28
The pharynx, soft palate, and larynx
Chapter contents
|
28.5 Lymphatic drainage of the pharynx, larynx, and deeper structures of the face |
28.1 Introduction
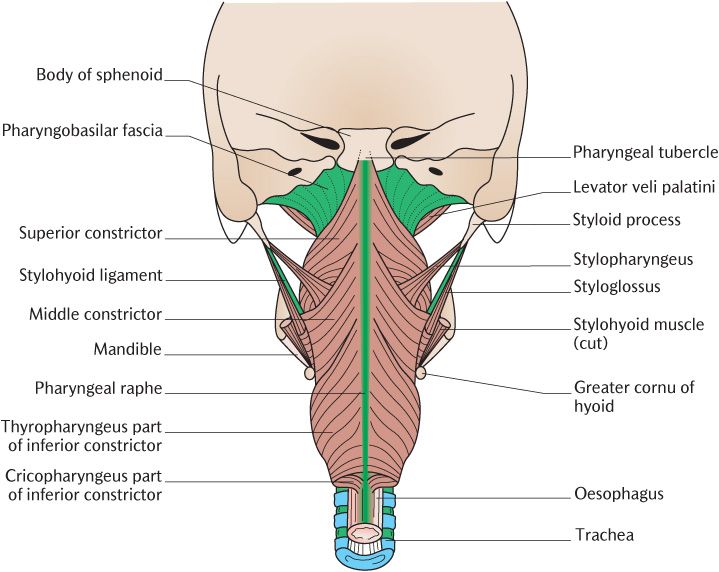
The pharynx is a muscular tube beginning behind the posterior nasal apertures and extending down to the cricoid cartilage in the neck where it becomes continuous below with the oesophagus. The pharynx is incomplete anteriorly where the nasal and oral cavities and laryngeal entrance open into it. The pharynx can thus be divided for descriptive purposes into three regions. Identify the three regions and their landmarks in Figure 28.1:
• The nasopharynx behind the posterior nasal apertures, extending down to the soft palate;
• The oropharynx posterior to the oral cavity, extending from the soft palate to the tip of the epiglottis;
• The laryngopharynx posterior to the laryngeal entrance between the epiglottis and level of the cricoid cartilage.
Air enters the nasopharynx and passes through the oropharynx to enter the larynx at the laryngopharynx. Food and drink enter the oropharynx from the mouth, then travel through the laryngopharynx to the oesophagus and stomach. The pharynx is thus part of both the gastrointestinal and respiratory tracts. Essentially, food and air cross each other’s paths in the laryngopharynx. This anatomical arrangement requires precise control of swallowing to ensure that food and drink enter the oesophagus and not the larynx.
As you can see in Figure 28.1, the larynx, the last part of the upper respiratory tract, is situated superficially in the midline of the neck in front of the pharynx and is only covered anteriorly by skin, fascia, and the infrahyoid muscles. The laryngeal opening is just behind and below the root of the tongue. The walls of the larynx are reinforced by cartilage like the lower respiratory tract. However, instead of simple cartilage rings or plates in the walls attached to each other by fibrous tissue, the elaborately shaped laryngeal cartilages articulate with each other through synovial joints and can be moved with precision by the laryngeal muscles. The vocal folds stretch anteroposteriorly across the larynx; they can be brought together to close the larynx and protect the lower respiratory tract or tensed to produce noise, the phonation component of speech.
The soft palate is a flap of muscular tissue attached to the posterior edge of the hard palate. As illustrated in Figure 28.1, it hangs down into the pharynx when relaxed. It is raised during swallowing to close off the nasopharynx to prevent food and drink entering the nasal cavity. It is also used during articulation of speech to direct air through the mouth or nose.
28.2 The pharynx
The pharynx extends from the base of the skull to the lower border of the cricoid cartilage where it is continuous with the oesophagus; it is about 12 cm long.
The nasopharynx lies behind the nasal cavity and above the soft palate. As you can see in Figure 28.1, the auditory tube opens into the lateral wall of the nasopharynx a short distance behind the nasal aperture. This opening is deepened above and behind by the tubal elevation produced by the underlying cartilage of the auditory tube. Nodules of lymphoid tissue forming the tubal tonsils are located in the mucosa around the opening of the auditory tube. The roof and posterior wall of the nasopharynx are under the body of the sphenoid and the basiocciput in the central part of the cranial base. Figure 28.1 also shows the position of the pharyngeal tonsil or adenoid which is a collection of lymphoid tissue beneath the mucosa lining the upper part of the posterior wall. Respiratory mucosa lines the nasopharynx and receives its sensory nerve supply from the maxillary trigeminal nerve and secretomotor nerves through the facial nerve via the pterygopalatine ganglion. The nasopharynx, unlike the oro- and laryngopharynx, is always open because its walls are kept patent by their attachments to the base of the skull behind and the pterygoid plates in front (see Section 28.2.1).
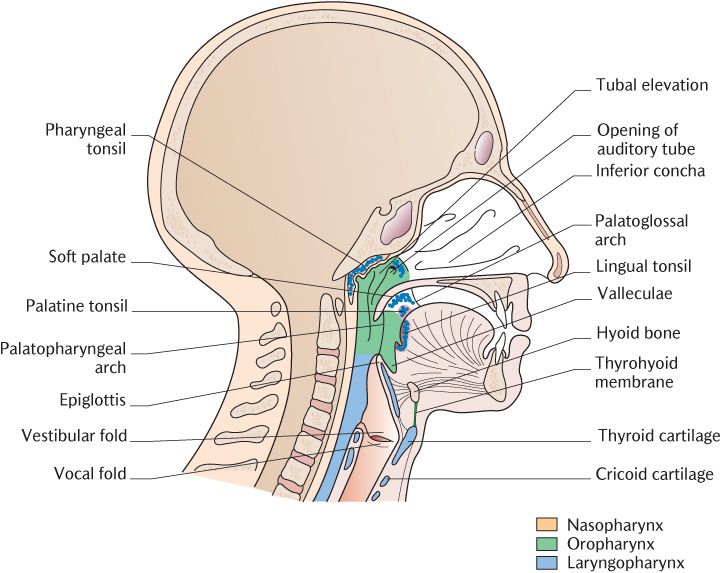
Fig. 28.1 Sagittal section of the head and neck to show the pharynx and larynx.
Box 28.1 Help! My child has swallowed part of his toy
The valleculae are about the same size as the sort of object that young children may put in their mouth such as a dried pea, a small pebble, or the head of a Lego® figure. They can become stuck in the valleculae, causing pain and minor obstruction. They cannot be removed by coughing as the airstream is deflected by the epiglottis, therefore, have to be removed manually.
The oropharynx extends from the soft palate to the tip of the epiglottis. Identify the features described in Figure 28.1. The oral cavity opens into the oropharynx anteriorly through the oropharyngeal isthmus formed by the palatoglossal arches overlying the palatoglossus muscles, descending from the soft palate to the side of the tongue. The valleculae are two shallow pits between the posterior surface of the tongue and the epiglottis separated from each other by the median glossoepiglottic fold of mucosa. The palatopharyngeal arches produced by the underlying palatopharyngeus muscles produce vertical mucosal ridges on the lateral wall of the oropharynx behind the palatoglossal arches. The tonsillar fossa is a depression between the palatoglossal and palatopharyngeal arches which contains the palatine tonsil on each side; a fibrous capsule encloses the tonsil laterally (see Figure 25.2A). The appearance of the palatine tonsils to the naked eye has already been described in Section 25.2.3. The oropharynx is lined by stratified squamous epithelium and its nerve supply is from the pharyngeal plexus (see Section 28.2.2).
The laryngopharynx extends from the epiglottis to the lower border of the cricoid cartilage. The laryngeal inlet is in its anterior wall below the epiglottis. There is a small recess termed the piriform fossa either side of the inlet (see Figure 28.11). The laryngopharynx is lined by stratified squamous epithelium and is innervated from the vagus nerve through its internal and recurrent laryngeal branches. When there is no transit of food or liquid, the laryngopharynx and oropharynx are flattened against the cervical vertebrae narrowing their lumen.
The pharyngeal, tubal, and palatine tonsils in the pharynx, together with the lingual tonsils in the posterior tongue, form an incomplete ring of lymphoid tissue around the upper parts of the respiratory and alimentary passages. The tonsils together with accumulations of lymphoid tissue in the small intestine and appendix are collectively known as mucosa-associated lymphoid tissue. They have the same functions as lymph nodes and respond to potentially harmful foreign organisms and/or their toxins entering the oropharynx through the nose or mouth by producing immune responses. The consequences of tonsillar enlargement are outlined in Box 28.2
The tonsil may become enlarged in chronic infections of the upper respiratory tract. The palatine tonsils are variable in size and frequently become infected and become enlarged and painful (tonsillitis). Adenoids, enlargement of the pharyngeal tonsil, may block the airway and lead to mouth breathing. Children are subject to novel exposure to infective organisms when they are born or start school, for instance. Their tonsils are about twice as large as adult tonsils, but the pharynx is relatively narrow so blockage is much more likely in children than adults. Infections may be treated with antibiotics, but (palatine) tonsillectomy and/or adenoidectomy may be considered after repeated chronic infections.
28.2.1 Pharyngeal muscles
The posterior and lateral pharyngeal walls are formed by three pairs of pharyngeal constrictor muscles. The pharyngeal raphe is a narrow band of connective tissue running vertically in the posterior midline of the pharynx; as shown in Figure 28.2, it is attached above to the pharyngeal tubercle, a slight elevation on the underside of the body of the sphenoid, and extends downwards to blend with the connective tissue surrounding the oesophagus. Figure 28.2 illustrates each pair of muscles sweeping around the side of the pharynx to a variety of anterior structures from their posterior attachment to the raphe. They are arranged in a superior–inferior sequence rather like stacked plant pots or ice cream cones with the muscle below partially overlapping the muscle above.
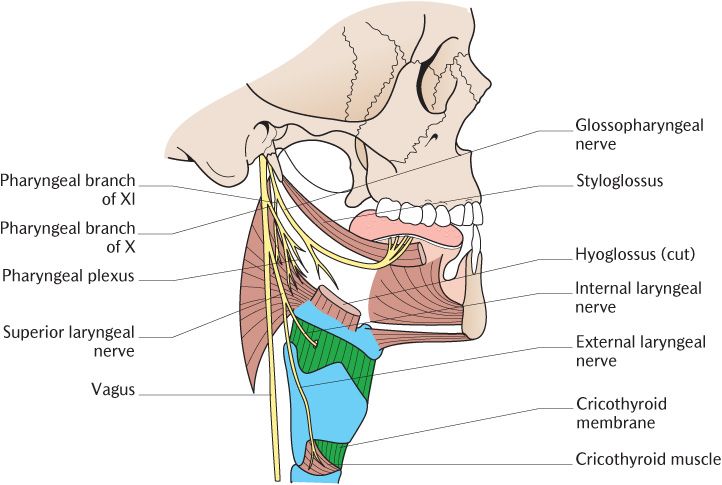
The stylopharyngeus and palatopharyngeus are more vertically orientated muscles inserted into the pharyngeal wall. Palatopharyngeus is described with the soft palate in Section 28.3.1. The muscles of the pharynx are illustrated in Figures 28.2 and 28.3; examine them as you read the following description.
The superior constrictors
The uppermost fibres of these muscles are inserted into the pharyngeal tubercle; below this, they attach to the pharyngeal raphe as far as the lower limit of the nasopharynx. The muscles form a thin sheet around the posterior and side walls of the pharynx. Each muscle attaches to the lower two-thirds of the posterior border of the medial pterygoid plate, including the hamulus and the pterygomandibular raphe below. This raphe extends between the pterygoid hamulus to the posterior end of the mylohyoid line on the medial surface of the mandible. The superior constrictors attach to it posteriorly and the buccinators anteriorly.
You can see in Figures 28.2 and 28.3 that there is a gap between the upper border of each superior constrictor muscle and the base of the skull. This is closed by the strong pharyngobasilar fascia which is pierced by the auditory tube and the levator veli palatini muscle (see Section 28.3.1).
Fig. 28.2 Posterior view of the constrictor muscles of the pharynx.
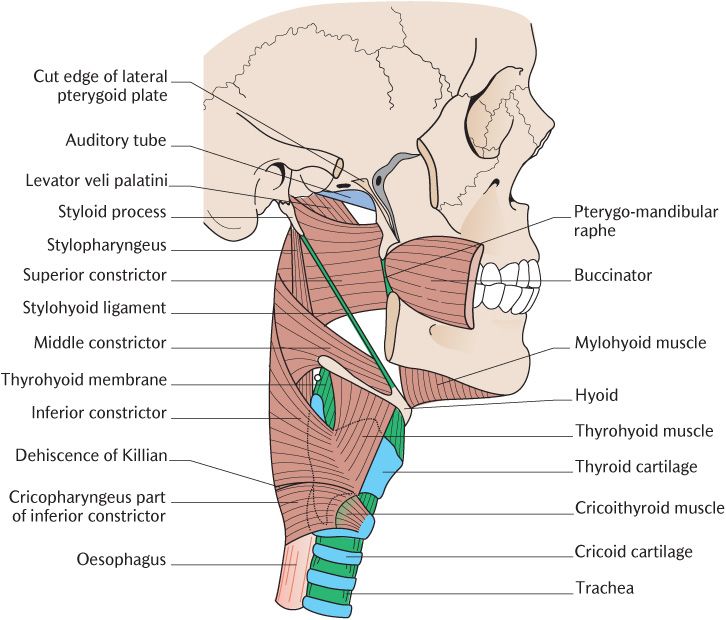
Fig. 28.3 Lateral view of the constrictor muscles of the pharynx.
The middle constrictors
The middle constrictors pass anteriorly around the pharynx from their posterior attachment to the pharyngeal raphe. The upper fibres run downwards, superficial to the lower part of the superior constrictor whereas the lower fibres run more horizontally, passing deep to the upper part of the inferior constrictor. They attach to the lower part of the stylohyoid ligament and between the lesser and greater cornua of the hyoid bone.
The inferior constrictors
Like the superior and middle constrictors, the inferior constrictor muscles attach posteriorly to the pharyngeal raphe. Each inferior constrictor consists of two parts. The upper part of the inferior constrictor runs anteriorly and downwards to the oblique line on the thyroid cartilage: it is sometimes called the thyropharyngeus and its uppermost fibres cover the inferior part of the middle constrictor. The lower part encircles the lowermost part of the pharynx in a thick band as the cricopharyngeus muscle which is sometimes regarded as a separate muscle. It is continuous inferiorly with the circular fibres of the upper part of the oesophagus and is attached anteriorly to the side of the arch of the cricoid cartilage. The inferior constrictor is attached to a tendinous band between the thyroid and cricoid cartilages which arches over the cricothyroid muscle. Killian’s dehiscence is a posterior gap between the two parts of the inferior constrictor. The mucosal lining of the pharynx may protrude through this weak area, creating a pharyngeal pouch, a potential food trap.
Their name indicates precisely the action of the pharyngeal constrictor muscles. They constrict the pharynx in a wave of contraction from above downwards, moving food and liquids through the pharynx into the oesophagus. Their action in swallowing is described in Section 29.1.2.
The stylopharyngeus muscles
Each stylopharyngeus muscle arises from the medial surface of the styloid process and runs almost vertically downwards between the internal and external carotid arteries. As you can see in Figures 28.2 and 28.3, it crosses the lower border of the superior constrictor muscle and then continues downwards inside the middle constrictor, beneath the pharyngeal mucosa, to attach to the side wall of the pharynx and the posterior border of the thyroid cartilage. Some muscle slips arise from the lower part of the auditory tube close to its opening and pass downwards to blend with the constrictor muscles; these are sometimes called the salpingopharyngeus muscle.
Stylopharyngeus is an elevator of the pharynx and larynx. It is the only muscle derived from the third pharyngeal arch and is, therefore, innervated by the glossopharyngeal nerve.
28.2.2 Nerve supply of the pharynx
The pharyngeal plexus of nerves is in the connective tissue on the superficial surface of the constrictor muscles, especially the middle constrictors. The plexus is formed from the pharyngeal branches of the glossopharyngeal and vagus nerves and sympathetic vasoconstrictor nerves from the laryngopharyngeal branch from the superior cervical sympathetic ganglion.
The glossopharyngeal branches supply sensory nerves for the mucosa of the oropharynx and parasympathetic neurons to its glands. The preganglionic parasympathetic neurons synapse with post-ganglionic neurons within the pharyngeal mucosa. The pharyngeal branch of the vagus carries motor axons to the pharyngeal constrictor muscles and most of the muscles of the soft palate.
The lining mucosa of the nasopharynx is supplied by the pharyngeal branch of the maxillary trigeminal nerve which also carries facial post-ganglionic parasympathetic neurons from the pterygopalatine ganglion. The laryngopharynx receives its sensory and parasympathetic innervation through the internal and recurrent laryngeal branches of the vagus. The internal laryngeal nerve also supplies taste buds in the mucosa of the epiglottis and valleculae.
The vagus nerves
The vagus nerves leave the cranial cavity through the middle compartment of the jugular foramina with the spinal accessory nerves. They continue vertically downwards within the carotid sheath, running between the internal jugular vein and the internal carotid artery at first, then between the internal jugular vein and the common carotid artery.
There are several branches of the vagus supplying structures in the head and neck; the more important ones are illustrated in Figure 28.4; trace them as you read the description.
The pharyngeal branch passes forwards between the internal and external carotid arteries below and parallel to the glossopharyngeal nerve to the middle constrictor where it joins with the pharyngeal branch of the glossopharyngeal nerve to form the pharyngeal plexus. The vagus supplies motor axons to the muscles of the pharynx and soft palate through this plexus.
The superior laryngeal nerve leaves each vagus below the pharyngeal branch. It descends on the side of the pharynx deep to the internal carotid artery and divides into internal and external laryngeal nerves. The internal laryngeal nerve pierces the posterior part of the thyrohyoid membrane to supply somatosensory nerves to the pharynx around the laryngeal inlet and the lining of the larynx as far down as the vocal folds. The external laryngeal nerve runs downwards on the inferior constrictor to supply the cricothyroid muscle.
Superior and inferior cardiac branches run downwards into the thorax to join the cardiac plexuses; they convey the parasympathetic innervation of the heart.
The recurrent laryngeal nerve is the lowest branch supplying structures in the neck. The course differs between the two sides. Figure 12.11A shows the right nerve leaving the vagus within the neck as it crosses in front of the subclavian artery; the nerve hooks under the artery and then ascends through the neck in the groove between the trachea and oesophagus. On the left side, the recurrent laryngeal nerve arises from the vagus at the lower border of the arch of the aorta within the thorax. As shown in Figure 12.11B, it winds beneath the arch and then ascends in the neck in the groove between the trachea and oesophagus. The recurrent laryngeal nerves on both sides are closely related to the terminal branches of the inferior thyroid artery near the lower pole of the lobe of the thyroid gland; the nerve usually passing behind but, not infrequently, between or in front of these vessels. The relationships of the recurrent laryngeal nerve to the thyroid gland and its arteries are of clinical significance in surgery of the thyroid gland (see Box 28.7). The nerve then enters the larynx deep to the lower border of the inferior constrictor behind the cricothyroid articulation. It supplies all the muscles of the larynx, except cricothyroid, the laryngeal mucosa below the vocal folds, and branches to the mucosa and muscular coats of the oesophagus and trachea.
Fig. 28.4 The vagus and glossopharyngeal nerves and the formation of the pharyngeal plexus.
Two small branches not illustrated in Figure 28.4 are the meningeal branch which supplies the dura mater of the posterior cranial fossa and the auricular branch which passes through the temporal bone to supply the skin of the auricle, the lining of the external acoustic meatus, and outer surface of the tympanic membrane.
The bulk of each vagus nerve continues downwards into the thoracic and abdominal regions and carries the parasympathetic and visceral sensory supply of the viscera of the trunk.
28.2.3 Blood supply and lymph drainage
The pharynx receives blood from various branches of the external carotid arteries. The details are given in Box 28.3 for those who require this information.
Box 28.3 Blood supply of the pharynx
The arterial branches of the external carotid artery supplying the pharynx are, from above downwards: the pharyngeal and greater palatine branches of the maxillary artery, the ascending palatine and tonsillar branches of the facial artery, ascending pharyngeal artery, branches of the lingual artery, and superior laryngeal branches of the superior thyroid arteries. The inferior laryngeal branches of the inferior thyroid arteries from the subclavian arteries complete this formidable list.
The veins draining the pharynx form a pharyngeal venous plexus on the superficial surface of the constrictor muscles. The plexus drains into the internal jugular vein and has connections to the pterygoid venous plexus.
The lymphatic channels from the pharynx pass to the deep cervical nodes, either directly or through the retropharyngeal nodes.
28.3 The soft palate
The soft palate (also called the velum) is a mobile muscular flap, consisting of four pairs of muscles attached to a fibrous aponeurosis suspended from the posterior border of the hard palate. It projects downwards and backwards, separating the nasopharynx and oropharynx. It is continuous on each side with the lateral wall of the pharynx through the palatoglossal and palatopharyngeal arches, running downwards to the tongue and side wall of the pharynx, respectively. The uvula is a conical projection of variable length, hanging from the lower free margin of the soft palate. The mucosa of the soft palate is lining oral mucosa on its oral side and respiratory mucosa on the nasopharyngeal surface which receives their sensory nerve supply from the lesser palatine branches of the maxillary trigeminal nerve.
28.3.1 Palatine musculature
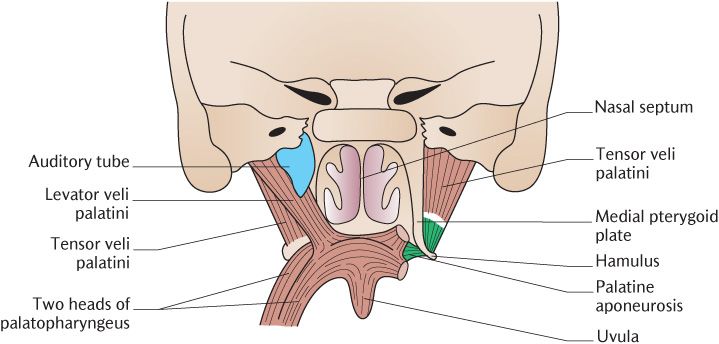
Two pairs of muscles raise and tense the soft palate and two pairs lower it. They are illustrated in Figure 28.5.
Tensor veli palatini
Each of these thin triangular muscles arises from the scaphoid fossa located at the upper end of the posterior border of the medial pterygoid plate (see Figure 24.9) and the lateral side of the cartilaginous part of the auditory tube. The fibres converge to a tendon which turns medially around the pterygoid hamulus into the soft palate. The tendon of each muscle broadens out and joins its opposite number to form the palatine aponeurosis. This thin strong sheet of fibrous tissue is attached to the posterior border of the bony palate and the other palatine muscles are attached to it.
Fig. 28.5 Posterior view of the muscles of the soft palate. The levator veli palatini and auditory tube have been removed from the right side to show the underlying muscle.
The tensor muscle does what its name implies; it tenses the palatine aponeurosis so that the other palatine muscles can act. Tensing the soft palate also produces/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses