Temporomandibular Joint
• To diagram and label a sagittal section of the temporomandibular joint (TMJ)
• To define the role of a synovial cavity
• To describe the two movements of the TMJ as the mouth opens and know where these movements take place
• To describe the role of the superior posterior elastic lamina, the inferior posterior collagenous lamina, and the superior and inferior heads of the lateral pterygoid muscle as the jaw goes through its various functional movements
• To define disc derangement, subluxation, bruxism, and TMJ sounds
STRUCTURE
As the name indicates, the temporomandibular joint (TMJ) is the articulation between the temporal bone and the mandible. A joint is a joining together of two bones, and there are a number of joint types. A suture of the skull is one type of joint that we have already studied (see Chapter 26), and the TMJ is another type because it is a joint in which the surface of one bone moves over the surface of another.
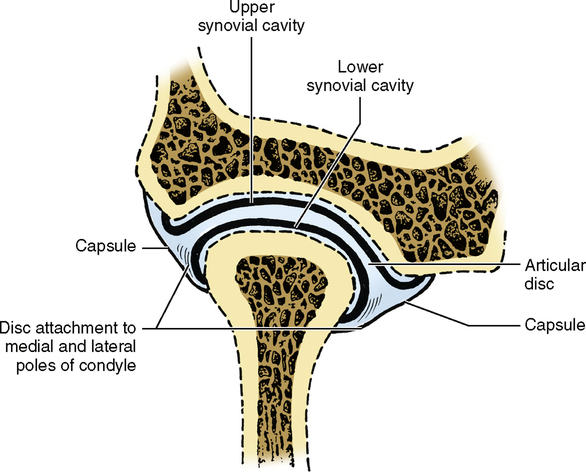
Actually, the TMJ is two joints that move and function as one. It is also a bilateral or two-sided joint in that the mandible is fused at the midline so that the left and right joints are interrelated in their movements. In Chapter 26, you learned the osteology or the system of bony parts of the TMJ. Fig. 29-1 shows the mandibular fossa, posterior tubercle, and articular eminence of the temporal bone, as well as the condyle of the mandible. Between these two bones you can see a small fibrous pad of dense collagen tissue called the articular disc. The upper surface of the disc is concavoconvex to match the contours of the mandibular fossa and articular eminence, whereas the lower surface of the disc is concave to match the contour of the condyle. Fig. 29-1 shows that the articular disc is thickest at its posterior end, it is thinnest at its middle, and there is a slight increase in thickness at its anterior end. The thick posterior area is called the posterior band, the thin middle area is called the intermediate zone, and the slightly thicker anterior area is called the anterior band. Above and below this disc are small saclike compartments called synovial cavities. Part of the tissue lining these cavities is an epithelium that secretes a few drops of lubricating liquid called synovial fluid, which allows the surfaces to rub over one another without irritation.
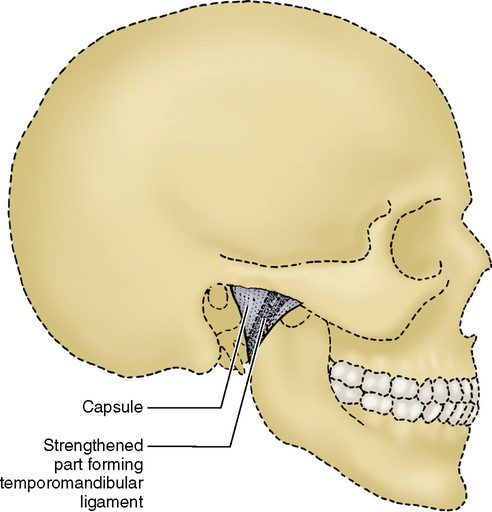
The entire TMJ is surrounded by a thick fibrous capsule. The lateral side of this capsule is thickened between the articular tubercle and the lateral pole of the condyle. This thickened area is the temporomandibular ligament. This ligament prevents the condyle from being displaced too far inferiorly and posteriorly and provides some resistance to lateral displacement (Fig. 29-2). On the medial side are two other ligaments that help to control the movement of the TMJ. They are the stylomandibular ligament and the sphenomandibular ligament.
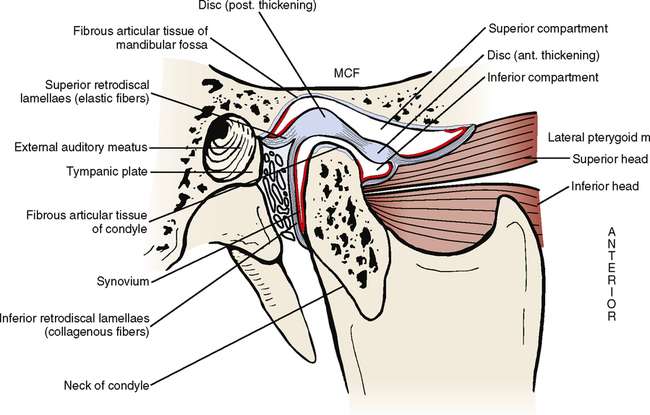
The articular disc is attached both medially and laterally to the poles of the condyle (Fig. 29-3). Anteriorly it is attached to some fibers of the superior head of the lateral pterygoid muscle. These fibers penetrate the capsule and insert into the disc. The area posterior to the disc is the retrodiscal pad. This is an area composed of relatively loose connective tissue in which much of the blood and nerve supply to the joint is located. The blood supply comes from the ascending pharyngeal, superficial temporal, deep auricular, and anterior tympanic arteries. All these arteries are branches directly or indirectly off of the external carotid artery. The nerve supply to the joint comes from the following three branches of the third division of the trigeminal nerve: auriculotemporal, deep temporal, and masseteric nerves. Running from the upper posterior part of the disc is an elastic lamina or tissue layer that lies above the retrodiscal pad. Posteriorly it attaches to the tympanic plate of the temporal bone. Running from the lower posterior border of the disc is a collagenous lamina that lies below the retrodiscal pad and attaches to the posterior neck of the condyle, where the capsule attaches to it (see Fig. 29-1).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses