27
The multidisciplinary management of obstructive sleep apnoea
INTRODUCTION
Obstructive sleep apnoea (OSA) is a sleep-related breathing disorder, characterised by the repeated collapse of the upper airway during sleep, with cessation of breathing. Patients are at risk of severe cardiovascular and respiratory complications, secondary to the recurrent hypoxia and hypercapnia, and the overall quality of life for sufferers and their families may be reduced.
OSA is defined as the occurrence of five or more abnormal respiratory events per hour of sleep. These abnormal events include both apnoeas (cessation of breathing, lasting 10 or more seconds) and hypopnoeas (reduction in tidal volume, accompanied by a 4% or greater fall in oxygen saturation, lasting 10 or more seconds). It is estimated that 4 per cent of middle-aged men and 2 per cent of middle-aged women are affected by OSA.1 This chapter describes the multidisciplinary management of OSA and highlights the important role dentistry can play.
AETIOLOGY OF OSA
The aetiology behind the collapse of the upper airway, during sleep, is complex and incompletely understood. OSA is thought to arise from a combination of anatomical and patho-physiological factors. A number of cephalometric studies have demonstrated the combination of a retropositioned facial skeleton and reduced oro-pharyngeal dimensions at one or more sites, between the soft palate, tongue and pharyngeal wall, which partly explains the underlying aetiology of this condition.2–5 Functional impairment of the upper airway dilatory muscles, with patients demonstrating lower tonic and phasic muscle contraction during sleep, is also thought to be an important contributor to the development of OSA.6
CLINICAL SYMPTOMS
The symptoms of OSA can be readily classified into nocturnal and daytime. Nocturnal symptoms are:
- Snoring
- Witnessed apnoeas
- Choking/gasping
- Nocturia
- Restlessness.
Daytime symptoms are:
- Excessive daytime sleepiness
- Depression
- Impaired quality of life.
The severity of OSA can be worsened by a number of aggravating factors:
- Supine sleeping position
- Alcohol consumption
- Drug therapy which acts to suppress the central nervous system
- Obesity.
DIAGNOSIS
History and Examination
A comprehensive medical and sleep history should be obtained, ideally with the patient’s sleeping partner present, to describe the degree of nocturnal disturbance experienced. Validated questionnaires, such as the Epworth Sleepiness Scale (ESS) have been designed to subjectively assess the severity of daytime sleepiness.7
Patients can also undergo an ear, nose and throat examination, in order to identify any obvious physical obstructions to breathing. Height and weight are also recorded and used to calculate the body mass index (weight in kilograms divided by the height in metres squared). Neck circumference can also provide a useful measure of upper airway compliance.
Investigations
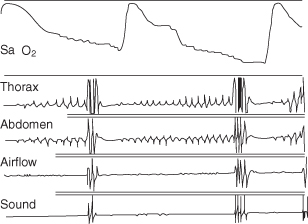
A comprehensive medical and sleep history used in conjunction with the ESS questionnaire and clinical measures described can provide useful screening for OSA. However, the diagnosis of OSA is established from an overnight sleep study. Overnight polysomnography (Figure 27.1) is regarded as the definitive investigation for the diagnosis of OSA, giving an objective measure of its severity in the form of an apnoea–hypopnoea index (AHI), in addition to oxygen saturation, brain, heart, muscle, eye activity, sleep sounds and patterns of respiration (Figure 27.2). The investigation is undertaken in a specially equipped sleep laboratory, attended by a sleep technician. OSA is typically classified as follows:
- Mild OSA – AHI 5–15 episodes per hour of sleep
- Moderate OSA – AHI 16–30 episodes per hour of sleep
- Severe OSA – AHI >30 episodes per hour of sleep.
Figure 27.1 Overnight polysomnography.
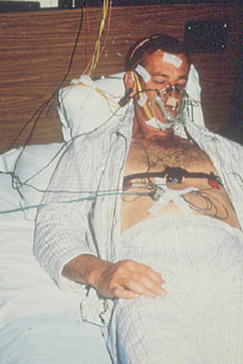
Figure 27.2 Printout from an overnight polysomnographic study of an OSA patient, illustrating repetitive episodes of apnoea and their resolution.
More recently, a number of multichannel monitoring systems have been developed to permit domiciliary sleep studies to be performed. Such limited sleep studies have been shown not only to accurately and reproducibly diagnose OSA in the home environment but also to provide reliable follow-up data during therapeutic trials in OSA subjects.8 Studies performed in this way can save on the costs of accommodation in the sleep centre and the attendant staff costs.
TREATMENT
In view of the multifactorial nature of OSA, current management strategies focus around a multidisciplinary approach. Clinicians typically involved include:
- Thoracic physician (lead clinician)
- Orthodontist
- ENT surgeon.
In addition, a variety of other specialities may be called on, including oral and maxillofacial surgeons. Treatment for OSA is based on the following approach.
Conservative Treatment
Regardless of the severity of OSA, first-line treatment aims to eliminate co-existent conditions that predispose to, precipitate or worsen upper airway dysfunction during sleep. Thus patients are advised to abstain from alcohol during the evening, avoid the use of other central nervous system depressants, ensure a/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


