Periodontal Problems in Children and Adolescents
Gingivitis
Gingivitis is characterized by inflammation of the gingival tissues with no loss of attachment or bone. It occurs in response to the bacteria that live in biofilms at the gingival margin and in the sulcus.1 The clinical signs of gingivitis include erythema, bleeding on probing, and edema. In the early primary dentition, gingivitis is uncommon. Younger children have less plaque than adults do and appear to be less reactive to the same amount of plaque. This can be explained both by differences in bacterial composition of plaque and by developmental changes in the inflammatory response. Gingivitis occurs in half the population by the age of 4 or 5 years, and the incidence continues to increase with age. The prevalence of gingivitis peaks at close to 100% at puberty, but after puberty it declines slightly and stays constant into adulthood.2 Some children exhibit severe gingivitis at puberty, as shown in Figure 24-1. Puberty-associated gingivitis is related to increases in steroid hormones.3 The gingiva may be enlarged with granulomatous changes similar to those occurring in pregnancy. The peak prevalence of puberty-associated gingivitis is at age 10 years in girls and age 13 years in boys.
Certain local factors may be important contributors to gingivitis in children. Crowded teeth and orthodontic appliances may make oral hygiene more difficult and predispose to gingivitis. Mouth breathing may cause chronically dehydrated gingiva in the maxillary labial area and lead to a characteristic localized gingivitis as shown in Figure 24-2. Inflammation, especially erythema, often occurs around erupting primary and permanent teeth.
Gingival Enlargement
Chronic Inflammatory Gingival Enlargement
Long-standing gingivitis in young patients sometimes results in chronic inflammatory gingival enlargement, which may be localized or generalized. It commonly occurs when plaque is allowed to accumulate around orthodontic appliances as shown in Figure 24-3 or in areas chronically dried by mouth breathing. The interdental papillae and the marginal gingiva become enlarged, and the tissue is usually erythematous and bleeds easily. It may be soft and friable with a smooth, shiny surface (see Figure 24-3, A), or dense and fibrotic with a matted surface (see Figure 24-3, B). Inflammatory gingival enlargement often slowly resolves when adequate plaque control is instituted, unless the tissues are fibrotic; in such cases gingivectomy is often required.
Drug-Induced Gingival Enlargement
Long-term therapy with certain systemic medications can produce an overgrowth of gingival tissue (Figure 24-4).4 It can occur after therapy with the anticonvulsant phenytoin (Dilantin), the immunosuppressant cyclosporine, or a calcium channel blocker. Cyclosporine is used to control host rejection of transplanted organs and to manage autoimmune diseases. Calcium channel blockers such as nifedipine and nitrendipine are cardiac drugs that are sometimes prescribed for children to control hypertension. The overgrowth is painless and differs from chronic inflammatory enlargement in that it is fibrous, firm, and pale pink, often with little tendency to bleed. The enlargement occurs first in the interdental region and may appear lobular. It gradually spreads to the gingival margin. The condition can become extreme, sometimes covering the crowns of the teeth and interfering with eruption or occlusion.
Anatomic Problems
Development and Defects of the Attached Gingiva
When teeth erupt they pierce through an existing band of keratinized gingiva, and the width of this band and its relationship to the teeth change very little during subsequent growth and development. Deflections in the path of eruption, such as those due to crowding or overretention of primary teeth, may result in a narrowed band of attached gingiva.5 This is particularly common when mandibular incisors erupt labial to the alveolar ridge as shown in Figure 24-5. If the band of attached gingiva is very narrow, even a small subsequent loss of attachment can result in a mucogingival defect (which occurs when the pocket depth exceeds the width of keratinized gingiva), and recession may occur as shown in Figure 24-5 (left central incisor). The gingival architecture often makes labially erupted teeth difficult to clean, particularly once recession has occurred, leaving them even more vulnerable to inflammation and further attachment loss. The loss of attachment and recession that occurs with a labially malpositioned tooth is sometimes called stripping. Other factors that may contribute to recession in children and adolescents are habit-related self-inflicted injury and the use of smokeless tobacco.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


 Outline
Outline
 FIGURE 24-1
FIGURE 24-1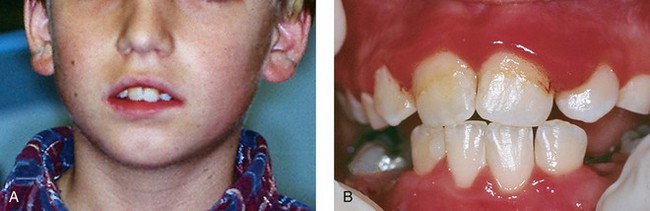
 FIGURE 24-2
FIGURE 24-2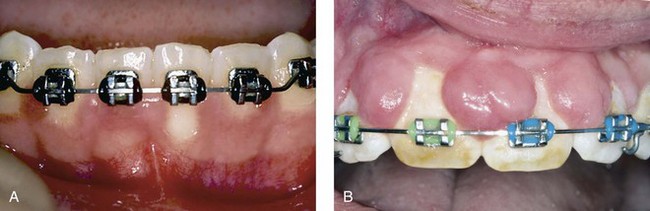
 FIGURE 24-3
FIGURE 24-3
 FIGURE 24-4
FIGURE 24-4