Management of Human and Animal Bites
Incidence of Bites
Human Bites
Human bites are the third most common bite injuries following dog and cat bites; it is likely that 50% of the U.S. population will have been bitten by a human or animal during their lifetime.1–3 It has been estimated that as many as 150,000 human bites of humans occur annually but go unreported.4 This estimate includes bites to the hand that occur when an assailant punches a victim in the teeth. The population of human bite victims is usually between 20 and 30 years of age.5 Males are affected more frequently than are females.6–8
Human bite injuries can be found in almost any anatomic location, including the face and head, upper and lower extremities, breasts, lips, cheeks, nose, ears, abdomen and thorax, and genitalia; more than 50% occur to the hands and are clenched fist injuries.4,6,9–12 Human bites are generally inflicted as a result of interpersonal violence and are typically associated with murder or attempted murder, rape, sexual assault, child abuse, burglary, and kidnapping.10 The incidence of human bite infections ranges from 4% of facial injuries to 50% of bites to the hand.5,13–16 Human bites more commonly become infected than dog or cat bites.2,17
Animal Bites
Approximately 4.5 million persons are bitten by animals each year; 15% of these will seek treatment from healthcare providers.1,6,9,18 Many of these wounds go unreported because some injuries may appear innocuous or because of social concerns. The overwhelming offender is the domesticated dog (85% to 90%), followed distantly by the domesticated cat (6% to 8%). In 2001, an estimated 368,245 patients were treated for dog bite–related injuries in hospital emergency departments.19 Wild animals, including skunks, raccoons, bats, foxes, and others, account for less than 6%. Other domesticated animals, including horses, cattle, and sheep, account for less than 3% of these bites. The rate of injury is higher among boys than girls; most victims are between 5 and 14 years of age, but many are younger than 5 years (Table 23-1).20–23
TABLE 23-1
Number, Percentage, and Rate* of Nonfatal Dog Bite–Related Injuries
2001
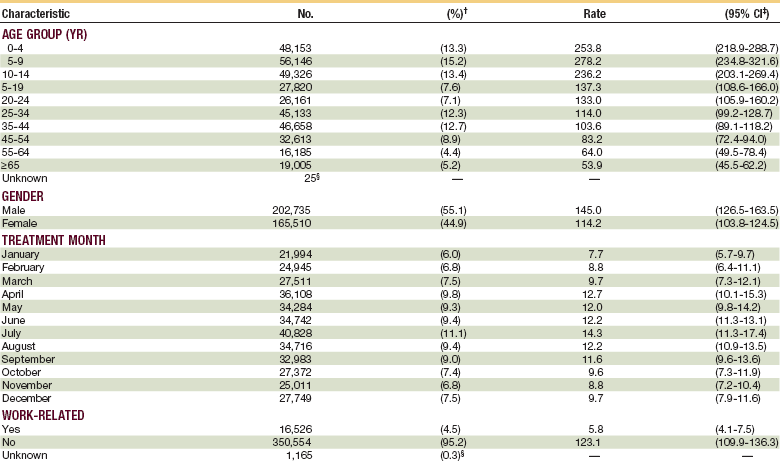
*Per 100,000 population. These bites were treated in U.S. hospital emergency departments, by selected characteristics.
†Numbers might not sum to total because of rounding.
§Estimate might be unstable because the coefficient of variation is >30%.
From Centers for Disease Control and Prevention (CDC): Nonfatal dog bite-related injuries treated in hospital emergency departments—United States, 2001. MMWR Morb Mortal Wkly Rep 52:605–610, 2003.
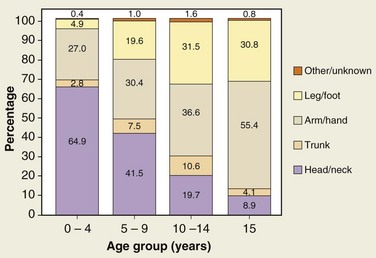
Injury severity scales of children who are admitted to the hospital with dog bite injuries range from 1 to 25, with an average of 4 ± 5; the head and neck area is involved in almost 70% of these injuries.* This is in contrast to adult victims, who suffer only 5% to 15% of animal bites to the head and neck19,26,27 (Fig. 23-1).
As many as 50% of dog bites may be reported as “unprovoked” (a possible indication of rabies infection), and more than 80% of these injuries involved the family’s or a neighbor’s pet.18 Breeds most often involved included pit bulls (25%), golden retrievers (12%), Labrador retrievers (12%), Chow Chows (10%), German shepherds (10%), Rottweilers (10%), and Doberman pinschers (5%) (Table 23-2).
TABLE 23-2
Dog Bite Injuries by Breed of Dog
| Breed | Bite Injuries (% of all Bite Injuries) |
| Pit bulls | 25 |
| Golden retrievers | 12 |
| Labrador retrievers | 12 |
| Chows | 10 |
| German shepherds | 10 |
| Rottweilers | 10 |
| Doberman pinschers | <5 |
Data from Gandhi RR, Liebman MA, Stafford BL, Stafford PW: Dog bite injuries in children: A preliminary survey. Am Surg 65:863–864, 1999.
There were 1164 deaths caused by nonvenomous animals from 1979 through 1990.28 From 1995 to 1996, 279 human deaths occurred as a result of dog attacks.29 During 1997 and 1998, at least 27 dog bite–related fatalities occurred.30 Although some deaths involved hunters who were attacked by large animals, such as bears, most of the deaths were caused by large domesticated dogs, especially Pit bulls, Rottweilers, and German shepherds.23 The most frequent reason for death is exsanguinating hemorrhage. The victims are usually infants (60%) or older individuals.20
Pathophysiology
Human Bites
When humans chew, they generate forces in the range of 1.6 to 26.7 kg.31–34 Maximum molar bite forces range from a low of 1 kg to a high of 443 kg. Although human incisors shear, canines tend to puncture and molars crush. Thus, human bites can penetrate, avulse, and crush the tissue. These injuries are contaminated by a wide range of microorganisms (Box 23-1).*
More than 42 different species of bacteria have been reported in human saliva. Consideration must be given to all normal oral flora and common pathogens in the treatment of these contaminated crush injuries. Although the amount and type of inoculum may be minimal in the case of pristine dentition, they are of significant concern in the neglected mouth. More than 190 species have been isolated when gingivitis or periodontitis is present. The most common bacteria associated with human bite infections include Streptococcus, Staphylococcus aureus, Eikenella, Prevotella, Peptostreptococcus, Fusobacterium, and Candida spp. Immunocompromised patients, alcoholics, and diabetics are at a higher risk for infection by human bites. Other transmissible human diseases that are of concern include herpes, hepatitis B, hepatitis C, tuberculosis, and syphilis.37,38 Acquired immunodeficiency syndrome (AIDS) transmitted by saliva is considered to be of low or no risk, according to the Centers for Disease Control and Prevention (CDC). However, a number of case reports have listed a human bite as the likely event responsible for transmission of AIDS infection and the use of postexposure prophylaxis has been advocated.2,39,40
Animal Bites
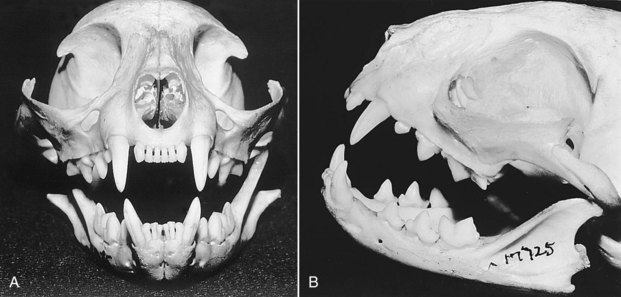
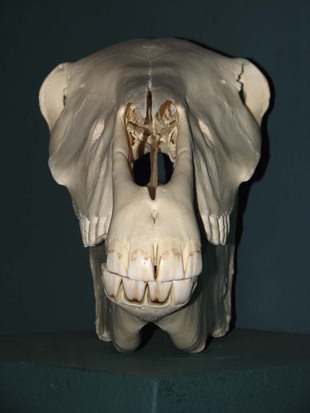
The force delivered by an animal’s jaw when biting can be as high as 1800 psi.41,42 This can result in devitalized tissue caused by crushing, tearing, avulsion, or a combination of all three. Furthermore, these wounds are contaminated by a broad spectrum of microorganisms and can cause a wide range of zoonotic diseases. Sharp, thin, long teeth more frequently cause puncture injuries, as in the case of the domesticated cat6,20 (Fig. 23-2). Shorter, blunter, rounder teeth frequently cause a combination of penetrating and crush injuries, as in the case of the domesticated dog (Fig. 23-3). Flat teeth cause crush and tear injuries, as in the case of the domesticated horse (Fig. 23-4). Animal bites may cause fractures in addition to soft tissue injury, a thorough examination should be performed to prevent missing critical injuries, especially in infants, children, and older adults (Fig. 23-5).
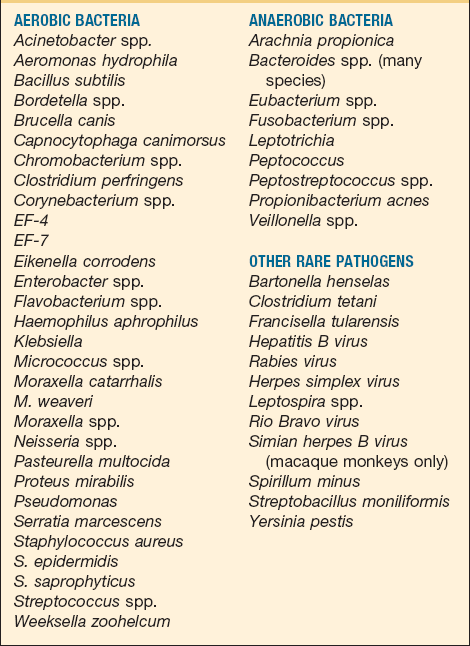
A list of microorganisms from all animal bite sources is presented in Box 23-2.* No species seems to be associated with any particular type of bacterial variant, except that animal bites differ from human bites in the presence of Pasteurella multocida in as many as 50% to 75% of cases of infection. Consistent with the heterogeneity observed between feline and canine oropharyngeal Pasteurella strains, P. canis biotype 1 is the predominant isolate from dog bites, whereas P. multocida subsp. multocida and septica have been isolated much more frequently from cat bites.49
The aerobic bacteria most frequently associated with infected animal bites include alpha- and beta-hemolytic streptococci (24% to 46%), S. aureus and S. epidermidis (10% to 25%), and Escherichia coli, Pseudomonas, and Moraxella spp. (10% to 25%).† The most common anaerobic bacteria isolated from infected animal bites are the Bacteroides, Prevotella, and Fusobacterium spp. (13% to 76%). Oral and environmental fungi may also contaminate bite wounds. Candida spp. have been isolated from 8% of infected human bites, but their pathogenic role remains unclear.51,52
Tetanus
The CDC has stated that 201 cases of tetanus were reported from 1991 to 1994, with an annual incidence rate of 0.02 cases/100,000.53 There was a reported case fatality rate of 25%. Of these injuries, 49% resulted from puncture wounds, 20% from lacerations, and 12% from abrasions. Only 5 patients reported injury by an animal.
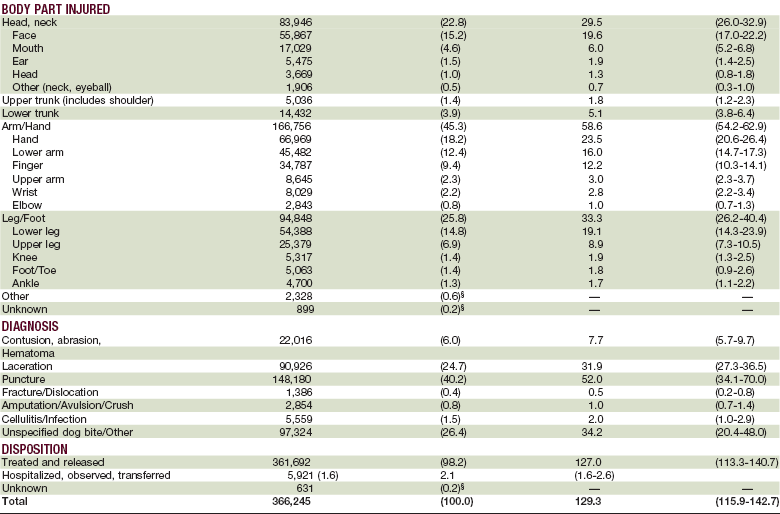
No bite injury should be considered clean or minor. Although the incidence of the tetanus may seem low, the high rate of mortality in patients who contract it makes the treatment of tetanus a priority. If adequate history of immunization cannot be elicited, the patient should be treated according to the Advisory Committee on Immunization Practices (Table 23-3).53
TABLE 23-3
Summary Guide to Tetanus Prophylaxis in Routine Wound Management
*Such as, but not limited to, wounds contaminated with dirt, feces, soil, and saliva, puncture wounds; avulsions, and wounds resulting from missiles, crushing, burns, and frostbite.
†For children < 7 yr old; DTP (DT, if pertussis vaccine is contraindicated) is preferred to tetanus toxoid alone. For those ≥7 yr of age, Td is preferred to tetanus toxoid alone.
‡If only three doses of fluid toxoid have been received, then a fourth dose of toxoid, preferably an adsorbed toxoid, should be given.
§Yes, if >10 yrs since last dose.
¶Yes, if >5 yrs since last dose. (More frequent boosters are not needed and can accentuate side effects.)
Rabies
The incidence of rabies has declined steadily since the 1950s.54 Approximately 36 cases have been reported in the United States since 1990.1,55 Only one case of rabies in a human was reported to the CDC during 2001. This viral disease is most frequently carried in wild animals (especially bats, raccoons, and skunks). Domestic animals accounted for 6.7% of all rabid animals reported in the United States during 2001; these were mainly cats, dogs, and cattle. Vaccination of domestic animals, vaccination programs targeting wildlife, and ongoing educational programs have contributed to the very low incidence of rabies in humans. Approximately 20% of human cases occur in the United States because of exposure abroad. Of the almost 80% of cases that occurred within the United States from 1990 to 2001, 92.3% of infected persons were found to have viral variants associated with bats.
The rabies virus is a bullet-shaped rhabdovirus.56 After entering its new host, it travels to the central nervous system through the peripheral nerves, proliferating in the gray matter. It then spreads centrifugally to the salivary glands, adrenal glands, musculature, and heart. This mechanism accounts for the signs and symptoms associated with the different phases of the rabies infection. There is a long incubation period in rabies, typically lasting 20 to 90 days and rarely exceeding a year or more.57 The prodromal phase usually ranges from 3 days to 3 months, the excitement phase lasts from 3 months to 6 months, and the brainstem dysfunction phase ranges from 6 to 12 months. Symptoms of rabies in animals include an unprovoked attack or bizarre behavior in domestic animals. Signs of infection in humans include symptoms of cerebral dysfunction, anxiety, confusion, and agitation, progressing to delirium, abnormal behavior, hallucinations, and insomnia.
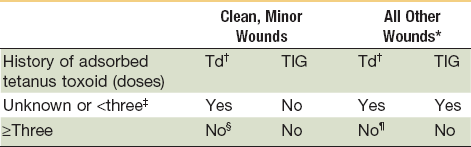
If the bite has been inflicted by a human, chipmunk, guinea pig, gerbil, hamster, squirrel, rat, mouse, rabbit, or horse, there is little to no risk of rabies infection.1,55 If the bite is from a healthy domesticated dog, cat, or ferret, the animal should be confined and observed for 10 days. Any sign of illness prompts sacrifice and testing of the animal and postexposure prophylaxis for the victim. Any bite by a wild animal, such as a raccoon, skunk, fox, or coyote is considered high risk and rabies prophylaxis must be given. Interestingly, bats are the most common source of exposure to rabies in the United States. Currently, postexposure prophylaxis is recommended for anyone with a bite, scratch, or mucous membrane contact with a bat.
For victims at risk for rabies, management must begin immediately (Table 23-4); 20 IU/kg (0.133 mL/kg) of rabies immune globin (RIG) should be administered. Most of the dose should be injected in and around the site of the wound as much as possible, avoiding vascular compromise. The remainder should be given IM.1,58 Rabies vaccine should also be administered in five doses IM on the day of the attack and on days 3, 7, 14, and 28 after the attack.3,7,59 RIG should not be administered to patients who have been previously vaccinated, but they should receive additional vaccine. Three inactivated rabies vaccines are licensed for use in the United States. They are human diploid cell vaccine (HDCV), rabies vaccine absorbed (RVA), and purified chick embryo cell vaccine (PCEC).
TABLE 23-4
Rabies Postexposure Prophylaxis Guide—United States, 2008
| Animal Type | Evaluation and Disposition of Animal | Postexposure Prophylaxis Recommendations |
| Dogs, cats, and ferrets | Healthy and available for 10 days observation. Rabid or suspected rabid. Unknown (e.g., escaped). |
Persons should not begin prophylaxis unless animal develops clinical signs of rabies.* Immediately vaccinate. Consult public health officials. |
| Skunks, raccoons, foxes and most other carnivores; bats | Regarded as rabid unless animal proven negative by laboratory tests.† | Consider immediate vaccination. |
| Livestock, small rodents, Lagomorphs (rabbits and hares), large rodents (woodchucks and beavers), and other mammals | Consider individually. | Consult public health officials. Bites of squirrels, hamsters, guinea pigs, gerbils, chipmunks, rats, mice, other small rodents, rabbits, and hares almost never require antirabies postexposure prophylaxis. |
*During the 10-day observation period, begin postexposure prophylaxis at the first sign of rabies in a dog, cat, or ferret that has bitten someone. If the animal exhibits clinical signs of rabies, it should be euthanized immediately and tested.
†The animal should be euthanized and tested as soon as possible. Holding for observation is not recommended. Discontinue vaccine if immunofluorescence test results of the animal are negative.
Treatment of Bite Injuries
Management of bite wounds to the face is not unlike managing other trauma to the head and neck. Because bite wounds can cause a wide variety of injuries, and because they may not be isolated injuries, appropriate attention to complete evaluation and adherence to Advanced Trauma Life Support (ATLS) protocols is important; plain film or computed tomography (CT) scans should be ordered, when appropriate.60 Certain aspect/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses