Correction of Dentofacial Deformities
Myron R. Tucker and Brian B. Farrell
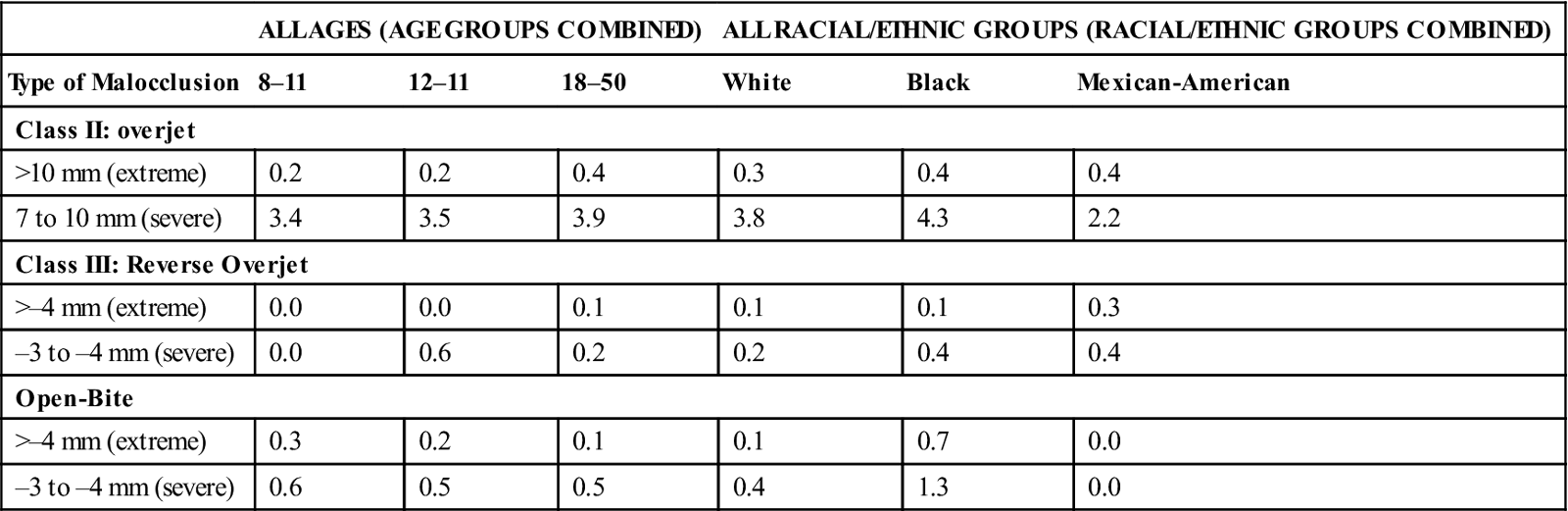
Prevalence of Dentofacial Deformities
Epidemiologic surveys demonstrate that a large percentage of the United States’ population has a significant malocclusion.1–3 Very little data describe the exact prevalence of significant skeletal facial deformity. This information can be extrapolated from studies that have evaluated the prevalence of severe malocclusion. The National Health and Nutrition Examination Survey (NHANES III), conducted from 1989 to 1994, obtained a sample of 14,000 individuals ages 8 through 50 years, which roughly approximates the general U.S. population. In this study, information was collected describing overjet and reverse overjet, vertical overlap (deep bite and open bite), and posterior cross-bites.1 It can be assumed that patients with extreme values in each of these categories have underlying facial deformities (Table 26-1). Because many patients have dental compensations for skeletal growth abnormalities (described later in this chapter), this study likely underestimates the severity of skeletal abnormalities. This type of data, combined with other criteria that clearly define the most severe characteristics of a malocclusion such as overjet versus crowding, can help to estimate more accurately the prevalence of skeletal abnormality that may require surgical correction as part of the treatment for malocclusion.2
Table 26-1
Percentage of the U.S. Population with Severe or Extreme Malocclusion
< ?comst?>
| ALL AGES (AGE GROUPS COMBINED) | ALL RACIAL/ETHNIC GROUPS (RACIAL/ETHNIC GROUPS COMBINED) | |||||
| Type of Malocclusion | 8–11 | 12–11 | 18–50 | White | Black | Mexican-American |
| Class II: overjet | ||||||
| >10 mm (extreme) | 0.2 | 0.2 | 0.4 | 0.3 | 0.4 | 0.4 |
| 7 to 10 mm (severe) | 3.4 | 3.5 | 3.9 | 3.8 | 4.3 | 2.2 |
| Class III: Reverse Overjet | ||||||
| >–4 mm (extreme) | 0.0 | 0.0 | 0.1 | 0.1 | 0.1 | 0.3 |
| –3 to –4 mm (severe) | 0.0 | 0.6 | 0.2 | 0.2 | 0.4 | 0.4 |
| Open-Bite | ||||||
| >–4 mm (extreme) | 0.3 | 0.2 | 0.1 | 0.1 | 0.7 | 0.0 |
| –3 to –4 mm (severe) | 0.6 | 0.5 | 0.5 | 0.4 | 1.3 | 0.0 |
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
Data from Proffit WR: Malocclusion and dentofacial deformity in contemporary society. In: Proffit WR, Fields HW, Jr., Sarver DM, eds: Contemporary orthodontics, ed 4, St Louis, MO, 2007, Mosby.
It appears that about 2% of the U.S. population has mandibular deficiency, vertical maxillary excess that is severe enough to be considered a handicap, or both.3 Other abnormalities and their percentages of prevalence in the population include mandibular excess, maxillary deficiency, or both, 0.3%; open bite, 0.3%; and asymmetry, 0.1%. Therefore, it appears that approximately 2.7% of the U.S. population may have a dentofacial deformity contributing to malocclusion that will require surgical treatment for correction.
Historically, treatment of malocclusions, even those associated with dentofacial deformities, has been aimed at correction of dental abnormalities, with little attention to the accompanying deformity of the facial skeleton. In the last 60 years, surgical techniques have been developed to allow positioning of the entire midface complex, the mandible, or dentoalveolar segments to any desired position. The combining of surgical and orthodontic procedures for dentofacial deformities has become an integral part of the correction of malocclusions and facial abnormalities.
Causes of Dentofacial Deformity
Malocclusion and associated abnormalities of the skeletal components of the face can occur as a result of a variety of factors, including inherited tendencies, prenatal problems, systemic conditions that occur during growth, trauma, and environmental influences. Although it is not within the scope of this book to present a detailed discussion of facial growth, an understanding of basic principles as they relate to the development of dentofacial deformities is essential. Enlow and Han’s Essentials of Facial Growth should be reviewed for a more complete discussion of the principles of facial growth.4
General Principles of Facial Growth
The development of proper craniofacial form and function is a complex process affected by many factors. In the area of the craniofacial complex, some parts appear to have their own intrinsic growth potential, including the spheno-occipital and sphenoethmoidal synchondroses and the nasal septum. In addition, the majority of growth of the bones of the face occurs in response to adjacent soft tissue and the functional demands placed on underlying bone. These soft tissue influences include the nasal, oral, and hypopharyngeal airway; facial muscles; and muscles of mastication.5
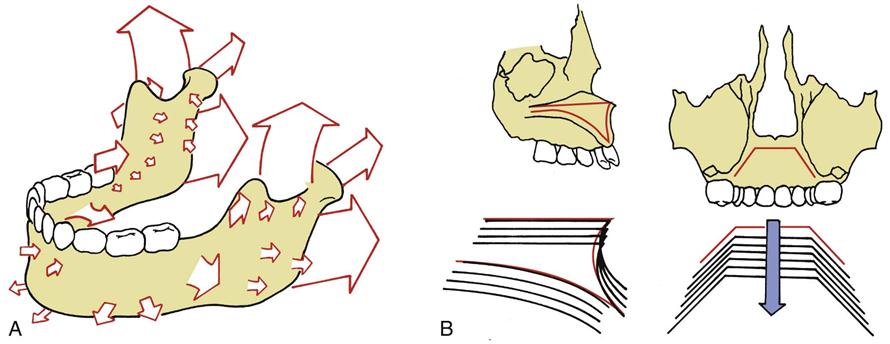
The general direction of normal growth of the face is downward and forward with lateral expansion. The maxilla and the mandible appear to grow by remodeling or differential apposition and resorption of bone, producing changes in three dimensions. Enlow and Hans describe this phenomenon as area relocation, with the maxillary–mandibular complex enlarging in the downward and forward direction as an “expanding pyramid” (Figure 26-1).4 The direction and amount of growth characterize an individual’s growth pattern.6 Alterations in the pattern of growth or in the rate at which this growth occurs may result in abnormal skeletal morphology of the face and an accompanying malocclusion.
Genetic and Environmental Influences
Genetic influence certainly plays a role in dentofacial deformities. Patterns of inheritance such as a familial tendency toward a prognathic or deficient mandible are often seen in a patient with a dentofacial deformity. However, the multifactorial nature of facial development precludes the prediction of an inherited pattern of a particular facial abnormality.
Abnormal facial growth and associated malocclusions are sometimes associated with congenital abnormalities and syndromes. Some of these syndromes such as hemifacial microsomia and mandibulofacial dysostosis (Treacher Collins syndrome) are related to embryonic abnormalities of neural crest cells. Other congenital abnormalities affecting jaw growth include cleft lip and palate and craniosynostosis (premature fusions of craniofacial sutures). Facial growth abnormalities may be caused by conditions related to maternal systemic influences, for example, fetal alcohol syndrome, which may result in hypoplasia of midface structures.
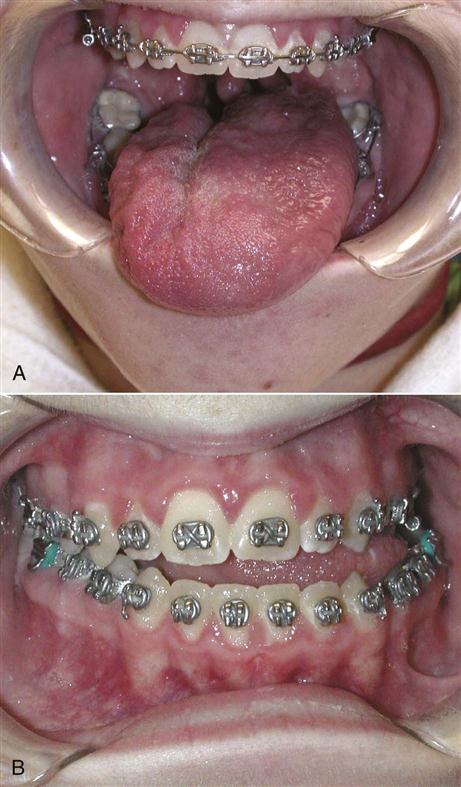
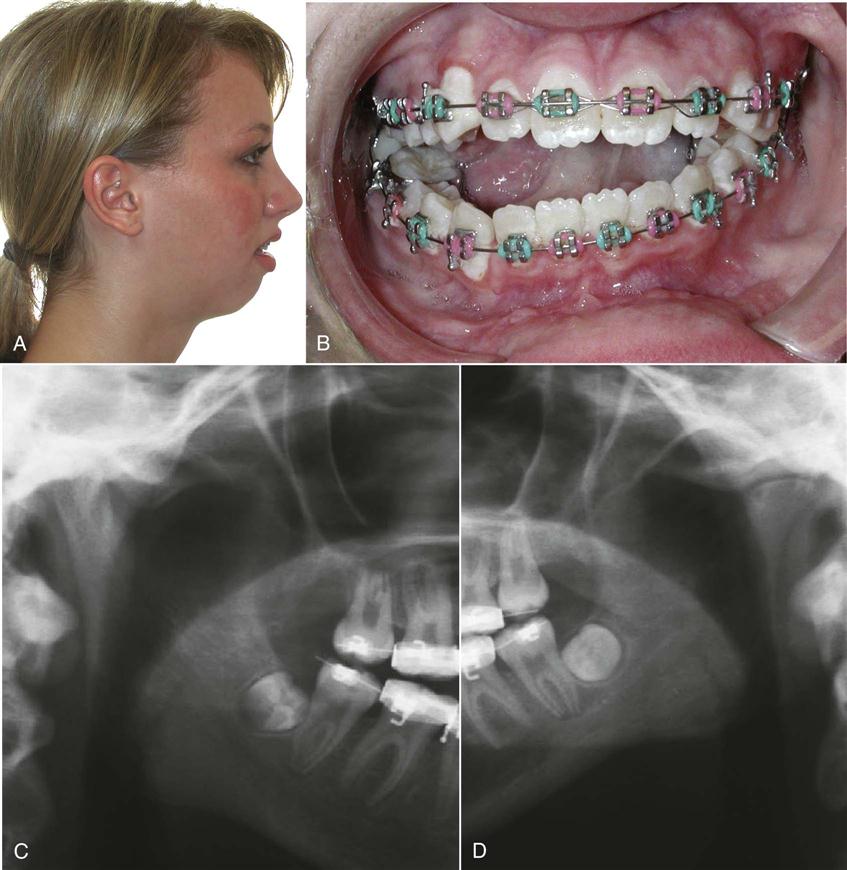
Environmental influences also play a role in the development of dentofacial deformities. As early as the prenatal stage, intrauterine molding of the developing fetal head may result in a severe mandibular deficiency. Abnormal function after birth also may result in altered facial growth because soft tissue and muscular function often influence the position of teeth and growth of the jaws. Abnormal tongue position or size can affect the position and growth of the maxilla and the mandible (Figure 26-2). Respiratory difficulty, mouth breathing, and abnormal tongue and lip postures can adversely influence facial growth.7 Trauma to the bones of the face can result in severe abnormalities of the facial skeleton and the occlusion. In addition to the abnormality that occurs as an immediate result of trauma, further effects on the development of facial bones may occur. In the case of temporomandibular joint (TMJ) trauma in a growing child, significant restriction of jaw function may occur as a result of scarring or bony or fibrous ankylosis. Subsequent alteration of growth may result with deficient or asymmetric mandibular growth (Figure 26-3).
Evaluation of Patients with Dentofacial Deformity
In the past, patients with dentofacial deformities were often treated by individual practitioners. Some patients have been treated with orthodontics alone, with a resultant acceptable occlusion but a compromise in facial esthetics. Other patients have had surgery without orthodontics in an attempt to correct a skeletal deformity, which resulted in improved facial esthetics but a less than ideal occlusion. In addition to orthodontic and surgical needs, these patients often have many other problems requiring periodontic, endodontic, complex restorative, and prosthetic considerations.
Many areas of dental practice, in addition to orthodontics and surgery, must be integrated to address the complex problems of patients with dental deformities. This integrated approach, used throughout the evaluation, presurgical, and postsurgical phases of patient care, provides the best possible results for these patients.8
The most important phase in patient care centers on evaluation of the existing problems and definition of treatment goals. At the initial appointment, a thorough interview should be conducted with the patient to discuss the patient’s perception of the problems and the goals of any possible treatment. The patient’s current health status and any medical or psychological problems that may affect treatment are also discussed at this time.
The involved orthodontist and oral-maxillofacial surgeon should conduct a thorough examination of facial structure, with consideration of frontal and profile esthetics.
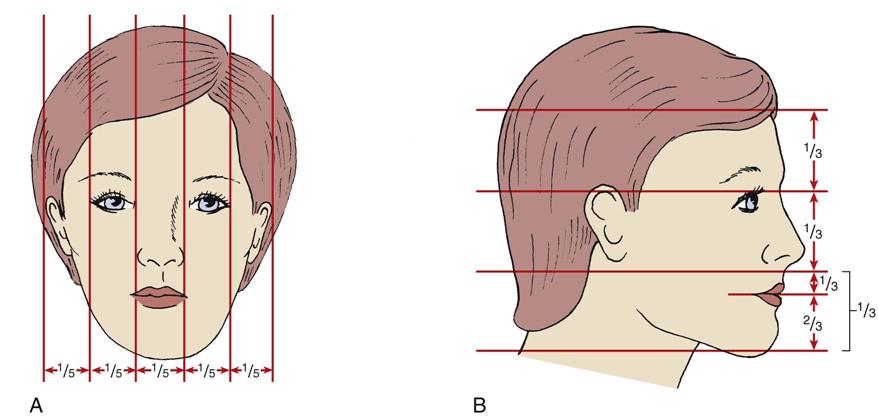
Evaluation of facial esthetics in the frontal view should assess the presence of asymmetries and evaluate overall facial balance. The evaluation should include assessment of the position of the forehead, eyes, infraorbital rims, and malar eminences; configuration of the nose, including the width of the alar base; paranasal areas; lip morphology; relationship of the lips to incisors; and overall proportional relationships of the face in the vertical and transverse dimensions. Figure 26-4 demonstrates normal facial proportions. The profile evaluation allows an assessment of the anteroposterior and vertical relationships of all components of the face. The soft tissue configuration of the throat should also be evaluated. Photographic documentation of the pretreatment condition of the patient should be a standard part of the evaluation. Video and digital computerized images have been introduced over the past decade as an additional aid in evaluating facial morphology.
A complete dental examination should include assessment of dental arch form, symmetry, tooth alignment, and occlusal abnormalities in the transverse, anteroposterior, and vertical dimensions. The muscles of mastication and TMJ function should also be evaluated. A screening periodontal examination, including probing, should assess the patient’s hygiene and current periodontal health status. Impressions and a bite registration for dental cast construction and evaluation should also be obtained at this time.
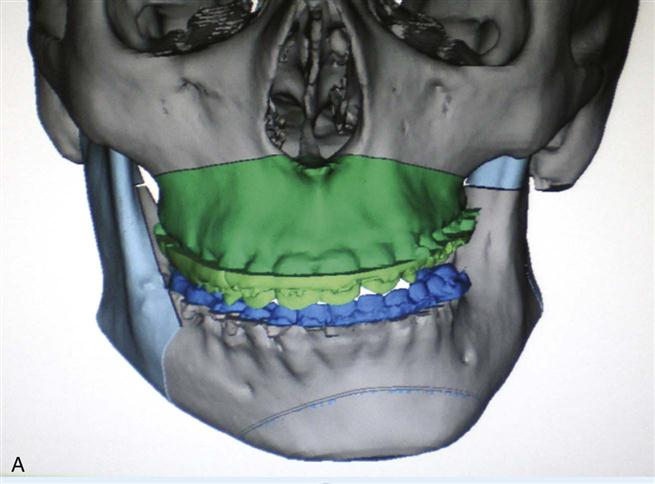
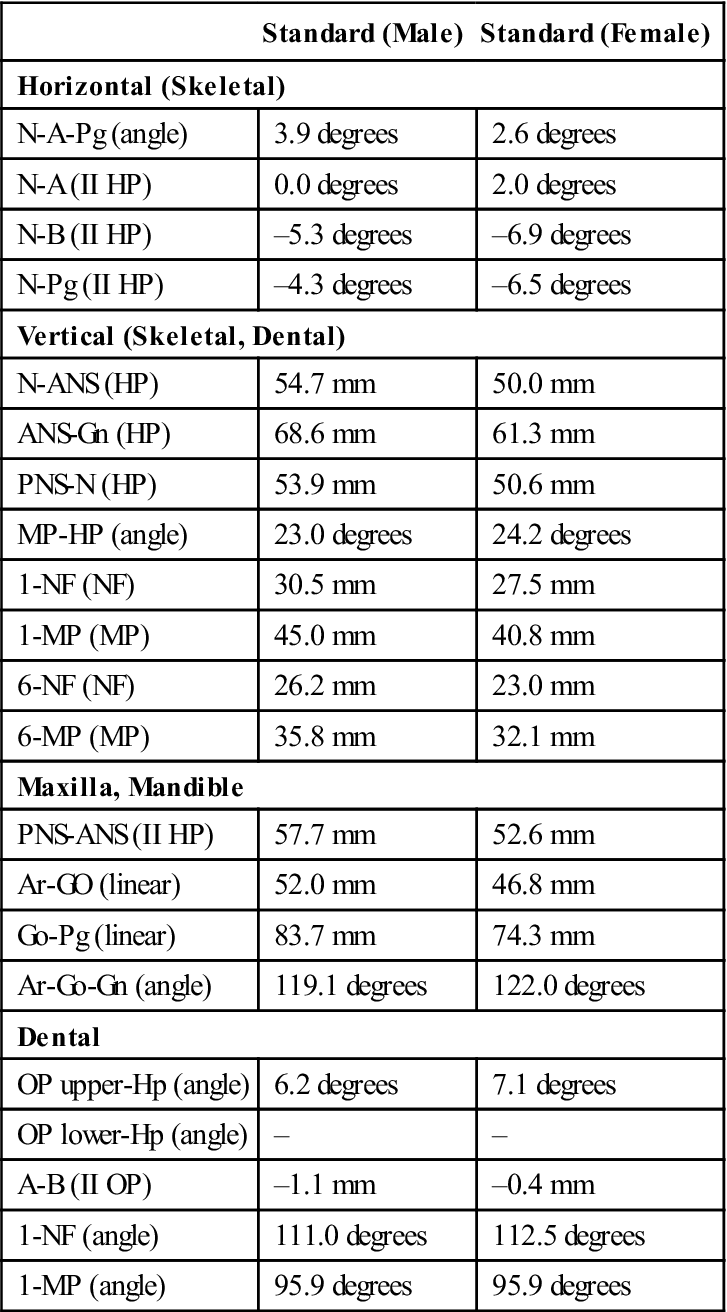
Lateral cephalometric and panoramic radiographs are routinely used in the patient evaluation and are an important part of the initial assessment. The cephalometric radiograph can be evaluated by several techniques to aid in the determination of the nature of the skeletal abnormality (Figure 26-5; Table 26-2).9,10 An important note, however, is that cephalometric radiographs are only a part of the evaluation process; they are used as adjunctive diagnostic tools in the clinical assessment of the patient’s facial structure and occlusion. Other radiographic images may be helpful in evaluating patients for surgical correction. These may include posteroanterior facial films, TMJ images when indicated, and conventional and cone beam computed tomography (CBCT) (Figure 26-6). In difficult, complex cases, it may be helpful to obtain a stereolithic three-dimensional model constructed from CT data. Computerized digital technology helps integrate cephalometric data with digital images of the face to improve evaluation of the relationship of the underlying facial skeleton and overlying soft tissue. After careful clinical assessment and evaluation of the diagnostic records, a problem list and treatment plan should be developed, combining the opinions of all practitioners participating in the patient’s care, including the orthodontist, oral-maxillofacial surgeon, periodontist, and restorative dentist.
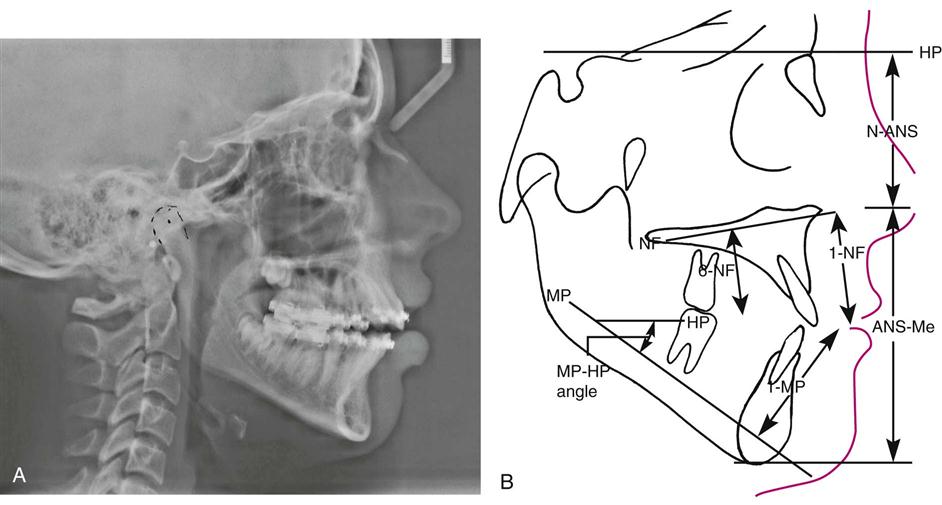
Table 26-2
Orthognathic Cephalometric Analysis
< ?comst?>
| Standard (Male) | Standard (Female) | |
| Horizontal (Skeletal) | ||
| N-A-Pg (angle) | 3.9 degrees | 2.6 degrees |
| N-A (II HP) | 0.0 degrees | 2.0 degrees |
| N-B (II HP) | –5.3 degrees | –6.9 degrees |
| N-Pg (II HP) | –4.3 degrees | –6.5 degrees |
| Vertical (Skeletal, Dental) | ||
| N-ANS (HP) | 54.7 mm | 50.0 mm |
| ANS-Gn (HP) | 68.6 mm | 61.3 mm |
| PNS-N (HP) | 53.9 mm | 50.6 mm |
| MP-HP (angle) | 23.0 degrees | 24.2 degrees |
| 1-NF (NF) | 30.5 mm | 27.5 mm |
| 1-MP (MP) | 45.0 mm | 40.8 mm |
| 6-NF (NF) | 26.2 mm | 23.0 mm |
| 6-MP (MP) | 35.8 mm | 32.1 mm |
| Maxilla, Mandible | ||
| PNS-ANS (II HP) | 57.7 mm | 52.6 mm |
| Ar-GO (linear) | 52.0 mm | 46.8 mm |
| Go-Pg (linear) | 83.7 mm | 74.3 mm |
| Ar-Go-Gn (angle) | 119.1 degrees | 122.0 degrees |
| Dental | ||
| OP upper-Hp (angle) | 6.2 degrees | 7.1 degrees |
| OP lower-Hp (angle) | – | – |
| A-B (II OP) | –1.1 mm | –0.4 mm |
| 1-NF (angle) | 111.0 degrees | 112.5 degrees |
| 1-MP (angle) | 95.9 degrees | 95.9 degrees |
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
Modified from Burstone CJ, James RB, Legan H, et al: Cephalometrics for orthognathic surgery. J Oral Surg 36:269, 1978.
Presurgical Treatment Phase
Periodontal Considerations
As the first step in treatment, gingival inflammation must be brought under control and the patient’s cooperation ensured. In patients who are unwilling or unable to clean their teeth properly before the placement of orthodontic appliances, oral hygiene procedures will be even less effective when complicated by orthodontic band placement.
Periodontal therapy includes oral hygiene instruction, scaling, and root planing; in certain instances, flap surgery to gain access for root planing may be necessary to provide proper tissue health. Whenever possible, it is advisable to delay comprehensive treatment until adequate patient compliance and control of inflammation are achieved.
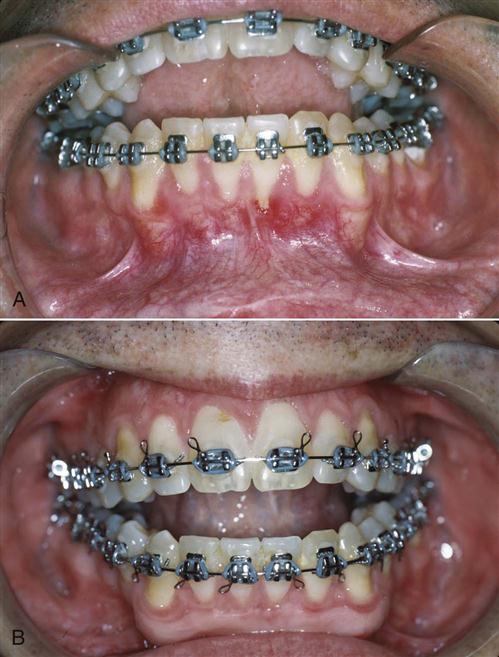
As a result of the periodontal examination findings and proposed orthodontic and surgical plan, mucogingival surgery is often accomplished during this initial phase of therapy to provide a zone of attached keratinized tissue that is more resistant to potential orthodontic and surgical trauma. Soft tissue grafting is indicated in areas that have no keratinized gingiva or where only a thin band of keratinized tissue with little or no attachment is found when an increase in tissue trauma is likely (Figure 26-7). Such trauma to these areas includes labial orthodontic movement of teeth or a surgical procedure such as an inferior border osteotomy or segmental osteotomies in interdental areas.
Restorative Considerations
During the presurgical restorative phase, the patient is evaluated for carious lesions and faulty restorations. Teeth should be evaluated endodontically and periodontally for restorability, and any nonrestorable teeth should be extracted before surgical intervention. All carious lesions must be restored early in the presurgical treatment phase. Existing restorations must function for 18 to 24 months during the orthodontic and surgical treatment phases, requiring that more durable restorative materials (i.e., amalgam and composite resin) be used, even though they may be replaced during the definitive postsurgical treatment phase. It is wise to delay the final restorative treatment until the proper skeletal relationships are achieved and the finishing orthodontics are completed.
In the edentulous or partially edentulous patient, particular attention is paid to residual ridge shape and contour in denture-bearing areas. The distance between the maxillary tuberosity, posterior mandible, and ramus areas must be evaluated to ensure that adequate space is present for partial or complete dentures. Teeth that serve as removable partial denture abutments should be evaluated for potential retentive undercuts. If minor orthodontic movement can enhance undercuts, this information is conveyed to the orthodontist.
Presurgical Orthodontic Considerations
Obviously, not all malocclusions require correction with surgery. When the skeletal discrepancy is minimal and orthodontic compensation does not adversely affect dental or facial esthetics or post-treatment stability, orthodontic treatment alone may be the treatment of choice. However, in some cases an adequate occlusal relationship cannot be achieved because of the skeletal discrepancy; some patients may be treated with orthodontic compensation for a skeletal abnormality, resulting in an adequate occlusion but poor facial or dental esthetics or a poor long-term prognosis for post-treatment retention. These patients should be considered for surgery combined with orthodontic treatment.
Treatment timing.
Treatment of the stable adult deformity can be started without delay, but questions often arise about how best to manage the growing child who is identified as having a developing dentofacial deformity. If the facial pattern is favorable and significant growth potential remains, growth modification with techniques such as functional appliance therapy or headgear may be the preferred approach. For patients with unfavorable growth patterns or severe skeletal abnormalities or who are unwilling to undergo attempts at growth modification, surgery is usually the preferred treatment. As a general guideline, orthognathic surgery should be delayed until growth is complete in patients who have problems of excess growth, although surgery can be considered earlier for patients with growth deficiencies.
Orthodontic treatment objectives.
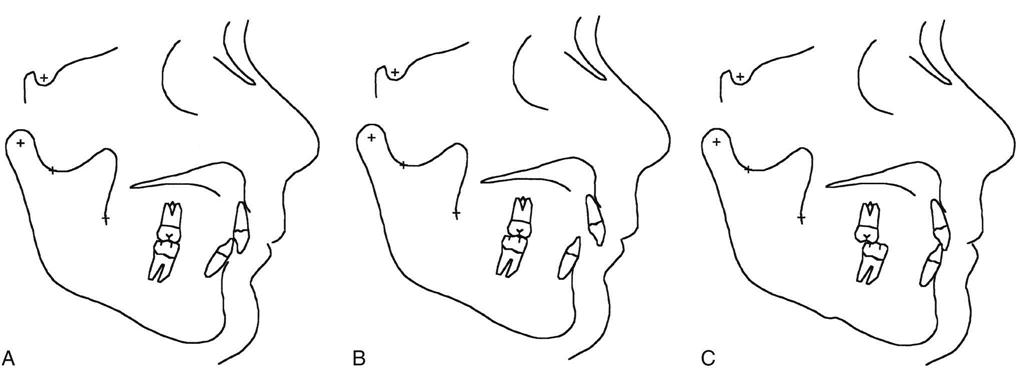
Undesirable angulation of the anterior teeth occurs as a compensatory response to a developing dentofacial deformity. For example, a patient with maxillary deficiency, mandibular excess, or both often has dental compensation for the skeletal abnormality with flared upper incisors and retracted or retroclined lower incisors (Figure 26-8, A to C). Dental compensations for the skeletal deformity are corrected before surgery by orthodontically repositioning teeth properly over the underlying skeletal component, without considerations for the bite relationship to the opposing arch. This presurgical orthodontic movement accentuates the patient’s deformity but is necessary if normal occlusal relationships are to be achieved when the skeletal components are properly positioned at surgery (see Figure 26-8, D to F). The surgical treatment then results in an ideal position of the skeletal and dental components (see Figure 26-8, G to I). The opposite dental compensation may occur in maxillary protrusion or mandibular deficiency (Figure 26-9). Again, the decompensation is aimed at improving angulation of teeth over underlying bone, after which skeletal problems are corrected.
The essential steps in orthodontic preparation are to align the arches individually, achieve compatibility of the arches or arch segments, and establish the proper anteroposterior and vertical position of the incisors. The amount of presurgical orthodontics can vary, ranging from appliance placement with minimal tooth movement in some patients to approximately 12 to 18 months of appliance therapy in those with severe crowding and incisor malposition.
As the patient is approaching the end of orthodontic preparation for surgery, it is helpful to take impressions and evaluate progress models for occlusal compatibility. Minor interferences that exist can be corrected easily with arch wire adjustment and significantly enhance the postsurgical occlusal result. After any final orthodontic adjustments have been made, large stabilizing arch wires are inserted into the brackets, which provide the strength necessary to withstand the forces resulting from intermaxillary fixation (IMF) and surgical manipulation.
Final Treatment Planning
After the completion of the presurgical periodontics, restorative dentistry, and orthodontics, the patient returns to the oral-maxillofacial surgeon for final presurgical planning. The evaluation completed at the initial patient examination is repeated. The patient’s facial structure and the malocclusion are re-examined. Presurgical digital photographs and conventional radiographs or CT scans are obtained in preparation for developing the final surgical plan.
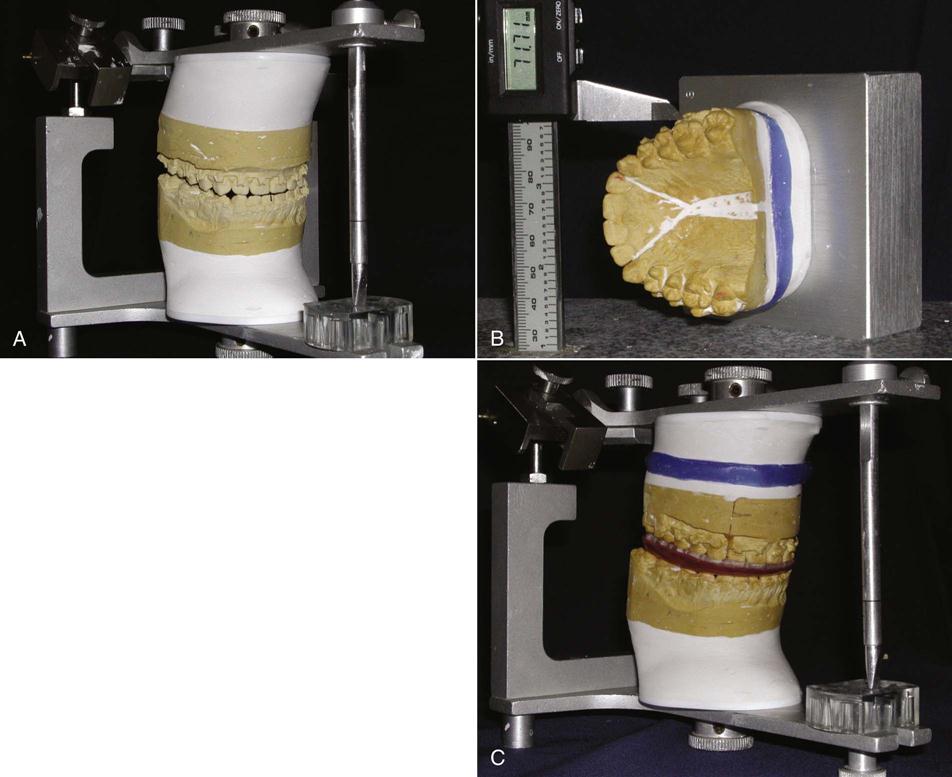
Conventional treatment planning and image prediction.
When using a traditional model surgery planning technique, presurgical models, a centric relation bite registration, and face-bow recording for model mounting are completed. Model surgery on a duplicated set of presurgical dental casts determines the exact surgical movements necessary to accomplish the desired postoperative occlusion (Figure 26-10).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses