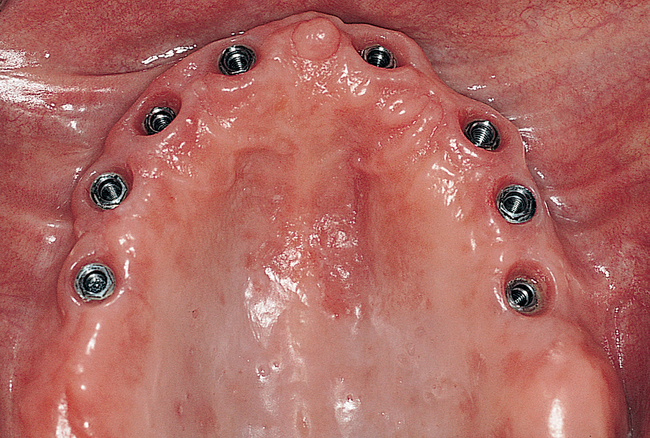
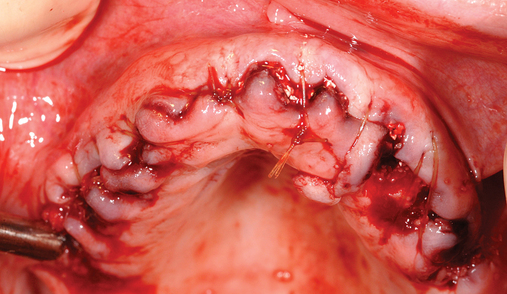
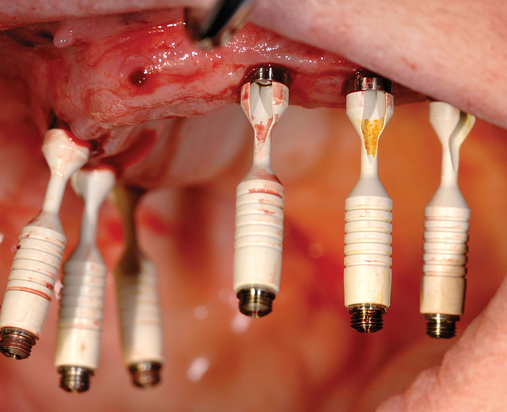
Exposure of implants in the edentulous maxilla
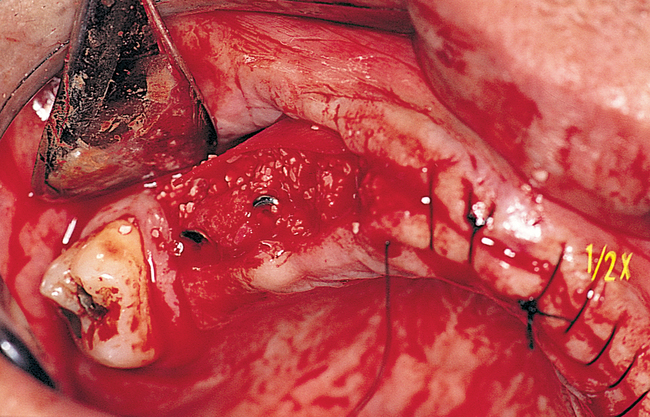
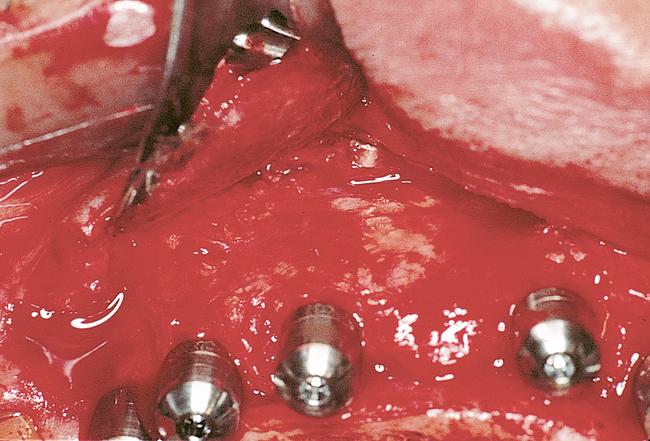
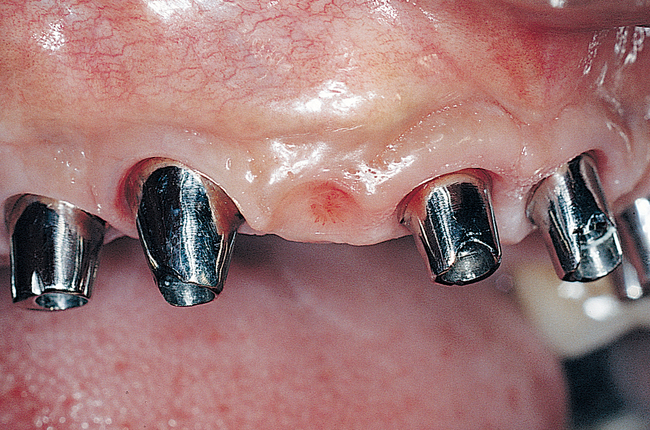
After an appropriate amount of time has been allowed for implant healing, the patient returns for exposure of the implants and placement of temporary healing abutments (Figure 3-2). After administration of a local anesthetic, an incision is made bisecting the keratinized gingiva (KG) to transpose it labial to the implant abutments. The mucosal flap is reflected full thickness, including periosteum, to allow direct visualization of the implant. The cover screws are removed, the top of the implant is gently cleansed of soft tissue, the inside of the implant is irrigated with sterile solution, and the temporary healing abutment is placed. The gingival flap may be excessively thick and may need to be thinned. The inside thickness of tissue is removed with a scalpel to thin the flap, which is reduced as necessary. The incision is closed around the healing abutments. The denture is relieved and relined to stent the mucosa to the alveolus (see Figure 3-2).
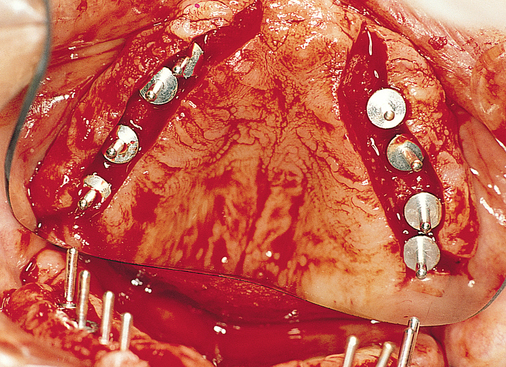
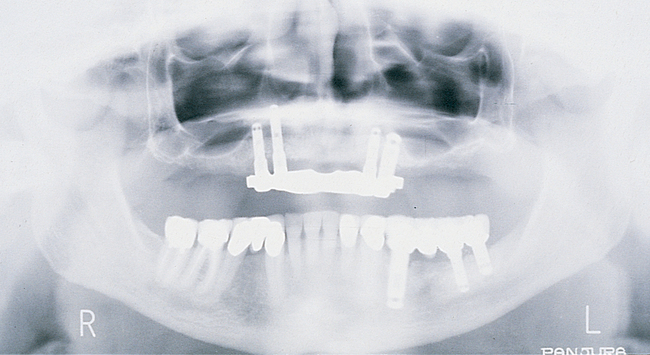
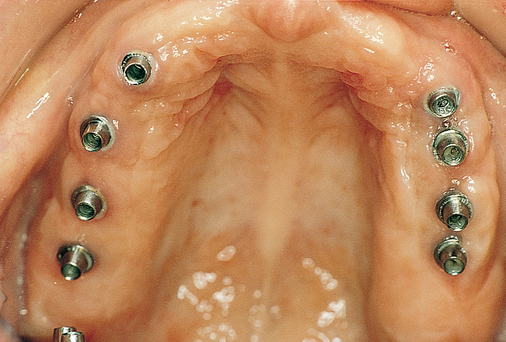
Placement of anterior and posterior implants without a graft
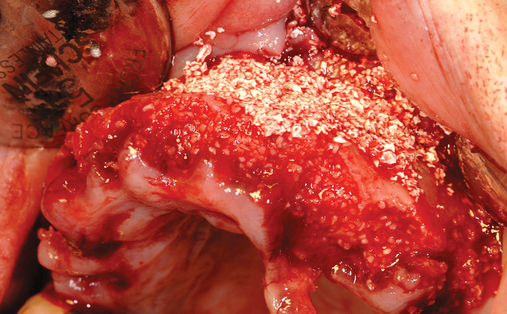
An edentulous patient with a class I maxilla requires only the placement of implants to replace the missing teeth (Figure 3-3). In most patients with a class I maxilla, who have lost their teeth with minimal bone loss, the labial bone has an irregular contour. These patients may benefit from augmentation of the labial bone to smooth the bone contour and enhance the final restoration, especially for those with high smile lines.

Patients with a class II maxilla, who have lost their teeth but have a moderate amount of bone, must have an esthetic evaluation as described previously. Determination of lip support is important. These patients should be advised that pink restorative material may be necessary for soft tissue support. These patients may require a labial flange of a removable prosthesis to provide nasolabial support. Conversely, they may need material added to a fixed restoration to provide an esthetic facial appearance. Either way, this needs to be determined before implant placement. Maxillary hybrid type prostheses rarely require additional flange support because of the bulk on the labial portion of the fixed prosthesis. With the use of maxillary hybrid prostheses and better pink restorative materials, more fixed options are available, resulting in less use of fixed removable prostheses. The cost of these fixed prostheses is always important to consider but is not preventive for many patients (Figure 3-4).




Patients with a class III maxilla, who have lost their teeth and most of the alveolar bone to the basal level, can benefit from a fixed or a fixed-removable restoration, depending on bone height and availability (see Figure 3-4). If implants are angled, then their length increases, increasing the mechanical stability, and hence more fixed options become available. The use of angled abutments restores parallelism for the restorative phase.




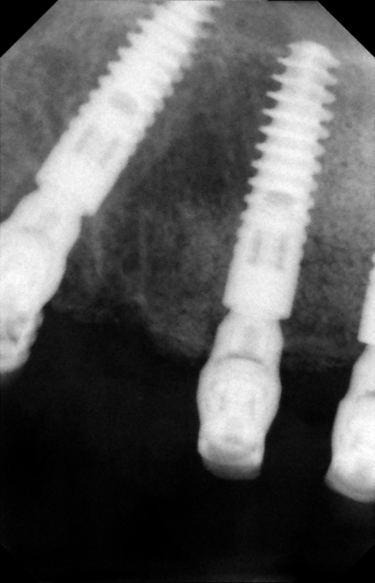
When there is sufficient bone anterior and posteriorly, a fixed restoration can be planned. There are generally two options for implant placement. One option is placement of implants in the molar and premolar locations bilaterally for right and left three-unit fixed bridges. Additional implants are placed in the canine and central incisor locations bilaterally for a six-unit, four-implant retained prosthesis. This plan does not provide cross-arch stabilization, which may also result in adverse mechanical stresses.6
A second option is to place implants from canine posteriorly in the canine, premolar, and molar sites for four implants for each side, leaving the anterior maxilla void of implants. A full arch single unit restoration is fabricated. This provides the patient with a cross-arch stabilized restoration, which has been shown to be stable long term. Lateral forces from occlusion are absorbed by the full arch framework with less tension and compression felt on the implant as described in the Skalak model.6 If three units are made for a full arch restoration, lateral forces may not be absorbed as efficiently. If necessary, the full arch restoration can be screw retained for maintenance or cemented with temporary cement for removal.
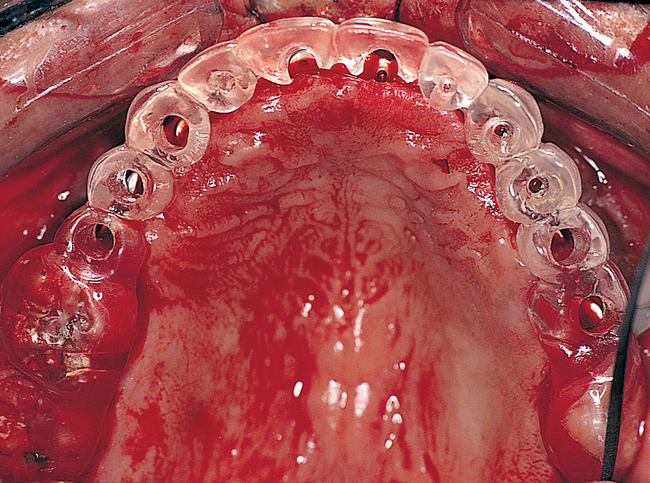
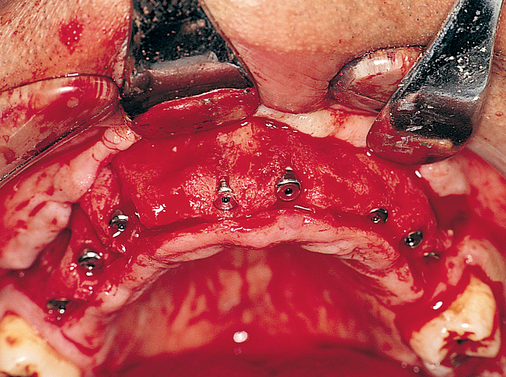
Incisions for full-arch distribution of implants placed into the maxilla usually are placed slightly palatal or over the crest. Vertical release incisions are made posterior to the most distal implant, which typically is in the first or second molar region. Anterior, midline, vertical release incisions usually are not necessary. Midline releasing incisions cause increased postoperative discomfort. Planning for incision breakdown is recommended; thus, placing the incisions on the crest ensures that the KG will be labial to the implants. A vestibular incision or an incision made at the junction of the attached and unattached gingivae may result in loose gingiva adjacent to the implants if incision breakdown occurs (Figure 3-5).


Full arch rehabilitation in patients with systemic disease that adversely affects their teeth
Michael S. Block and Celeste Block
Cyclic neutropenia is a rare hematologic disorder that is an inherited or acquired autosomal dominant disorder of the gene for protease neutrophil elastase (ELA-2 or ELANE). Neutrophil elastase normally synthesizes neutrophil precursors during primary granule formation.7 When a missense or deletion mutation occurs, apoptosis of neutrophil elastase precursors is accelerated and spontaneous, resulting in a reduced neutrophil production and the cyclic nature of this disorder.8 This apoptosis might be mediated by an abnormal proapoptotic factor called Bcl-2. 9,10 It is thought that mutated ELA-2 leads to impaired production and survival of bone marrow–derived myeloid-committed progenitor cells and an increased proliferation of primitive CD34+ progenitor cells.8,11–13
Clinical characteristics in the child and young adult are recurrent fever and skin and throat inflammation including ulcers, gingivitis, respiratory infections, and sinusitis. Between neutropenic intervals, the patient is usually healthy.8,14,15
A normal absolute neutrophil count (ANC) is above 1500 cells per microliter (1.5 K/µL). An ANC less than 0.5 K/µL is defined as neutropenia and significantly increases the risk of infection. Neutropenia is the condition of a low ANC, and the most common condition in which an ANC would be measured is in the setting of chemotherapy for cancer.16
The cycles of cyclic neutropenia occur every 21 days and last for 3 to 5 days during which the circulating neutrophil count decreases to about 0.2 K/µLat the nadir of the cycle.10 As the neutrophil count decreases, the monocyte and eosinophil levels increase.11 When the neutrophil count is extremely low, life-threatening infections commonly occur. Cyclic neutropenia can occur at any age, but a large percentage occurs during childhood. Neutrophil levels continue to cycle, but symptoms decrease in severity after the second decade of life.11
Within the first 5 years of implant placement, both periodontal patients and nonperiodontal patients share similar results. After 5 years, more significant differences arise among periodontal patients such as greater marginal bone loss because of maintenance issues. Patients with a history of periodontitis must be kept on a strict hygiene recall as well as educated on proper oral hygiene to maintain healthy tissues needed for implant therapy.17,18 Smaller studies imply that there is a difference but not at a statistically significant level.19–21 Treating periodontally compromised patients before and after implant placement helps the success of implant therapy, as reported in a 10-year follow-up study. Putting patients on a regular recall schedule contributed to more successful outcomes. This study showed greater bone loss around an implant in a periodontally compromised patient compared with a periodontally healthy patient.19
In a study of 10 patients with a history of periodontitis, immediate implant placement into an extraction site showed successful osseointegration. These authors believed that success was due to a decrease in treatment time and a flapless surgery. By doing a flapless surgery, the blood supply was not altered. They also used periodontal therapy to reduce the microbial load to prevent inflammation.22
The microbial flora present subgingivally before extractions and after implant placement was reduced for both aerobes and anaerobes. There was a slight increase in anaerobes present around the implant site. The specific flora around the implant that was reduced over time includes but is not limited to Tannerella forsythia and Prevotella intermedia. However, there was not a notable change in Aggregatibacter actinomycetemcomitans around the implant site.23
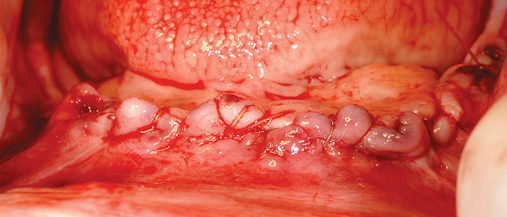
This 59-year-old woman presented with several complaints, including flaring of her teeth, mobility of her teeth, chronic dental pain, and the inability to chew a normally textured diet. She was also concerned about her facial appearance (Figure 3-6).









A cone-beam scan (ICAT, Image Sciences International) was taken as well as diagnostic models.
Her facial examination showed:
2. Flaring of her maxillary and mandibular dentition
3. Loss of papilla between her teeth
4. Slightly deficient lower facial height
1. Flaring and malposition of her teeth.
2. Severe bone loss of her teeth in the mandible and maxilla.
Treatment plan
Phase 1
1. Because of the extreme proclination of the maxillary incisors, her current incisor position needed to be corrected. The buccal-lingual position of the central incisor was established based on the anatomical average distance from the distal border of the incisive papilla to the outer labial surface of maxillary incisor. The average reported distance is 12.5 mm with a standard deviation of 3.8 mm.24 In this case, the position of her current central incisor distance was 16 mm. The teeth on the immediate denture were set to bring the incisal edge position 4 mm lingual to her current position.
2. The vertical position of the central incisor was established based on the anatomical average distance measured from the base of the sulcus to the incisive edge of the maxillary incisor. The reported average vertical distance is 22 mm. This distance was used to provide a reference for the placement of the central incisor tooth vertical position.24
Her current occlusal plane was kept the same as pre-extraction with rotation of the mandible to close her vertical dimension 3 mm. Her incisal edge position was based on average dimensions as describe above.
3. A practical method used to establish the buccal-lingual angulation of the maxillary central incisor was by recording the angle made between the central incisor’s incisal third and the maxillary posterior occlusal plane. When the angle is acute like in this patient, the incisal third is overcontoured or protruded and should be restored back to its normal 90-degree position. This was used as part of the setup to maintain an appropriate esthetic analysis.25
Computed tomography–guided surgery in the edentulous maxilla
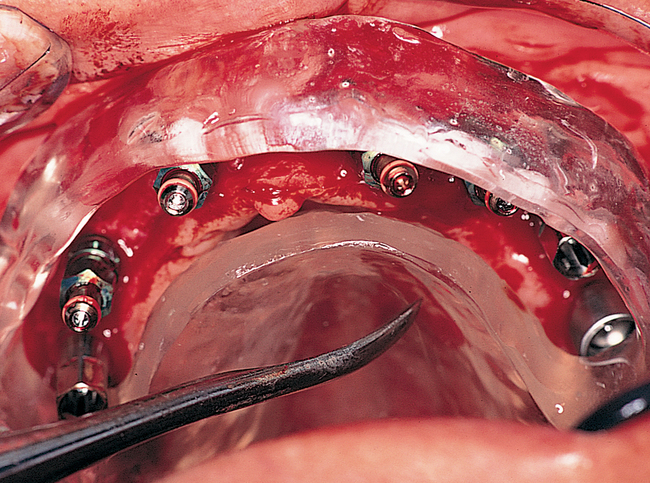
1. Implants can be placed in the ideal position based on preoperative planning. The implants are placed on the computer to the ideal locations as determined by fabrication of a radiographic duplicate of the planned restoration. The initial procedure performed by the restorative dentist determines the exact location of the teeth. This often requires fabrication of a new denture. The new denture, with its approved form, function, and esthetics, is duplicated for scanning. The duplicated denture is used to direct implant placement, with the type of final prosthesis taken into consideration. For example, if the final prosthesis is to be a fixed crown and bridge, the implants must be placed so as to avoid embrasures and 3 mm apical to the planned gingival margin position on the final prosthesis. If the final prosthesis is to be the fixed-removable type with a bar, the implants must be placed with sufficient space for fabrication of the bar and prosthesis, which includes a metallic intaglio surface that interdigitates with the milled bar. If the planned prosthesis is a hybrid denture, the implants must be placed with consideration given to the space necessary for cleaning the fixed prosthesis, which can be removed by the dentist but not by the patient.
2. Implants can be placed without the creation of flaps. If tissue need not be raised to allow direct visualization of the bone and its adjacent structures, the patient has less swelling, bruising, and pain. If bone is not reflected, the result is believed to be less disruption of the blood supply to the bone and thus less crestal bone resorption.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses