Masticatory System Disorders that Influence the Periodontium
The masticatory system consists of the temporomandibular joints (TMJs), the masticatory muscles, the teeth in occlusion, and the neurologic and vascular supplies that support all of these structures. Research suggests that masticatory system disorders include many varied conditions with multiple possible contributing factors rather than different manifestations of a single disease or syndrome.2,84,129 The ability to understand the anatomy and function of the masticatory system and to correctly interpret relevant diagnostic information is a prerequisite to fulfilling comprehensive standards of care. Our diagnostic process must have a broad enough base and be inclusive enough to determine the most appropriate cause of masticatory dysfunction.137
Temporomandibular Joint
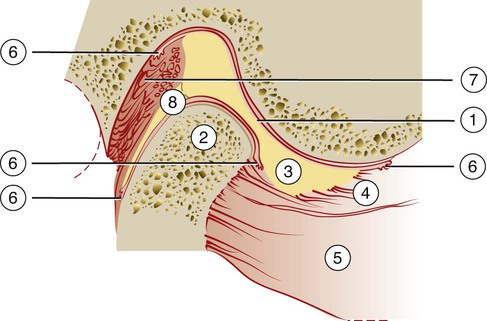
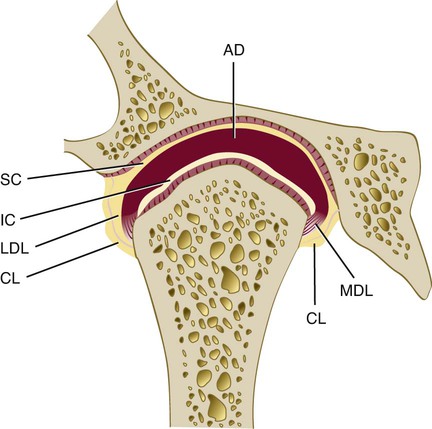
The TMJ is one of the most complex joints in the human body. It is capable of providing both hinging (rotation) and gliding (translation) movements, and it is able to resist incredible forces of mastication. The TMJ is formed by the head of the condyle of the mandible as it fits into the articular fossa of the temporal bone (Figure 27-1). The body of the mandible effectively connects both condyles so that neither condyle functions independently of the other. Interposed between the head of the condyle and the articular surface of the temporal bone is the articular disc, which consists of dense connective tissue; this results in a compound joint with two joint cavities (Figure 27-2). The articulating surfaces of the osseous structures are essentially convex in a healthy situation, so the biconcave configuration of the articular disc compensates for the opposing convexities. The articular surfaces of the condyles and the temporal bones consist of fibrous connective tissue, which renders them resistant to breakdown and capable of repair. Deep to the superficial connective tissue layer, articular cartilage provides the cellular and structural basis for the response to the functional loading and movement of the TMJs.84,137,186 The discal ligaments and attachments to the capsule, along with the disc itself, become the means of separating the joint into superior and inferior joint spaces (see Figures 27-1 and 27-2). Synovial lubrication of the articular surfaces is a function of the production of synovial fluid by endothelial cells along the borders of each joint cavity and at the anterior extent of the retrodiscal tissues.42,43,84,137,181,183,186
Muscles and Nerves of the Masticatory System
The muscles of mastication consist principally of two groups: the elevator muscles and the depressor muscles. The muscles responsible for elevating the mandible are the masseter, the internal pterygoid, and much of the temporal muscle. The posteriorly oriented fibers of the temporal muscle also retrude the mandible. The superficial muscle bundle of the masseter muscle may also assist with protruding the mandible, whereas the deeper bundle serves to stabilize the condylar head against the articular eminence. Juxtaposed with the masseter muscle, the medial pterygoid forms a muscular support for the mandible at its angle. Although its primary function is elevation of the mandible, it is also active during protrusion.84,137 The lateral pterygoid muscle is now known to function as two distinct muscles, the inferior and superior lateral pterygoid muscles, with independent and almost opposite functions.6,15 The inferior lateral pterygoid muscle depresses and protrudes the mandible. The superior lateral pterygoid muscle does not contract during depression of the mandible but rather contracts along with the elevator muscles, thereby bracing the condyle anteromedially.116,125,135,137,157
The innervation of both the capsular ligaments and the discal ligaments provide essential proprioceptive input with regard to joint position. Efferent or motor neurons cause muscle contraction in response to central cortical stimulation and in response to afferent stimuli during reflex activity.42,137,186
Pain perception causes the nociceptive reflex to open the mouth rapidly via the contraction of depressor muscles and the suppression of elevator muscles; this is consistent with other protective reflexes within the musculoskeletal system.137 Protective reflexes may be suppressed in individuals who are experiencing chronic occlusal parafunction (i.e., clenching or grinding of the teeth).27,53 Pressure perception is a function of the numerous mechanoreceptors within the PDL of teeth that are in contact. Discrimination within the dentition on the basis of the specific teeth in contact, the direction of force, the intensity of force, and their influence on muscle activity have been demonstrated in human study populations and animal studies.23,39,105,115,160 Both research and clinical observations suggest that elevator muscle contraction is suppressed when anterior teeth promote disclusion or the separation of posterior teeth during excursive mandibular movements.182
The loss of attachment that results from periodontitis involves the loss of some mechanoreceptors.
Patients with significant bone loss, significant inflammatory disruption of the integrity of the PDL, or chronic occlusal parafunction may experience the compromised regulation of muscle activity.2,26,53,81,84,130,137,155
Centric Relation
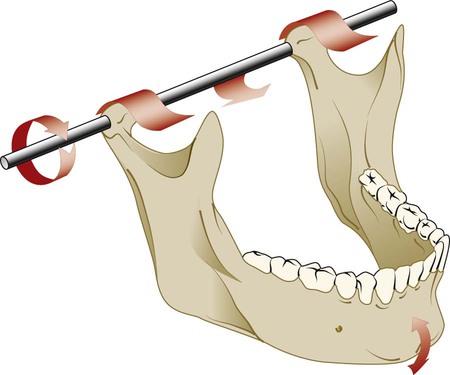
The mandible is suspended from the cranial base by ligaments and muscles. The understanding of mandibular movement begins with an initial reference point for each condyle, which is usually referred to as centric relation; this clinically determined relationship of the mandible to the maxilla occurs when both condyle–disc assemblies are positioned in their most superior position in the maxillary (or glenoid) fossa and against the slope of the articular eminence of the temporal bone. Verification of centric relation is obtained by loading the TMJs bilaterally with the teeth apart via the bimanual mandibular manipulation technique advocated by Dawson and others.42,43,44,45,172 When both condyles are in this relationship, rotation or hinging action occurs around an axis defined by the medial poles of each condyle (Figure 27-3).
The term centric relation is limited to the rotation axis through both condyles while they are seated in their respective glenoid fossae. The only occlusal consideration relative to centric relation occurs when rotation of the mandible initiates the first contact of opposing occlusal surfaces. The term initial contact in centric relation can be used to define this relationship (see Chapter 49). If the contraction of elevator muscles occurs at the point of initial occlusal contact and results in the distraction of one or both condyle–disc assemblies from their seated relationship, then centric relation is no longer occurring.42,43,44
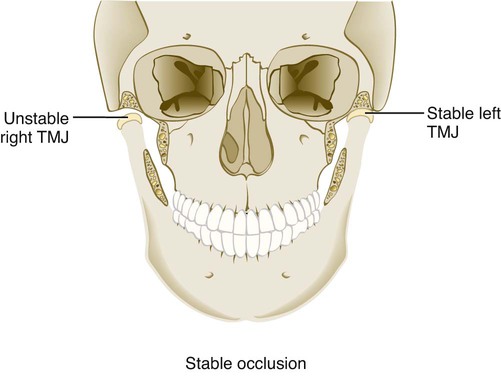
For TMJs to maintain orthopedic stability, the condyles must remain fully seated in their respective fossae when the teeth occlude in maximal intercuspation. Orthopedic instability occurs when the occlusal relationships are such that the contraction of elevator muscles is required to achieve stable occlusion in the maximal intercuspal position, which results in the unseating of one or both condyles from their respective fossae (Figure 27-4).
An individual’s susceptibility to masticatory system disorders determines whether that person adapts with minimal consequence or develops dysfunction or degeneration.26,42,43,137,172
Biomechanics of the Masticatory System
Because the maxillary teeth have a fixed relationship with the cranial base (just as mandibular teeth have a fixed relationship with the condyle), the contact of their respective occlusal surfaces may directly influence condylar position or movement.42,43,137
The mandible can move within a range of motion that is limited by skeletal, muscular, and ligamentous structures. Pure rotation of up to approximately 25 mm can occur before translation of the condyle is required to continue toward the maximal opening of the jaw. Movement of the condyle is relative to the disc, so rotation effectively occurs within the inferior joint space (Figure 27-5, A). Strict translation protrudes the mandible, whereas the condyle–disc assembly moves anterior and inferior toward the articular eminence of the temporal bone.
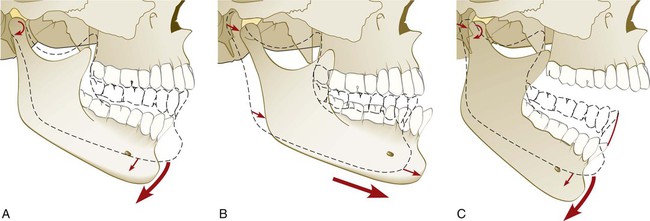
The disc moves relative to the temporal bone, and movement occurs within the upper joint space (see Figure 27-5, B). During combination translation/rotation movement of the condyle, the axis of rotation for each condyle changes as the condyle translates down the articular eminence to a position inferior to its fossa (see Figure 27-5, C). Harmonious muscle function and ligament attachments keep the condyle–disc assembly properly related so that the articular disc remains loaded in its concave avascular central portion between the condyle and the articular surface of the temporal bone. The elasticity and vascularity of the retrodiscal tissues permit anterior movement of the disc during the translation of each respective condyle.
When the teeth are in contact, their ability to influence both the position and the direction of movement of condyle–disc assemblies is defined by the intensity of muscle activity and the steepness of the inclines of those teeth.42,43,78,90,109,137
Dysfunction and Deterioration
Ideally, function never exceeds the integrity or adaptive limits of the structural elements of the masticatory system. Clinical experience shows that the tolerance of the components of the masticatory system can be exceeded by both acute trauma and chronic trauma. Acute trauma to the head and neck region can range from a distinct event, such as an accident or a blow to the face, to a sustained overuse experience, such as a long dental appointment. Acute trauma can serve as an initiating event that leads to a chronic condition, so accurate documentation and careful monitoring may prove extremely valuable should symptoms or dysfunction persist.13,20,47
Occlusal relationships that disrupt the condyle during the physiologic movement of rotation or translation require muscular and TMJ compensation. The extent to which the repeated loading of the teeth and the condyles during function and parafunction exceeds the tolerance of an individual will determine whether structural or muscular compromise occurs.137
Recently completed prospective research found only a weak association with occlusal disharmonies but significant correlations of both reported bruxism and tooth wear index with symptoms of temporomandibular disorders.24,118 When TMJ dysfunction could be correlated with specific occlusal relationships, the trend was to recognize that, when inclines of posterior teeth dominated occlusal function, masticatory system harmony was disrupted.1,30,44,56,71,77,82,128,137,180,182 Other researchers have found that various occlusal interferences and relationships are common among individuals with and without masticatory system disorders.
The researchers could not distinguish a particular occlusal feature as a specific etiologic or predisposing factor for the development of masticatory system disorders, although some found that several factors occurring together encouraged dysfunction.37,77,146,147,171 There seems to be less correlation between static references (e.g., the class of the malocclusion) and masticatory system disorders than when functional or extrafunctional occlusal forces exceed the tolerance of the TMJ and the masticatory musculature.137,159
The general terms for occlusal parafunction used in this text include bruxism, which is the grinding of the teeth, and clenching, which is when a person holds the teeth firmly together with significant force. Bruxism is usually confirmed by the observation of excessive tooth wear. The clenching type of parafunction can be distinguished from the grinding of the teeth, and it seems to be more often associated with masticatory system disorders than does bruxism.31,61,63,83,140,145 Sleep bruxism may include both tooth grinding and clenching, and it seems to occur primarily during stage 1 and stage 2 (i.e., non–rapid eye movement) sleep. These episodes often occur in association with short brain and cardiac reactivations called “microarousals.” Rhythmic masticatory muscle activity is relatively common among non-bruxers, but the frequency and intensity of the muscle contraction is substantially greater for the sleep bruxer. The central pattern generator of the primate brain stem does not modulate or reduce muscle contraction during sleep as it does during waking hours. In addition, the amplification of oral parafunction has been reported in association with a patient’s intake of selective serotonin reuptake inhibitors (e.g., Prozac).10,42,43,137,148,174
If sufficient evidence exists to suspect that the occlusal relationships in function or parafunction may have exceeded the tolerances of that individual’s masticatory system, responsible intervention or monitoring can be initiated.43,66,140,147
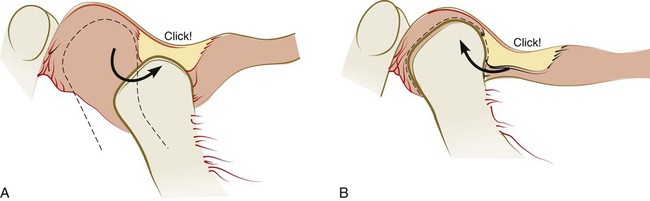
Progressive disc displacement most often begins on its lateral aspect and occurs in an anterior and medial direction as a result of the insertion of muscle fibers into the anteromedial aspect of the disc and the reported variability in resistance of the attachment of the lateral aspect of the disc.12,161 Stretching of the retrodiscal tissues and collateral ligaments permits the disc to be displaced and function to be limited in response to pain that results from compressive forces on the retrodiscal tissues. At some stage of opening, the remaining elasticity of the retrodiscal tissues and the tension of the capsular ligaments can pull the disc onto the head of the condyle, often with a discernible sound. Closing then results in the disc again becoming dislocated anteriorly, which results in a common joint sound that is often referred to as a reciprocal click36,85,86,103,104,113 (Figure 27-6).
When the disc remains anterior to the head of the condyle during rotation and the limited range of translation possible, the condition is called closed lock or disc displacement (dislocation) without reduction42,137 (Figure 27-7).
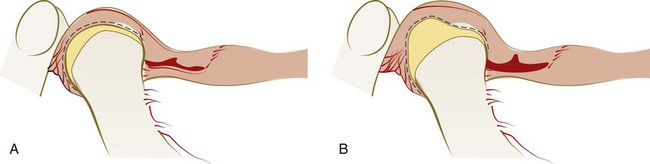
The entire disc need not be locked anterior to the head of the condyle for this condition to limit function and cause pain. The lateral aspect of the disc would be more likely than the medial aspect to be displaced anteriorly if a partial anterior disc displacement without reduction were to occur. A history of joint sounds is usually reported, although this state of the condyle–disc assembly may not result in currently discernible sounds.42,137
The vascular portion of the retrodiscal tissues being loaded between the condyle and the articular surface of the eminentia accounts for most current pain or a history of pain originating within the TMJ. The adaptation of the retrodiscal tissues to completely nonvascular fibrous tissue or perforation of the disc may account for the cessation of the painful symptoms.141
The presence of abnormal anatomic features of the condyle and fossa results in deviations in the shape of the affected articular surface to which the disc then must adapt its normal anatomy, thereby resulting in deviations in form and function. If this type of functional limitation or irregularity is observed at a consistently occurring point during jaw opening and closing, it is often within the compensatory mechanisms of the patient and should be distinguished from the disc derangements that were described previously.137
When the intensity and duration of the functional and dysfunctional loading of the TMJs result in injury, molecular agents appear to be active in the degeneration of joints. Free radicals, various catabolic enzymes, neuropeptides, estrogen, cytokines, and prostaglandins are implicated in inflammatory reactions that have an impact on the articular surfaces and the synovial fluid.58,69,94,97,99,126,127,133,151,163 The loss of the ability of the synovial fluid to lubricate articular surfaces can result in adherence of the disc. The limitation of rotation occurs with adherence between the disc and the condyle, whereas fixation of the disc against the fossa permits rotation but does not allow the disc to move forward during translation.137
Hypermobility (subluxation) of the TMJ can permit the condyle to translate beyond the eminentia, with both the disc and the condyle located beyond its prominence. The combination of anatomic features that predisposes individuals to subluxation often allows for the self-reduction of the condyles. When the condyles translate beyond the eminentia but the discs are trapped posteriorly, the combined steepness of the disc and the eminentia prevents the reduction of each condyle, and the mandible is locked open.137
Orofacial Pain
Discomfort associated with masticatory system disorders falls under the larger umbrella of orofacial pain. Pain associated with TMJ dysfunction is most frequently muscular in origin,42 and it may be amplified by both occlusal parafunction and stress.64 Although pain itself is a complex entity,168 a working knowledge of even the uncommon sources of pain perceived in the region of the masticatory system is essential to providing comprehensive diagnosis and treatment.
Sources of dental or periodontal pain should be identified by clinical, radiographic, and historic information. Nondental sources of pain include TMJ structures, muscles, cervical structures, neuropathies, vascular inflammation, all types of headache, sleep disorders, systemic disorders, and psychoimmune neurologic sources.136 A survey of 45,700 American households revealed that 22% of respondents had experienced some type of orofacial pain during the previous 6 months, thereby establishing a meaningful probability that the periodontal patient’s list of symptoms includes pain.11
Box 27-1 provides the current list of possible sources of orofacial pain. This list was prepared by the American Academy of Orofacial Pain.136
Headache pain is perceived primarily within the trigeminal nerve pathways, although other cranial and cervical nerves may offer painful sensory input.84,136,158 Pain that originates in masticatory system structures, which are also innervated by the trigeminal nerve, requires diagnostic differentiation from headache pain.159
Headache can present in a myriad of forms, and it can influence the perception of pain and the diagnosis of the origin of pain.84,136
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


