24
The temporomandibular joints, muscles of mastication, and the infratemporal and pterygopalatine fossae
Chapter contents
24.1 Introduction
It is essential that dental students and practitioners understand the structure and function of the temporomandibular joints and the muscles of mastication and other muscle groups that move them. The infratemporal fossa and pterygopalatine fossa are deep to the mandible and its related muscles; many of the nerves and blood vessels supplying the structures of the mouth run through or close to these areas, therefore, knowledge of the anatomy of these regions and their contents is essential for understanding the dental region.
24.2 The temporomandibular joints
The temporomandibular joints (TMJ) are the only freely movable articulations in the skull together with the joints between the ossicles of the middle ear; they are all synovial joints. The muscles of mastication move the TMJ and the suprahyoid and infrahyoid muscles also play a significant role in jaw movements.
24.2.1 Articular surfaces
The articular surfaces of the squamous temporal bone and of the condylar head (condyle) of the mandible form each temporomandibular joint. These surfaces have been briefly described in Chapter 22 on the skull and Figure 24.1A indicates their shape. The concave mandibular fossa is the posterior articulating surface of each squamous temporal bone and houses the mandibular condyle at rest. The condyle is translated forwards on to the convex articular eminence anterior to the mandibular fossa during jaw movements.
The articular surfaces of temporomandibular joints are atypical; they covered by fibrocartilage (mostly collagen with some chondrocytes) instead of hyaline cartilage found in most other synovial joints.
24.2.2. Capsule and ligaments
Figures 24.1B and 24.1C show the capsule and ligaments associated with the TMJ. The tough, fibrous capsule is attached above to the anterior lip of the squamotympanic fissure and to the squamous bone around the margin of the upper articular surface and below to the neck of the mandible a short distance below the limit of the lower articular surface. The capsule is slack between the articular disc (see Section 24.2.3) and the squamous bone, but much tighter between the disc and the neck of the mandible. Part of the lateral pterygoid muscle is inserted into the anterior surface of the capsule. As in other synovial joints, the non-load-bearing internal surfaces of the joint are covered with synovial membrane.
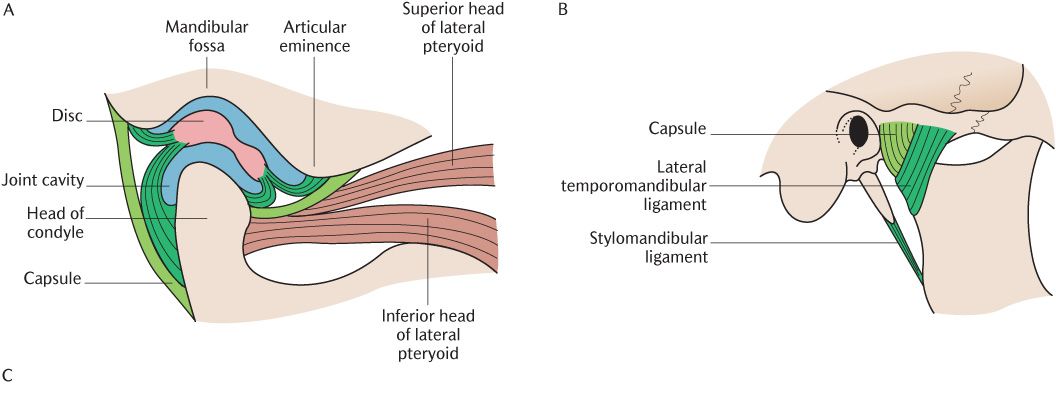
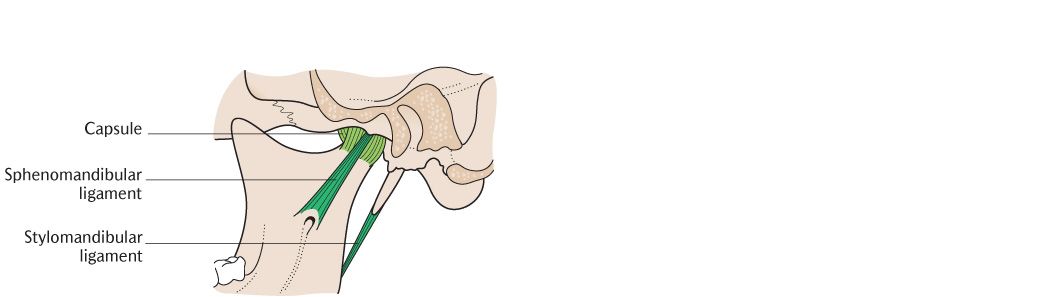
Fig. 24.1 The right temporomandibular joint. A) In sagittal section to show its internal structure; B) Lateral view; C) Medial view.
As illustrated in Figure 24.1B, the capsule is strengthened laterally by the lateral temporomandibular ligament, a thick band of fibrous tissue; it extends obliquely downwards and backwards from the articular tubercle to the lateral surface of the mandibular neck to prevent excess posterior movement of the TMJ.
There are two accessory ligaments of the TMJ which do not blend with or strengthen the capsule. As shown in Figure 24.1C, the sphenomandibular ligaments extend downwards and forwards from the spine of the sphenoid to the lingula of the mandible and are some distance medial to the joint. They act as a sling for the mandible and it rotates about an axis passing through the lower attachments of the ligaments during some mandibular movements. The stylomandibular ligaments extend from the styloid process to the angle of the mandible behind each joint; these are thickenings of the parotid capsule rather than true ligaments.
Recall from Section 2.4.1 that the capsule and ligaments of synovial joints have an important sensory role; they contain proprioceptive nerve endings and provide information on joint position—absolutely vital for the function of the TMJ. The sensory nerves are supplied from the auriculotemporal and masseteric nerves, both branches of the mandibular division of the trigeminal nerve (see Section 24.5.1).
24.2.3 The articular disc
As you can see in Figure 24.1A, the joint cavity of each TMJ is completely divided into an upper and lower compartment by the articular disc (or meniscus). The joint cavity is not divided in other synovial joints. The disc is made of dense fibrous tissue and is essentially a continuation of the tendon of attachment of the lateral pterygoid muscle through the joint cavity.
The disc blends laterally and medially with the capsule of the joint. As Figure 24.1A shows, it is attached in front to the anterior border of the squamous articular surface and the capsule. The disc divides into two layers posteriorly. The upper layer is attached to the anterior margin of the squamotympanic fissure while the lower layer is attached to the posterior surface of the neck of the mandible. The capsule on the posterior aspect of the joint blends with these two layers. The tendon of the lateral pterygoid muscle is inserted into the anterior margin of the disc.
Figure 24.1A shows that the disc is not uniform in thickness. The posterior part of the disc is thickest, the central part is thinnest and the front part of the disc is also thickened although not as much as the posterior part. Occasionally, the disc is perforated in the central thin region and the two compartments are then in communication. This makes no difference to joint function.
The functions of the articular disc are uncertain because surgical removal of the disc from patients with arthritic TMJs improves rather than impedes function. The disc seems unnecessary for efficient joint function. The lateral pterygoid muscles protrude the mandible by drawing the mandibular condyles forwards from the mandibular fossa to the articular eminence (see Section 24.3.3). They also draw the disc forwards wedging the thick posterior portion between the back of the condyle and articular eminence and may stabilize the joint as the mouth is opened.
The TMJ may be dislocated. The causes and consequences are described in Box 24.2.
24.3 The muscles of mastication
The muscles of mastication comprise four pairs of muscles. The temporalis and masseter muscles are superficial to the mandible whereas the medial and lateral pterygoid muscles are deep to it.
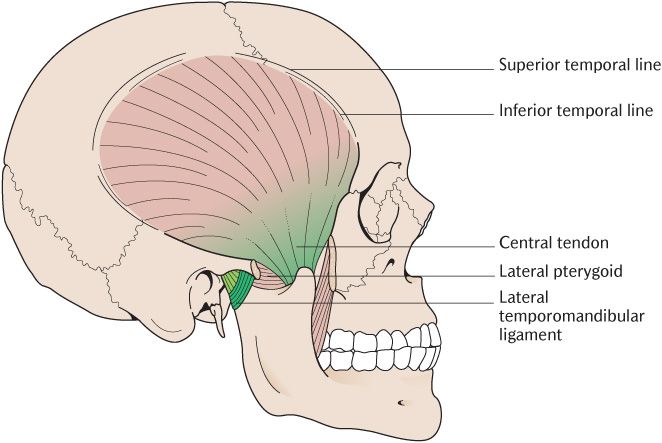
24.3.1 The temporalis muscle and temporal fascia
As shown in Figure 24.2, each temporalis muscle arises from an area on the external surface of the cranial vault between the inferior temporal line and the infratemporal crest below although the crest is hidden by the muscle in the figure. The muscle fibres converge from this wide area towards the coronoid process of the mandible. As Figure 24.2 illustrates, the anterior fibres run downwards and slightly backwards, the middle fibres pass directly downwards and the posterior fibres thus run downwards and forwards with the most posterior fibres running almost horizontally. The fibres attach to a well-developed tendon, passing deep to the zygomatic arch near the coronoid process. The tendon attaches to the apex, anterior, posterior borders, and medial aspect of the coronoid process; the attachment continues below the coronoid process down the anterior border of the ramus as far down as the retromolar fossa posterior to the mandibular third molar. The extent of this attachment must be taken into consideration during the design of lower dentures as described in Box 24.1. The fibres arising close to the infratemporal crest have a fleshy attachment into the medial surface of the coronoid process and ramus.
The temporal fascia, a strong sheet of fibrous tissue, covers the temporalis muscle. It is attached above to the whole length of the superior temporal line. Inferiorly, it splits to attach to the external and medial margins of the upper border of the zygomatic arch. The superficial temporal blood vessels and the auriculotemporal nerve cross the fascia superficially.
The temporalis is supplied by the deep temporal nerves from the anterior division of the mandibular nerve. Its principal action is elevation of the mandible to close the mouth. The disposition of the fibres within the muscle mean that some fibres are always aligned for the most efficient mechanical advantage irrespective of the position of the TMJ. The more horizontal posterior fibres retract the mandible.
Fig. 24.2 The temporalis muscle.
Box 24.1 The attachments of temporalis and prosthetic dentistry
The attachment of the temporalis tendon into the retromolar fossa can be verified on yourself. Push your finger along between your teeth and cheek and feel the anterior border of the mandibular ramus. Now clench your teeth and you can feel the tendon. Note how far it does come down into the fossa.
This relationship is clinically important when designing dentures. If the base of a lower denture is extended too far backwards, the tendon can displace the denture when temporalis contracts or oral mucosa is trapped between the denture base and the muscle causing soreness and discomfort. Avoidance of these potential problems is implicit in denture construction; prosthetic teeth tend to be smaller than the corresponding living teeth and only seven teeth are incorporated into a full lower denture, thus the denture does not have to be extended so far back that it will impinge on the temporalis attachment.
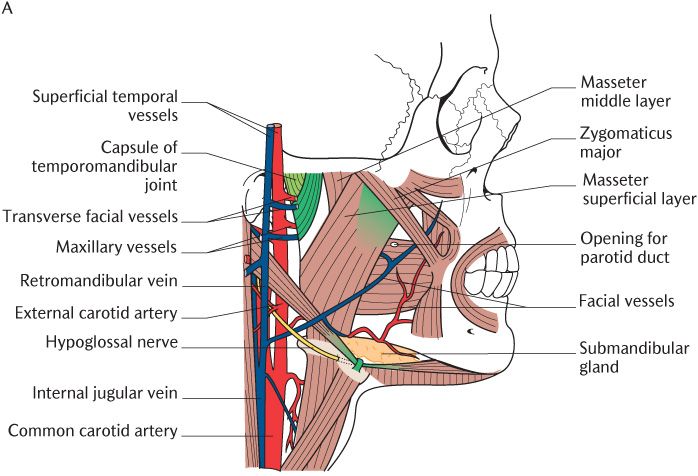
24.3.2 The masseter muscles
As illustrated in Figure 24.3A, each masseter muscle attaches between the zygomatic arch above and the outer surface of the angle of the mandible below. Take a closer look at Figure 24.3A and a dissected specimen if you have access and you will see that the superficial layer, the largest component of the muscle, conforms to this description. It arises from a strong aponeurosis attached to the anterior two-thirds of the lower border of the zygomatic arch and pass downwards and backwards to the angle of the mandible. You will also see more vertical fibres deep to the superficial layer. This is the middle layer attached above between the medial surface of the anterior two-thirds and the lower border of the posterior one-third of the arch and to the lateral surface of the middle part of the ramus below. The deep layer arises from the whole length of the medial surface of the zygomatic arch and its fibres pass downwards to attach to the upper part of the mandibular ramus. As shown in Figure 24.3B, these three layers are quite distinct and separable posteriorly, but anteriorly, they fuse to form a single mass. The three layers of muscle provide fibres running in the line of best mechanical advantage for any position of the TMJ.
There are several tendinous septa within the masseter muscle; some are attached to the zygomatic arch and interdigitate with others attached to the lateral surface of the mandible. The muscle fibres run between these septa in a multipennate arrangement (see Section 2.5.1 and Figure 2.5), making the masseter muscles extremely powerful elevators of the mandible. They are innervated by the masseteric branches of the anterior division of the mandibular nerve. As shown in Figure 24.3B, the masseteric branch of the transverse facial artery runs between the middle and superficial layers and provides the principal blood supply to the muscles.
24.3.3 The pterygoid muscles
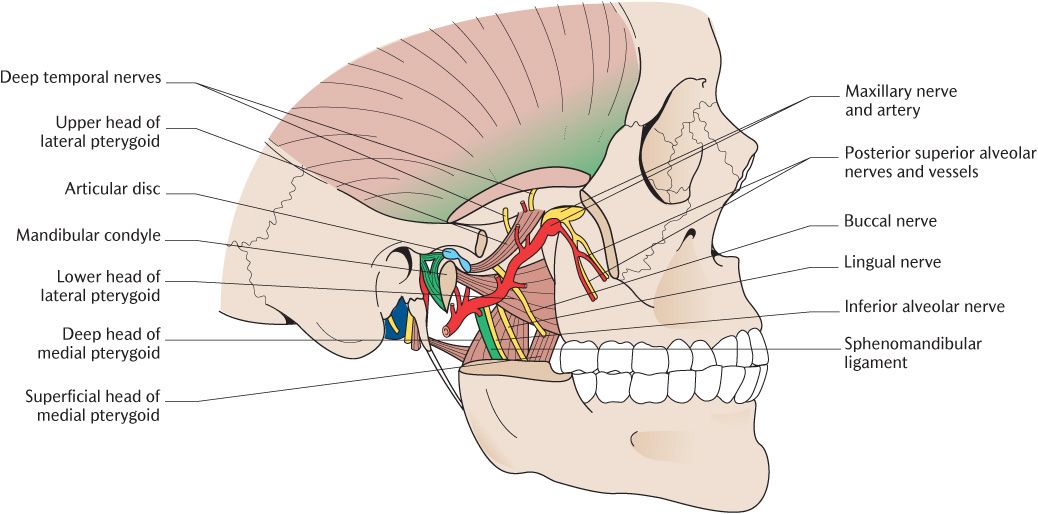
The lateral and medial pterygoid muscles are the two deep pairs of the muscles of mastication. The lateral and medial pterygoid muscles, the two deep muscles of the muscles of mastication, attach to the lateral and medial sides of the lateral pterygoid plates, respectively. The pterygoid plates are part of the pterygoid processes of the sphenoid bone in the cranial base but they function as a component of the upper facial skeleton.
The lateral pterygoid muscles
As you can see in Figure 24.4, each lateral pterygoid muscle arises by two heads. The upper head is attached to the infratemporal surface of the greater wing of the sphenoid and the lower head to the lateral surface of the lateral pterygoid plate. The fibres run backwards and laterally. The larger lower head of the muscle is attached by a short tendon into the pterygoid fovea on the anterior surface of the neck of the mandible. The smaller upper head is attached to the anterior aspect of the capsule and hence into the articular disc of the TMJ. The two parts of the muscle pull the head of the mandible and the disc forwards, respectively. There is good electrophysiological evidence that the two parts of the muscle act independently during movements of the mandible; these movements and the part played by the lateral pterygoids is described in Section 24.4. The muscle is innervated by a branch of the anterior trunk of the mandibular division of the trigeminal nerve.
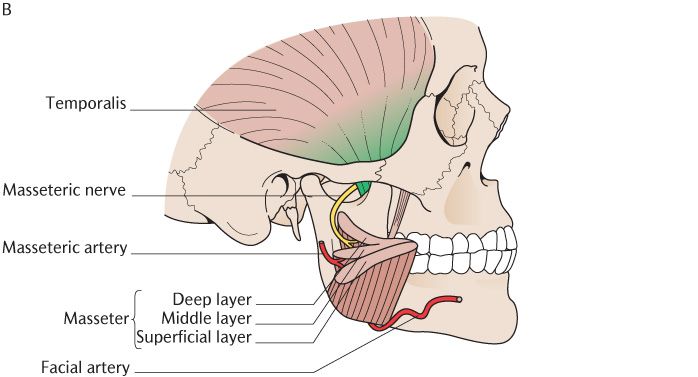
Fig. 24.3 A) The masseter muscle and related structures. The parotid gland has been removed for clarity. B) The three layers of the masseter muscle and its nerve and blood supply.
The medial pterygoid muscles
As shown in Figure 24.4, each medial pterygoid muscle also arises by two heads. Most of its fibres arise from the medial surface of the lateral pterygoid plate; a small slip arises from the maxillary tuberosity and adjacent palatine bone to form the superficial head. The fibres run downwards, backwards, and laterally to insert into the roughened area on the medial surface of the ramus and angle of the mandible. Each medial pterygoid muscle contains a number of tendinous septa which give it a multipennate arrangement like the masseter muscle. The medial pterygoid muscle is a powerful elevator of the mandible; its role in mandibular movements is described in Section 24.4. The muscle is innervated by a branch from the main trunk of the mandibular trigeminal nerve.
The pterygomandibular space is a gap between the muscle attachment to the angle and the medial surface of the ramus above. This is the area in which inferior alveolar nerve blocks are placed for local anaesthesia of the lower teeth. The anatomy of local anaesthesia is described in Section 25.5.2.
24.4 Movements of the TMJ
A unique feature of the TMJ is that the left and right joints are joined by the very robust mandible; one joint, therefore, cannot be moved in isolation so there must be compensatory movement in the other joint. For instance, if you wish to deviate your mandible to one side so that the cusps of the posterior teeth can grind food as you chew, you will slide the condyle of the opposite side forwards using the lateral pterygoid muscle while holding back the other side back with the horizontal fibres of temporalis. Move your mandible to the left while palpating both joints. You will feel the right joint sliding forward and at the same time, the left joint making a slight backward movement to compensate. Both TMJs must make movements simultaneously because they cannot operate independently; however the movements do not have to be identical in both joints.
Fig. 24.4 The pterygoid muscles and other contents of the right infratemporal fossa. The ramus of the mandible has been removed at a level just above the mandibular foramen.
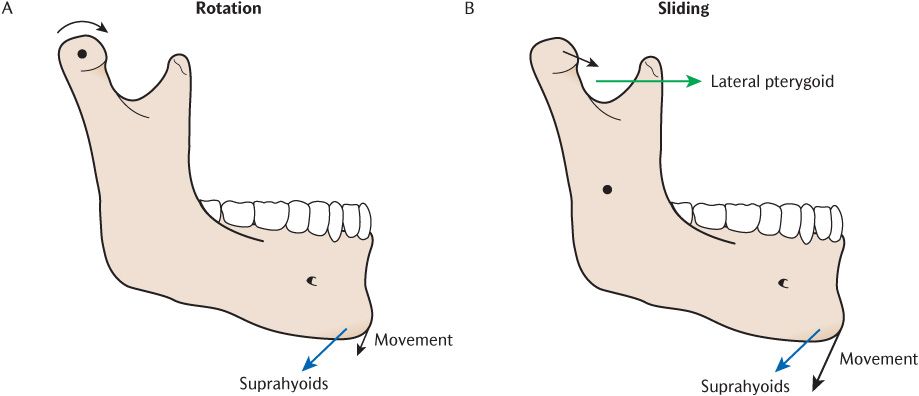
Each TMJ can rotate about an axis through the head of the condyle and can slide anteriorly from the mandibular fossa on to the articular eminence. Rotation alone produces relatively little opening movement. You can verify this by palpating your own joints as you open your mouth gradually; after the mandible has lowered a few millimetres, you will feel the forward sliding movements as you open wider. It is possible to slide the TMJ forwards (protrusion) without rotation but your teeth must be slightly apart otherwise the cusps interfere with jaw movement. In reality, sliding and rotator movements occur simultaneously. Reversing the direction of sliding will retract the jaw and rotating in the opposite direction will close the jaw.
The only possible movements at the joints are:
• Rotation of the head of the condyle within the mandibular fossa;
• Sliding of the condyle along the articular eminence.
These are combined in various ways to produce the functional movements of depression, elevation, protrusion, retraction, and lateral deviation of the mandible. They are illustrated in Figure 24.5. The functional movements are, in turn, combined to produce the complex patterns of movements during incision and mastication described in Section 26.3.
It is important to realize that the muscles of mastication are rarely completely relaxed, except when in deep sleep or unconscious. The muscles maintain a low level of activity (muscle tone) to counteract gravity sufficient to keep the mouth closed without the maxillary and mandibular teeth contacting. This is known as the mandibular rest position or postural position. Feel the space between the upper and lower teeth by running your tongue around your teeth; the 2–3 mm gap between them is the interocclusal (or freeway) space. Occlusion is the jaw position when the upper and lower teeth are in maximal contact. Most movements of the mandible start from the rest position rather than occlusion.
24.4.1 Basic movements
Figure 24.5A illustrates rotational movement of the head of the condyle about a transverse axis. This transverse axis of rotation does not coincide exactly with the long axis of the condylar head since the latter is angled posteromedially from the transverse plane (see Figure 22.13). The outcome of rotational movement is the depression of the mandible, but as already described, the mouth can only open a little without any sliding movement. If you attempt to depress the mandible by rotation alone, you will find that you can open your mouth only a short distance. The posterior border of the mandibular ramus soon impinges on the parotid gland behind it and further movement is impossible once because of its resistance to compression. Continued opening past this point requires that the mandibular head to translate forwards on to the articular tubercle.
The sliding movement is shown in Figure 24.5; the mandibular head and disc slide together forwards and downwards from the mandibular fossa on to the articular eminence. Verify this for yourself by palpating the lateral poles of the mandibular heads whilst depressing the mandible to its full extent; note how soon the rotational movement is also accompanied by sliding. During sliding, the axis of rotation of the mandible moves downwards from the condylar heads to a position approximately between the right and left mandibular foramina as shown in Figure 24.5. The steepness of the anterior surface of the mandibular fossa determines how soon the intercuspation of teeth in occlusion is released. In prosthetics, this is the condylar guidance angle. Sliding movements are not naturally used in isolation, except in specific circumstances such as recording the guidance angle during denture construction.
Fig. 24.5 Movement during depression of the mandible. A) Rotational movement; B) Sliding movement. The axis of rot/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses