Oral Mucous Membrane
• To name the three categories of mucosa and discuss where they are found
• To name the three stages of keratinization of oral mucous membrane and discuss where these different types are found
• To discuss the factors that affect the mobility of various types of mucosa
• To understand what the submucosa is and where it is found
• To describe the typical clinical picture of normal gingiva
• To describe some of the changes that are seen in diseased gingiva
DIVISIONS OF MUCOUS MEMBRANE
1. Specialized mucosa—mucosa on the upper surface or dorsum of the tongue (discussed in detail in Chapter 24)
2. Masticatory mucosa—comprises the gingiva and hard palatal tissue; undergoes trauma or compression during mastication
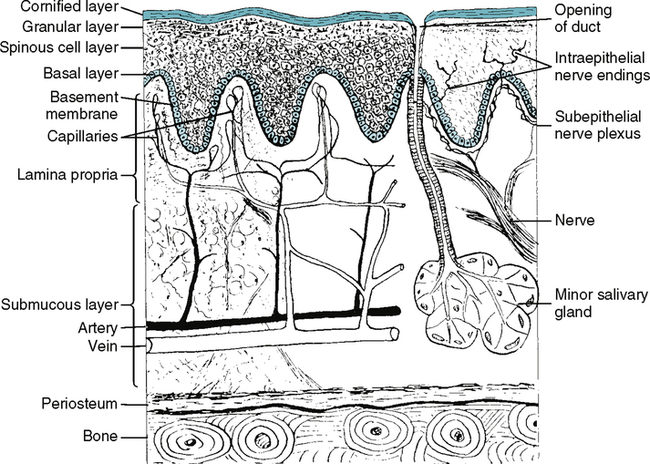
Mucous membrane is composed of stratified squamous epithelium and connective tissue. Stratified squamous epithelium can have various characteristics on its surface (Fig. 23-1) depending on whether it is keratinized, parakeratinized or nonkeratinized.
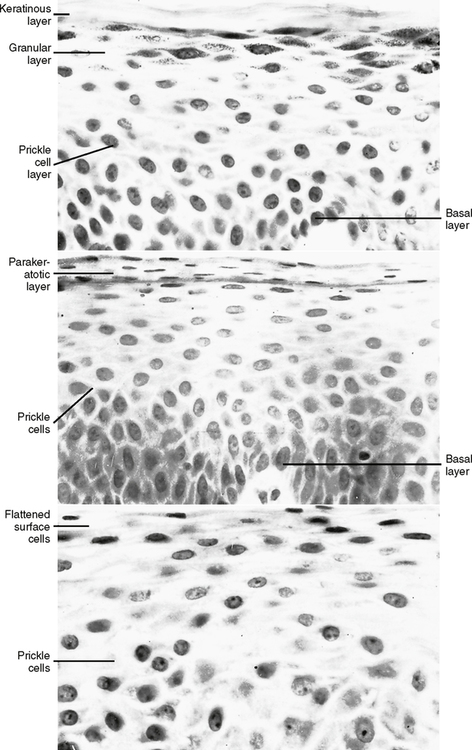
1. Keratinized—On its surface are layers of dead cells without nuclei. This layer is generally called the stratum corneum. The stratum granulosum layer beneath the corneum is relatively evident at this stage of keratinization. As keratinization increases, there tends to be an increase in the thickness of the stratum spinosum as well.
2. Parakeratinized—On its surface are some dead cells without nuclei and some apparently dying cells with slightly shriveled nuclei. The stratum granulosum is not quite as evident as in the keratinized mucosa.
3. Nonkeratinized—Cells on the surface all tend to have nuclei that appear fairly healthy and normal. The stratum granulosum is missing in this type of mucosa.
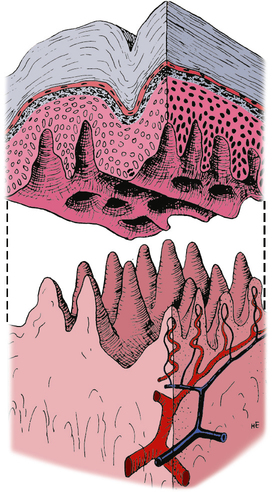
As seen in Fig. 23-2, there is a definite interdigitation between the epithelium and the connective tissue. In this illustration the ridges appear to interdigitate between the two; however, looking at a three-dimensional representation (Fig. 23-3), you can see that there are not only ridges of connective tissue but also pegs of connective tissue projecting up into the epithelium. The length of these ridges and connective tissue pegs determines how tightly the epithelium attaches to the underlying connective tissue and therefore how movable the epithelium is. The connective tissue is attached to underlying bone in some areas or to fatty or muscle tissue in other areas.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses