CHAPTER 26 Antianginal Drugs
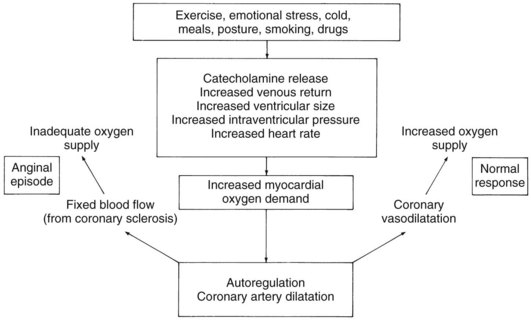
As shown in Figure 26-1, the normal response to increased myocardial oxygen demand is satisfied by vasodilation of the small coronary resistance vessels, increased blood flow, and increased oxygen supply. In contrast, in the classic anginal patient with exertional (exercise-induced) episodes, significant sclerosis (>70% narrowing of the luminal diameter) of the large conductance arteries precludes increased vasodilation in response to increased myocardial work because the poststenotic resistance vessels are already dilated, and the resultant demand for oxygen cannot be met. Cardiac determinants of oxygen consumption and factors that can precipitate changes in these determinants are also shown in Figure 26-1.
There are three types of angina pectoris: chronic stable angina (classic exertional angina), variant (Prinzmetal’s) angina, and unstable angina (also known as preinfarction angina, intermediate coronary syndrome, acute coronary insufficiency, and accelerated angina). Chronic stable angina occurs in patients who have fixed atherosclerotic coronary artery disease. Pain in these individuals occurs when the myocardial oxygen requirement reaches a given stable value. Variant angina occurs as a result of coronary artery spasm and a subsequent decrease in coronary blood flow and oxygen supply. These patients usually also exhibit coronary atherosclerosis, although it may be minimal in some. Variant angina is characterized by chest pain occurring at rest and, frequently, during sleep. The third type, unstable angina, refers to a new onset of severe, frequent angina, anginal pain at rest, or a sudden worsening of pain in a patient with previously stable exertional angina.18 The cause of unstable angina is often sudden platelet aggregation or plaque emboli in coronary vessels. Most of these patients have severe coronary artery disease; coronary spasm may also be involved. Of patients with chest pain, 30% have unstable angina, and it was estimated that 20% of these patients will have a myocardial infarct within a year and most within a month.11 More recent studies suggest that compared with conservative management, early invasive treatment of patients with unstable angina using coronary angiography with or without revascularization reduces mortality and myocardial infarction at 2 and 5 years.10
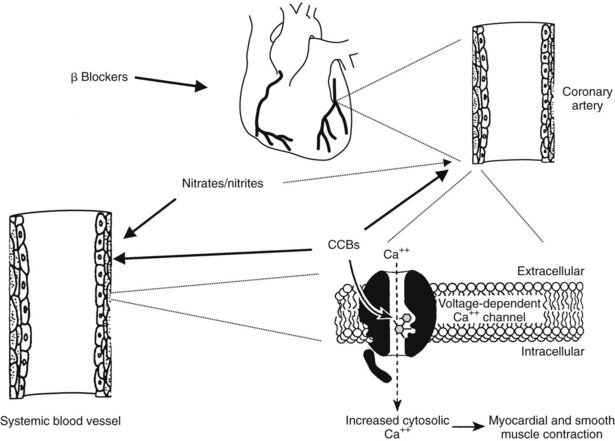
Six classes of drugs are used extensively in the treatment of angina pectoris; Figure 26-2 shows the sites of action of β-adrenergic receptor blockers, Ca++ channel blockers (CCBs), and nitrates/nitrites. The first class, organic nitrites and nitrates, comprises drugs (e.g., sublingual nitroglycerin) that provide immediate relief from anginal symptoms or provide prophylaxis of an attack and nitrate formulations (e.g., topical nitroglycerin, oral isosorbide dinitrate) that are promoted for long-term protection from anginal episodes.
The fourth class of drugs targets blood-clotting mechanisms and comprises aspirin, other antiplatelet drugs, and anticoagulants. Aspirin is used to treat stable and unstable angina. The pharmacologic features of aspirin are discussed in detail in Chapter 21. It acts by inhibiting platelet aggregation through irreversible inhibition of cyclooxygenase.
The fifth class is represented by ranolazine, which was approved by the U.S. Food and Drug Administration in 2006 for the treatment of chronic angina in patients who have failed to respond to other angina therapy. The sixth class is represented by trimetazidine, a novel anti-ischemic drug with properties unrelated to changes in myocardial oxygen supply/demand ratio.3 Trimetazidine is considered to be a metabolic agent that modifies substrate use in chronic heart failure.1 This drug can lessen oxidation of free fatty acids via inhibition of the enzyme long-chain 3-ketoacyl coenzyme A thiolase, which is crucial in the β-oxidation pathway. Trimetazidine has a favorable side-effect profile and exhibits no notable vasodilator properties at rest or during dynamic exercise.15 It is not discussed further.
NITRITES AND NITRATES
Amyl nitrite was introduced for use in angina pectoris in 1867, and nitroglycerin (glyceryl trinitrate) was introduced in 1879. Since then, nitroglycerin has remained the drug of choice for the relief of acute symptoms of angina pectoris. Nitroglycerin is administered sublingually as a tablet or aerosol spray and has a quick onset and short duration of action. Various organic nitrates and sustained-release forms of nitroglycerin have been developed in attempts to find a suitable, long-lasting preparation for the control and prevention of anginal pain. Amyl nitrite is used by inhalation for angina pectoris. Its use in the treatment of cyanide poisoning is discussed in Chapter 52.
Chemistry
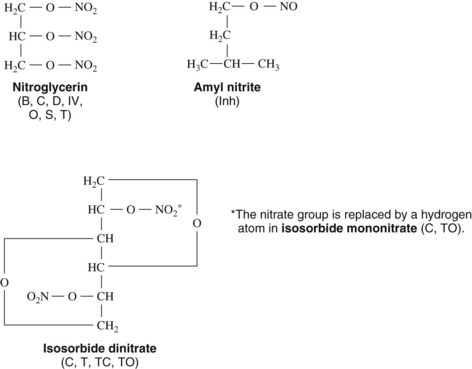
Nitroglycerin is chemically a simple compound. Figure 26-3 shows its structure and, for comparison, the structures of some of the other organic nitrates marketed for oral, topical, sublingual, buccal, inhalant, or intravenous administration. All nitrites and nitrates with antianginal activity are esters of nitrous or nitric acid. Organic nitrites and nitrates are capable of being metabolized to yield the free radical nitric oxide (NO). Research in this area led to the Nobel Prize for Physiology/Medicine being awarded in 1998 to Robert Furchgott, Louis Ignarro, and Ferid Murad for their discovery of NO as a signaling molecule in the cardiovascular system. Previous studies had identified a vasodilator substance released from endothelial cells and referred to as endothelium-derived relaxing factor. Experimental evidence from several laboratories indicates that endothelium-derived relaxing factor is NO.12 NO is the active intermediate of vasoactive nitrites and nitrates, which are appropriately referred to collectively as nitrovasodilators. (See Figure 8-3 for further information on NO.)
Pharmacologic Effects
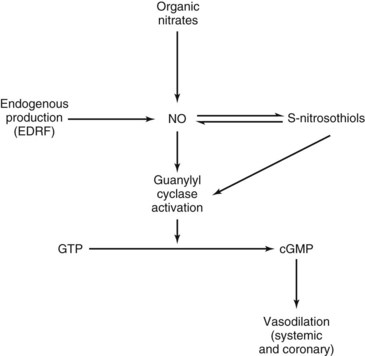
The pharmacologic effects of all the members of this class are similar and result from actions of NO released by denitration reactions of the parent drugs in the tissues. It is likely that mitochondrial aldehyde dehydrogenase plays an essential role in the synthesis of NO from nitroglycerin bioactivation, resulting in dilation of blood vessels.6 NO has been shown to stimulate the synthesis of cyclic 3′,5′-guanosine monophosphate (cGMP) by a direct action on cytosolic guanylyl cyclase or indirectly by being converted to S-nitrosothiols, which stimulate the enzyme (Figure 26-4; see also Figure 8-3). cGMP initiates a cascade of reactions involving cGMP-dependent protein kinases leading to the various cellular responses that relax vascular smooth muscle.
Long-Acting Drugs
Although sublingual nitroglycerin is highly effective for the treatment of acute anginal episodes, its short duration of action makes it unsuitable for long-term prophylaxis. Several nitrates formulated for oral administration have been marketed for many years for the prevention of anginal attacks. The vasodilatory effects of isosorbide dinitrate were discovered in the 1930s, and the drug was introduced in the 1960s as an oral preparation. When administered sublingually, isosorbide dinitrate (see Figure 26-3) was shown to be comparable to nitroglycerin. When administered orally in recommended dosages, this compound offered no protection against exercise-induced angina. Subsequent investigations showed, however, that large doses of isosorbide dinitrate (and nitroglycerin) improve exercise tolerance in patients with angina. There is a concomitantly increased possibility of drug toxicity.
Newer long-acting mononitrates, which are major active metabolites of isosorbide dinitrate, offer the advantage of improved bioavailability because they avoid first-pass hepatic elimination. Isosorbide-5-mononitrate, which is at least as effective as isosorbide dinitrate, is available as immediate-release tablets and as a sustained-release formulation for once-daily administration. The clinical efficacy of a single dose of isosorbide mononitrate formulated as a 30% immediate-release/70% sustained-release formulation is observed within a few minutes to increase work and exercise capacity.2 More recent evidence indicates that nitrates reduce platelet aggregation and adhesion in patients with acute myocardial infarction. This finding suggests a possible added benefit of nitrates.9
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses