Salivary Gland Diseases
Byron W. Benson
Salivary Gland Disease
Disease Mechanism
Dental diagnosticians have professional responsibility for detecting disorders of the salivary glands. A familiarity with salivary gland disorders and applicable current imaging technology is an essential element of the clinician’s armamentarium. Both major and minor salivary glands may be involved pathologically; however, this chapter deals only with the major glands. Salivary gland disease processes may be divided into the following clinical categories: inflammatory disorders, noninflammatory disorders, and space-occupying masses. Inflammatory disorders are acute or chronic and may be secondary to ductal obstruction by sialoliths, trauma, infection, or space-occupying lesions such as neoplasia. Noninflammatory disorders are metabolic and secretory abnormalities associated with diseases of nearly all the endocrine glands, malnutrition, and neurologic disorders. Space-occupying masses are cystic or neoplastic; the neoplasms are benign or malignant.
Clinical Signs and Symptoms
Diseases of the major salivary glands may have single or multiple clinical features. Swelling in the areas of the parotid and submandibular glands should create a clinical suspicion of salivary gland disease until ruled out. Pain and altered salivary flow may be present. Because the periodicity and longevity of these symptoms are important in the differential diagnosis, a review of the medical history and physical condition of the patient may provide important information. A history of skin, endocrine, or swallowing abnormalities may suggest a systemic collagen disease or metabolic disorder.
Differential Diagnosis of Salivary Enlargements
Enlargements of the Parotid Area
Unilateral enlargements of the parotid area are categorized by the presence of a discrete, palpable mass or a diffuse swelling. If no mass is apparent, sialadenitis should be considered. Sialadenitis may be primary or secondary to ductal obstruction (retrograde). A mass superficial to the gland may represent lymphadenitis, infected preauricular cyst, infected sebaceous cyst, benign lymphoid hyperplasia, or extraparotid tumor. A mass intrinsic to the gland suggests a neoplasm (benign or malignant), intraglandular lymph node, or hamartoma. Rapid growth, facial nerve paralysis, rock-hard texture, pain, and older age of occurrence are clinical features of malignant neoplasms.
The differential diagnosis of asymptomatic bilateral enlargements of the parotid area may include benign lymphoepithelial lesion, Sjögren’s syndrome, alcoholism, medication (iodine and certain heavy metals), and Warthin’s tumor. Painful bilateral enlargement may occur after radiation treatment or as a result of bacterial or viral sialadenitis (including mumps) when accompanied by systemic symptoms.
The differential diagnosis of diffuse facial swelling in the parotid region, not related to abnormalities of the gland, includes hypertrophy of the masseter muscle, accessory parotid gland, lesions related to the temporomandibular joint, and osteomyelitis of the ramus of the mandible. A palpable mass superficial to the gland suggests lymphadenitis, an infected preauricular or sebaceous cyst, benign lymphoid hyperplasia, or extraparotid tumor (Box 29-1).
Enlargements of the Submandibular Area
Unilateral enlargement of the submandibular area associated with tender lymph nodes is suggestive of sialadenitis, which may be primary or secondary to ductal obstruction or decreased salivary flow (retrograde). Unilateral enlargement without tender lymph nodes suggests a neoplasm, cyst, lymphoepithelial lesion, or fibrosis. An intraglandular mass may be neoplastic or cystic. Neoplasms of the submandibular gland have a greater chance of being malignant than neoplasms of the parotid gland. Sublingual gland neoplasms have a still greater chance of being malignant than neoplasms of the submandibular glands. Rapid growth, rock-hard texture, pain, and older age of occurrence are clinically suggestive of malignancy. Masses superficial or adjacent to the submandibular gland may be lymph nodes or extraglandular neoplasms.
Bilateral enlargement of the submandibular gland area suggests bacterial or viral sialadenitis. Although mumps is primarily a viral infection of the parotid glands, it may also occur in the submandibular glands. Other causes of swelling in the submandibular region include Sjögren’s syndrome, enlarged lymph nodes, submandibular space infection, and branchial cleft cyst (see Box 29-1).
Applied Diagnostic Imaging
Diagnostic imaging of salivary gland disease may be undertaken to differentiate inflammatory processes from neoplastic disease, distinguish diffuse disease from focal suppurative disease, identify and localize sialoliths, and demonstrate ductal morphology. In addition, diagnostic imaging attempts to determine the anatomic location of a tumor, differentiate benign from malignant disease, demonstrate the relationship between a mass and adjacent anatomic structures, and aid in the selection of biopsy sites.
Strategies for Diagnostic Imaging
Projection (plain film) radiographs are two-dimensional images acquired without special effects. They are an appropriate starting point for imaging the major salivary glands from a cost-benefit point of view. These images can demonstrate moderately calcified sialoliths and the possible involvement of adjacent osseous structures. Because obstructive and associated inflammatory conditions are the most common disorders and primarily involve the ductal system, conventional sialography is typically the most appropriate next imaging modality. If the patient is allergic to the iodine contrast agent used in sialography, magnetic resonance imaging (MRI), multidetector computed tomographic (MDCT) imaging, or ultrasonography (US) may be selected as alternative imaging modalities. More recent studies comparing the diagnostic yield of MRI with sialography suggest that MRI might replace sialography in the future as the imaging modality of choice for ductal pathosis. Sialography, cone-beam computed tomographic (CBCT) imaging, and MDCT imaging are the best imaging modalities for the detection of sialoliths (sialolithiasis) if they are calcified enough to be radiopaque. If sialography eliminates inflammatory disorders or suggests the presence of a space-occupying mass (either cystic or solid), contrast-enhanced MDCT imaging or MRI is appropriate for evaluation. US is an alternative technique to differentiate cystic lesions from solid masses and to identify advanced autoimmune lesions. Functional disorders such as xerostomia are appropriately imaged with sialography or scintigraphy (nuclear medicine scan). Scintigraphy can provide important physiologic information that may be helpful in forming the differential diagnosis.
Projection Radiography
Projection or plain radiography is a fundamental part of the examination of the salivary glands and may provide sufficient information to preclude the use of more sophisticated and expensive imaging techniques. Both intraoral and extraoral techniques are appropriate, depending on the patient’s clinical presentation and history. These images have the potential to identify unrelated pathoses in the areas of the salivary glands that may be mistakenly identified as salivary gland disease, such as resorptive or osteoblastic changes in adjacent bone causing periauricular swelling mimicking a parotid tumor. Panoramic and posteroanterior skull radiographs may demonstrate bony lesions, eliminating salivary pathosis from the differential diagnosis. Unilateral or bilateral functional or congenital hypertrophy of the masseter muscle may clinically mimic a salivary tumor. An extraoral image may demonstrate a deep antegonial notch, overdeveloped mandibular angle, and exostosis on the outer surface of the angle in cases of masseter hypertrophy.
Projection images are useful when the clinical impression, supported by a compatible history, suggests the presence of sialoliths (stones or calculi). The examination should include both intraoral and extraoral images to demonstrate the entire region of the gland. Sialoliths may be multiple at different locations. It is expedient to decrease the usual exposure by about half to avoid overexposure of the sialoliths. However, this technique is limited by the fact that 20% of the sialoliths of the submandibular gland and 40% of the sialoliths of the parotid gland are not well calcified, rendering them radiolucent and not visible on projection images. When acquired digitally, the images can be enhanced to assist in visualizing anatomic structures and pathologic abnormalities. Radiolucent sialoliths are rarely found in the sublingual glands.
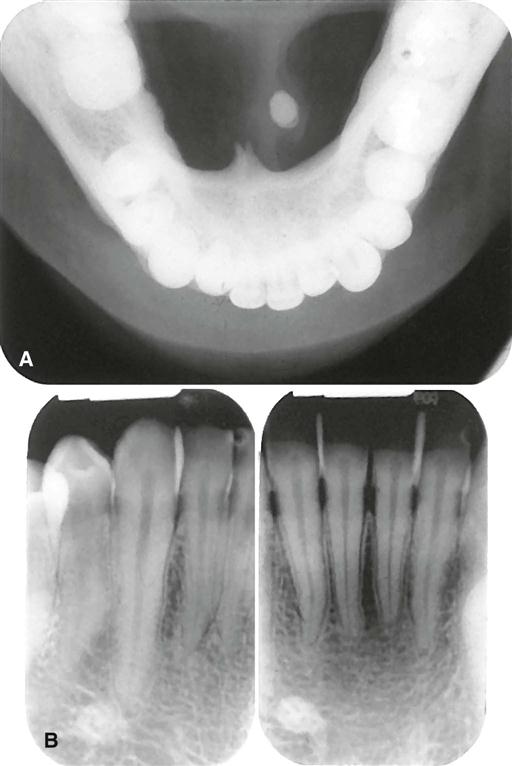
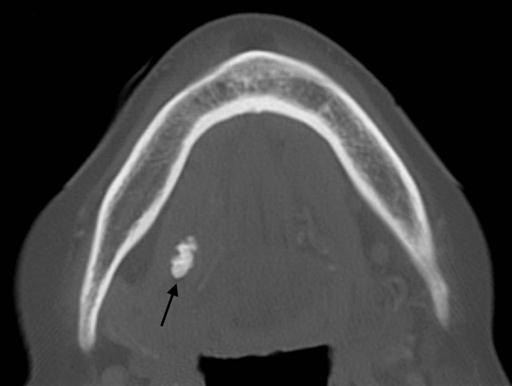
Intraoral Radiography
Sialoliths in the anterior two thirds of the submandibular duct are typically imaged with a cross-sectional mandibular occlusal projection as described in Chapter 7 (Fig. 29-1). The posterior portion of the duct may be demonstrated with an over-the-shoulder occlusal projection view, where the directing cone is placed on the shoulder and the central ray is directed in an anterior direction through the angle of the mandible, with the patient’s head rotated back and tilted to the unaffected side (Fig. 29-2).
Parotid sialoliths are more difficult to demonstrate than the submandibular variety owing to the tortuous course of Stensen’s duct around the anterior border of the masseter and through the buccinator muscle. As a rule, only sialoliths anterior to the masseter muscle can be imaged on an intraoral image. To demonstrate sialoliths in the anterior part of the duct, an intraoral image receptor is stabilized with a holder inside the cheek, as high as possible in the buccal sulcus and over the parotid papilla. The central ray is directed perpendicular to the center of the receptor.
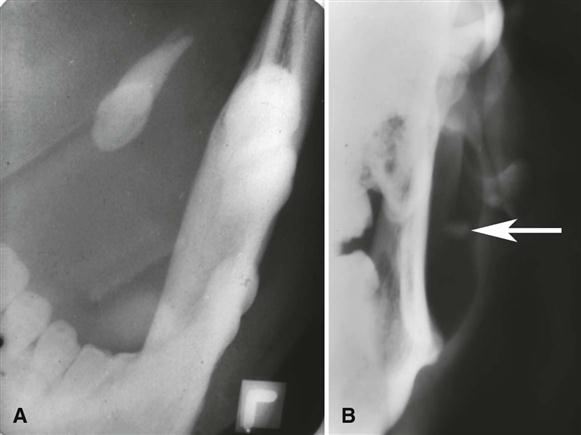
Extraoral Radiography
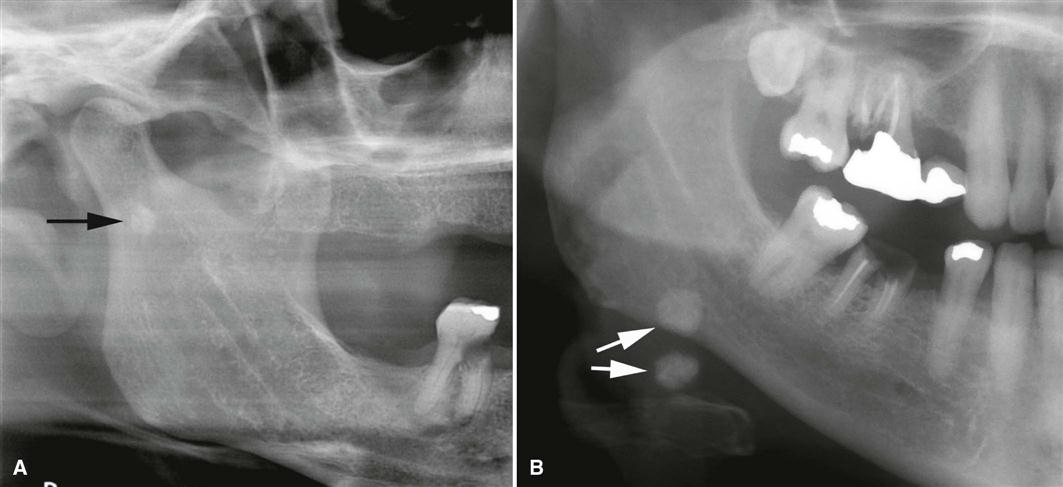
A panoramic projection frequently demonstrates sialoliths in the posterior duct or reveals intraglandular sialoliths in the submandibular gland if they are within the image layer (Fig. 29-3). The image of most parotid sialoliths is superimposed over the ramus and body of the mandible at the level of or just superior to the occlusal plane, making oblique lateral radiographs of the mandible of limited value. To demonstrate sialoliths in the submandibular gland, the lateral projection is modified by opening the mouth, extending the chin, and depressing the tongue with the index finger; this improves the image of the sialolith by moving it inferior to the mandibular border.
Sialoliths in the distal portion of Stensen’s duct or in the parotid gland are difficult to demonstrate by intraoral or lateral extraoral views. However, a posteroanterior skull projection with the cheeks puffed out may move the image of the sialolith free of the adjacent bone, rendering it visible on the projected image (see Fig. 29-2). This technique may also demonstrate interglandular sialoliths that may be obscured during sialography.
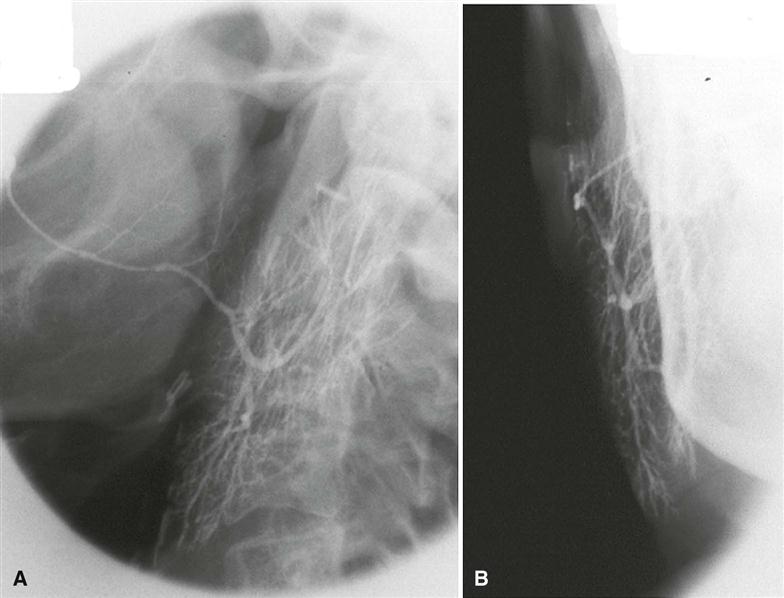
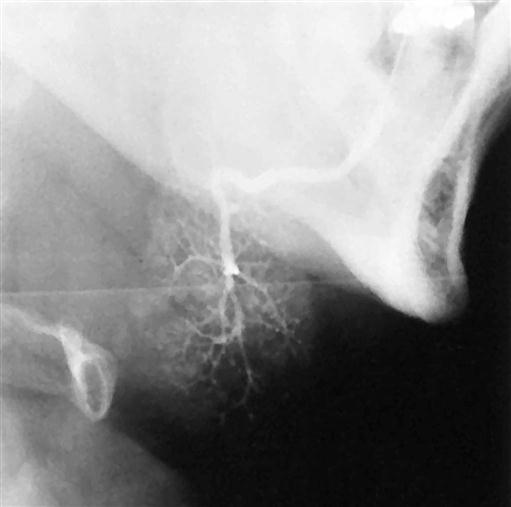
Conventional Sialography
First performed in 1902, sialography is a radiographic technique where a radiopaque contrast agent is infused into the ductal system of a salivary gland before imaging with plain films/digital image receptors, fluoroscopy, panoramic radiography, CBCT imaging, or MDCT imaging. Sialography is the most detailed way to image the ductal system (Figs. 29-4 to 29-6). CBCT imaging has been developed more recently as an imaging modality for conventional sialography. Its advantages are multiplanar and three-dimensional visualization of the ductal structures and the ability to remove overlapping anatomic structures from the image for better visualization of the gland.
The ductal systems of the parotid and submandibular glands are most readily studied with this technique. Although the sublingual gland is difficult to infuse intentionally, it may be fortuitously opacified while Wharton’s duct is infused to image the submandibular gland. A survey or “scout” image is usually acquired before infusion of the contrast solution into the ductal system as an aid in verifying the optimal exposure factors and patient positioning parameters as well as detection of radiopaque sialoliths or extraglandular pathosis.
With this technique, a lacrimal or periodontal probe is used to dilate the sphincter at the ductal orifice before the passage of a cannula (blunt needle or catheter) connected by extension tubing to a syringe containing contrast agent. Lipid-soluble (e.g., Ethiodol) or non–lipid-soluble (e.g., Sinografin) contrast solution is slowly infused until the patient feels discomfort (usually between 0.2 and 1.5 mL, depending on the gland being studied). These iodine-containing agents render the ductal system radiopaque. The filling phase can be monitored by fluoroscopy or with static projection images. The intent is to opacify the ductal system proximally to the acini. The image of the ductal system appears as “tree limbs,” with no area of the gland devoid of ducts. With acinar filling, the “tree” comes into “bloom,” which is the typical appearance of the parenchymal opacification phase (see Figs. 29-4 to 29-6). The gland is allowed to empty for 5 minutes without stimulation. If postevacuation images suggest retention of contrast agent, a sialagogue, such as lemon juice or 2% citric acid, may be administered to augment evacuation by stimulating secretion. Non–lipid-soluble contrast agents are preferred because of reports of inflammatory reactions subsequent to inadvertent extravasation of lipid-soluble agents. In addition to static projection radiographic images, the opacified gland can be imaged with CBCT, MDCT, or panoramic imaging techniques. CBCT imaging and MDCT imaging have the advantage of providing three-dimensional visualization.
Sialography is indicated for the evaluation of chronic inflammatory diseases and ductal pathoses. Contraindications include acute infection, known sensitivity to iodine-containing compounds, and immediately anticipated thyroid function tests.
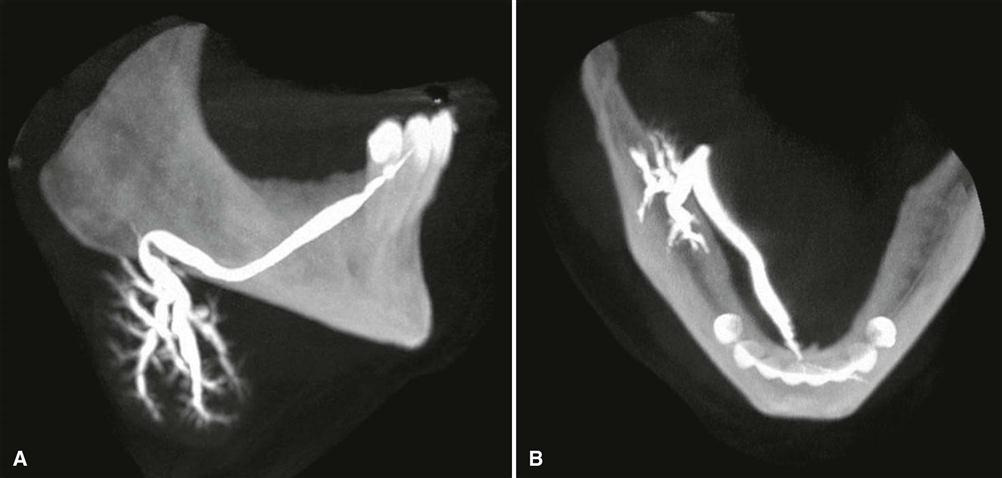
Cone-Beam Computed Tomographic Imaging
CBCT imaging is useful in evaluating structures in and adjacent to salivary glands but cannot resolve differences in soft tissue densities. Minimally calcified sialolithiasis is well depicted on CBCT imaging, and it is useful as a recording modality for conventional sialography, providing three-dimensional visualization of the ductal structure (Fig. 29-7).
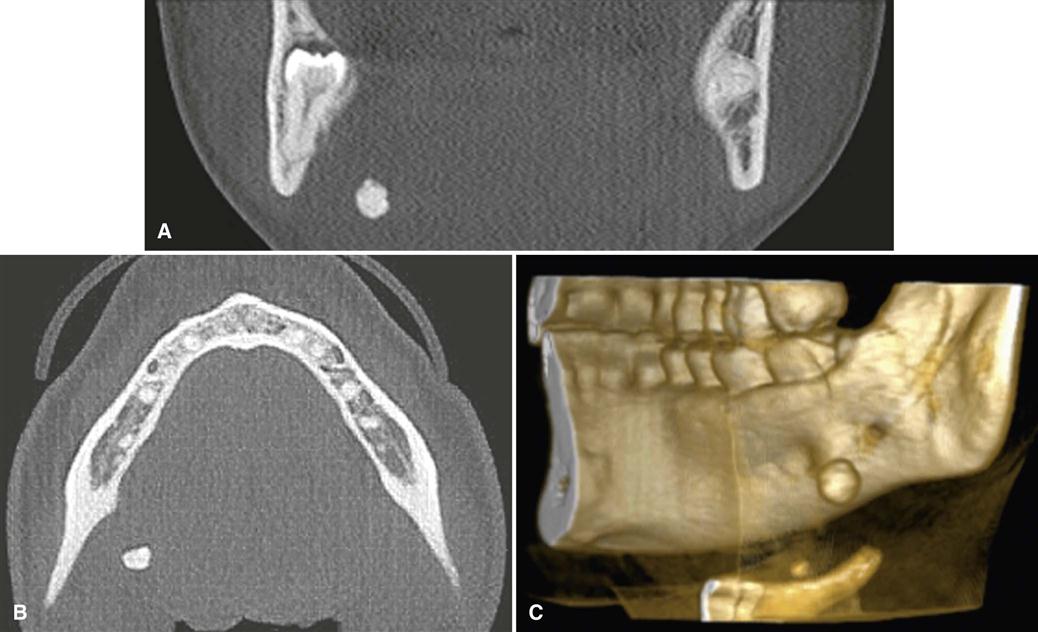
Multidetector Computed Tomographic Imaging
MDCT imaging is useful in evaluating structures in and adjacent to salivary glands; it displays both soft and hard tissues and minute differences in soft tissue densities. Thin axial and coronal images with a soft tissue algorithm are commonly acquired after intravenous administration of a contrast agent (Fig. 29-8). (See Chapter 14 for a description of the MDCT imaging process.) The imaging study is typically assessed in both hard and soft tissue windows. Glandular tissues are usually easily discernible from surrounding fat and muscle. The parotid glands are more radiopaque than the surrounding fat but less opaque than adjacent muscles. Although the submandibular and sublingual glands are similar in density to adjacent muscles, they are readily identified on the basis of shape and location. The submandibular and sublingual glands are most easily identified on directly acquired contrast-enhanced coronal MDCT scans. MDCT imaging is useful in assessing acute inflammatory processes and abscesses, cysts, mucoceles, and neoplasia. Calcifications such as sialoliths are also well depicted with MDCT imaging (Fig. 29-9). However, MDCT is not recognized as a sensitive study for salivary tumors per se.
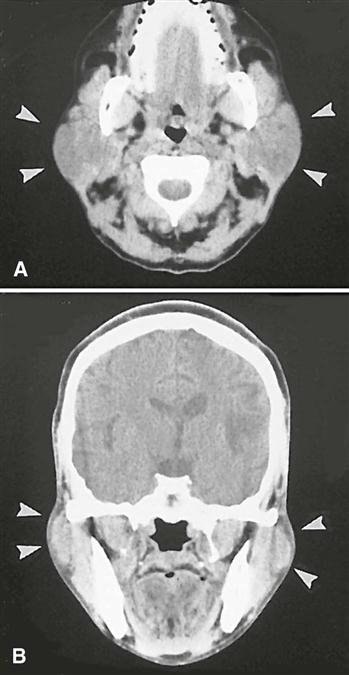
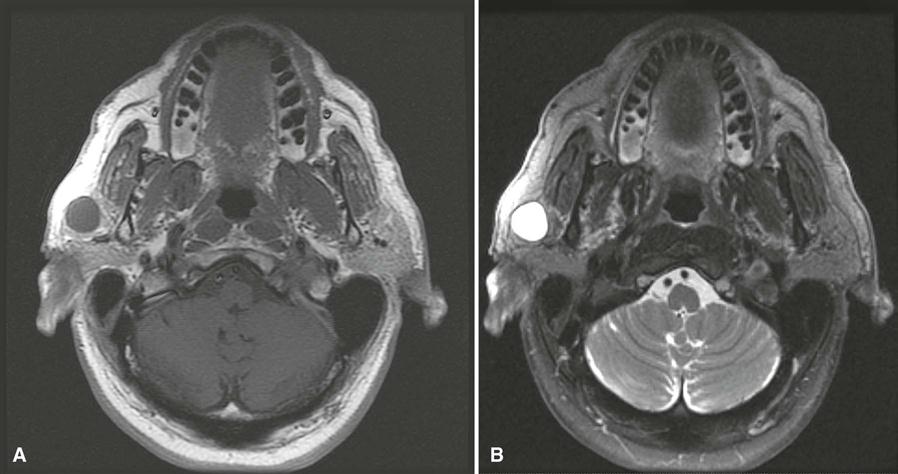
Magnetic Resonance Imaging
MRI typically provides a different and superior soft tissue contrast resolution than MDCT imaging; it also results in fewer problems with streak artifacts from metallic dental restorative materials (Fig. 29-10). (See Chapter 14 for a description of the basic concepts and principles of MRI.)
MRI can be an alternative to conventional sialography in evaluating ductal pathosis, especially when ductal catheterization is either problematic or contraindicated. Before imaging, the patient is given lemon juice or a similar sialagogue to stimulate salivation. The MRI study is performed using rapid acquisition with relaxation enhancement sequence and a three-dimensional constructive interference in steady state sequence. The images may be reformatted using a multiplanar reconstruction software algorithm.
Although indications for MDCT imaging and MRI occasionally overlap, MRI is usually the imaging method of choice in evaluating parenchymal masses or cystic lesions because of superior display of salivary gland masses, internal structures, and regional extension of the lesions into adjacent tissues or spaces, especially in examining the submandibular glands. The use of intravenous contrast agent (most commonly gadolinium) is helpful in distinguishing between cystic and solid masses and in evaluating perineural spread of malignant tumors. Sublingual masses should always be studied by MRI because of their high incidence of malignancy. Studies have shown MRI with evoked salivation, sometimes termed “MR sialography,” as a natural contrast medium to reveal ductal morphology accurately and to identify sialoliths. Axial views are acquired for all sequences, with coronal and sagittal views as needed. Noncontrast T1-weighted and T2-weighted sequences are obtained, followed by T1-weighted postcontrast, fat-suppressed images. Fast spin echo T2-weighted images may also require fat suppression.
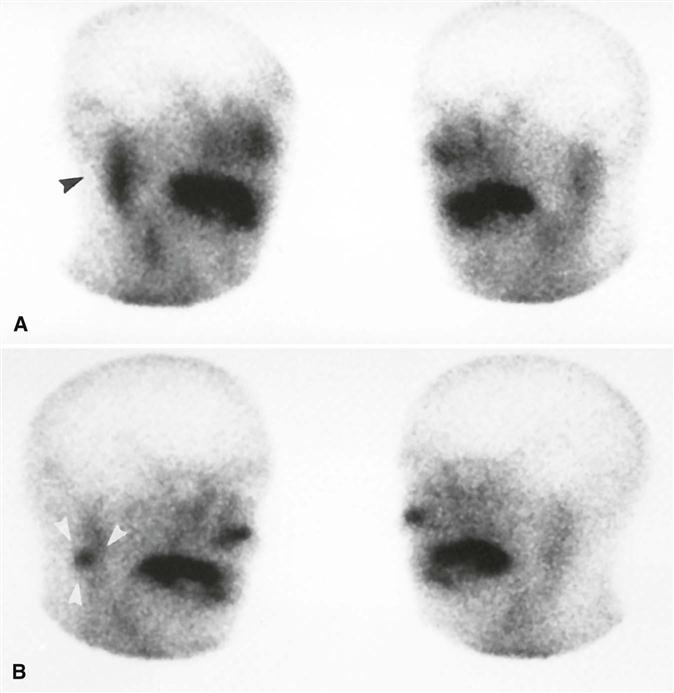
Scintigraphy (Nuclear Medicine, Positron Emission Tomography)
Nuclear medicine, or scintigraphy, provides a functional study of the salivary glands, taking advantage of the selective concentration of specific radiopharmaceuticals in the glands. (See Chapter 14 for a description of the nuclear medicine procedures used to acquire images.) When technetium 99m (99mTc)-pertechnetate is injected intravenously, it is concentrated in and excreted by glandular structures, including the salivary, thyroid, and mammary glands. The radionuclide appears in the ducts of the salivary glands within minutes and reaches maximal concentration within 30 to 45 minutes. A sialagogue is then administered to evaluate secretory capacity. All major salivary glands can be studied at once.
Although this technique has high diagnostic sensitivity, it lacks specificity and demonstrates minimal morphology. Pathosis may be demonstrated by an increased, decreased, or absent radionuclide uptake (Fig. 29-11). Lesions that concentrate 99mTc-pertechnetate are Warthin’s tumors and oncocytomas. The diagnosis of salivary gland tumors from nuclear medicine scans is not completely reliable. Because of relatively low image resolution, MDCT imaging and MRI are preferred for the evaluation of salivary masses. A specialized form of nuclear medicine is positron emission tomography (PET). Despite a much greater resolution than scintigraphy, PET has not been useful for classifying salivary tumors as benign or malignant.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses