Secondary Revision of Soft Tissue Injury
Scarring is a natural progression of healing following soft tissue injury.1–3 The primary and immediate secondary management of head and neck wounds will inevitably affect the long-term aesthetic and functional outcomes of the resulting scar. Therefore, meticulous planning is needed from the initial patient encounter to ensure successful outcomes in scar healing, maturation, and revision. This chapter will review the evaluation and management of various post-traumatic scarring, with an emphasis on commonly encountered clinical scenarios. It is meant to provide the reader with a literature-based rationale for treatment.
Soft Tissue Wound Healing
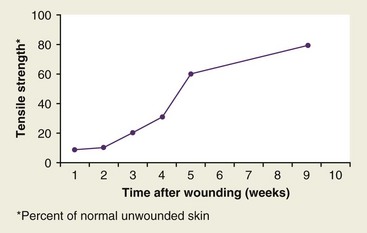
A basic understanding of wound healing is needed because of its relevance to scar formation and subsequent effects on revision.3–5 Wound healing is classified into three main phases (Fig. 22-1). These include the immediate inflammatory phase (1 to 3 days), which is characterized by a vascular and inflammatory response including local vasoconstriction for the first 5 to 10 minutes followed by a local vasodilatory response. The inflammatory phase takes place the first few days after injury, during which wound strength relies mainly on the fibrin clot. The second phase, the proliferation phase (3 to 12 days), begins within 24 hours after injury and is characterized by the recruitment of blood vessels and fibroblasts, resulting in granulation tissue. Epithelialization may be completed in 24 to 48 hours in primarily closed wounds or be delayed for as long as 3 to 5 days in wounds healing by secondary intention The final phase of wound healing is the maturation phase, during which the scar gains strength and volume and erythema decreases. Complete scar maturation and final tensile strength generally take 12 to 18 months (Fig. 22-2).
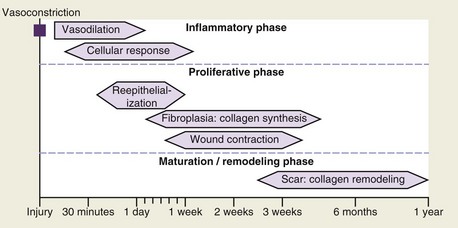
FIGURE 22-1 Phases of inflammation.
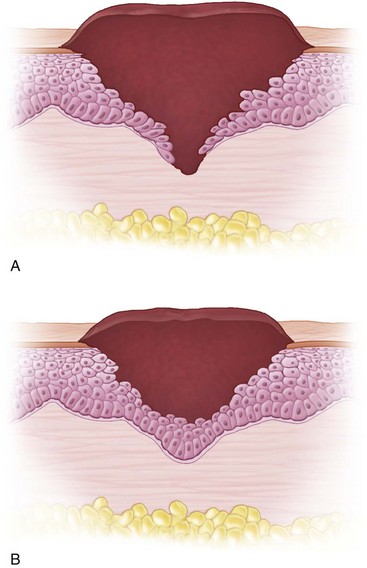
Scar consists of a poorly constructed collagen matrix in dense parallel bundles, which is contrasted to the efficiently cross-linked meshwork of collagen in the native dermis. It occurs in three phases—epithelialization migration, collagenization, and angiogenesis–granulation tissue formation. Epithelialization occurs by migration of keratinocytes over the dermis and under the clot (Fig. 22-3), which is facilitated by growth factors such as epidermal growth factor (EGF) and transforming growth factor α (TGF-α).6–8 Once a monolayer of keratinocytes covers the denuded wound surface, epithelial migration ceases and a new stratified epidermis with underlying basal lamina is reestablished from the margins of the wound inward. All aspects of a skin flap rarely touch along all the length of the wound; migration is aided by contraction of the underlying connective tissue. Within 3 to 4 days of injury, dermal fibroblasts around the wound begin to proliferate and lay down a collagen-rich matrix, a process modulated by platelet-derived growth factor (PDGF) and transforming growth factor β (TGF-β).9–12 Finally, angiogenesis of the wound and the incorporation of pink, capillary-filled granulation tissue is mediated by fibroblast growth factor 2 (FGF2) and vascular endothelial growth factor (VEGF) released at the site of the wound.13 Connective tissue contraction ultimately closes embryonic and adult wounds. The major difference between scar-free healing and scar formation is that a scar-free wound site has significantly less inflammation present.5
Principles of Wound Management
General principles of wound management should always be followed in the traumatic setting. These include an initial thorough removal of foreign bodies, débridement, and cleansing of the wound with copious pulsatile irrigation. Formal scrubbing of the wound may be undertaken if necessary but should be done sparingly to spare further damage to soft tissues. All devitalized soft tissue should be débrided and excised and sharp healthy wound margins should be obtained to facilitate closure, with minimal scarring.14 Devitalized tissue increases the local inflammatory response and subsequent scarring. Undiluted hydrogen peroxide use in open wounds should be avoided because it inhibits wound healing and may cause tissue necrosis. Normal saline with or without bacitracin is the preferred irrigant for soft tissue trauma. Although delayed closure may be necessary in some wounds caused by edema and/or high-velocity injuries such as gunshot wounds, in wounds with a significant amount of devitalized tissue, or because of other, more urgent medical and surgical interventions that precede the treatment of head and neck injuries, primary closure should be attempted, if feasible. In the case of avulsed tissue or the inability to reapproximate local tissue under minimal tension, local flaps, regional flaps, or free tissue transfer may be needed to restore tissues adequately to previous form and function.15 Wounds should be closed in layers, if possible, to place minimum tension on the superficial skin closure and aid in the eversion of skin edges to minimize scar widening.16 Tension across a wound decreases blood flow, which leads to necrosis of wound edges and increased connective tissue growth in the proliferation phase, and to elongation of scars in the remodeling phase.17,18 Skin flaps should be appropriately undermined so that wound edges can be everted, which will minimize scar depression.19
Meticulous attention to detail and gentle tissue handling are important to optimize wound healing and minimize scarring.1 A multivariate analysis has shown that characteristics associated with suboptimal cosmetic appearance following laceration and surgical incision closure are associated tissue trauma, use of electrocautery, incomplete wound edge apposition, and increased wound width (healing by secondary intention).20 If permanent sutures are used for wound closure, they should be removed in 5 days or less to prevent track marks. Another option is to use fast, resorbing plain gut suture (5.0 to 6.0). In a study that compared 5.0 or 6.0 nylon sutures versus plain gut sutures for skin closure in a population of pediatric patients who suffered lacerations, no difference in infection or wound dehiscence was found between the two groups; however, slightly better cosmesis was found in the plain gut suture group.21 Similar studies,22 including a meta-analysis,23 have confirmed these results, demonstrating no difference in long-term cosmesis, scar hypertrophy, infection rate, wound dehiscence, and wound erythema or edema between lacerations closed with nylon versus plain gut suture. For scalp incision and laceration repair, the use of staples as an alternative to suturing has been demonstrated in a randomized control trial to reduce procedure time significantly while not demonstrating any difference in cosmesis by a blinded physician at 1 week and 6 to 18 months postrepair.24
Adhesive bandages such as Steri-Strips (3M, Maplewood, Minn) should be used to reduce wound tension at the time of closure and to reduce the need for long-term suture placement in those wounds under increased tension. The use of 2-octyl cyanoacrylate–based fast-acting skin adhesives has been shown to be just as effective as Steri-Strips in reducing hypertrophic scar formation,25 although other study results have demonstrated superior cosmesis in wounds dressed with Steri-Strips.26 A review comparing the use of tissue adhesives versus standard wound closure in patients with traumatic lacerations found that pain and procedure time were significantly reduced in the tissue adhesive group and wound dehiscence and erythema were significantly reduced in the standard wound closure group; however, there was no difference in final cosmesis or scar appearance between the two groups.27
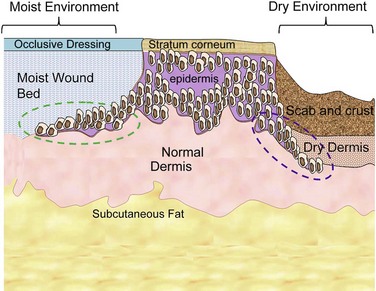
Desiccated and crusted wounds heal slower than those kept moist.28 Epithelial migration follows a path of moisture and humidity, even if this route is longer (Fig. 22-4). This often requires more energy expenditure by the cell. In addition, an apoptosis-mediated decrease in granulation tissue has been shown to occur in vitro in flaps that are covered postoperatively.29 Therefore, occlusive dressings and antibiotic ointment use are recommended so that epithelial migration proceeds in a direct and efficient manner. The use of occlusive or semiocclusive dressings has also been advocated as a means of promoting wound healing. Commercially available dressings, such as Tegaderm (3M), Opsite (Smith & Nephew, London), or similar polyurethane dressings minimize the amount of atmospheric oxygen that is absorbed directly through an open wound30,31 and have been shown to decrease epithelial closure time by as much as 50%.28,31–33 The moist environment is optimal for epithelial migration, with minimization of connective tissue formation, therefore expediting healing and reducing scar formation. These effects, however, have not been verified in a randomized control trial.34 Antibiotic ointment should be applied to the wound until epithelialization occurs. Bacteria delay healing by direct cell damage, prolonging the inflammatory phase of wound healing by competing for oxygen; therefore, in addition to providing a moist environment, antibiotic ointment is beneficial for reducing bacterial colonization.35
Wounds should be cleaned daily during the immediate postoperative period using a mixture of 50% hydrogen peroxide and 50% water. Sunblock should be applied to the area of wound closure to reduce irritation and minimize the inflammatory response. The patient should be instructed to massage the wound once epithelialization occurs using a simple base cream twice a day, 10 minutes at a time.36,37 The effects of scar massage, however, have been questioned.38 In addition, silicone sheets or gels may be used after epithelialization occurs and may assist in better scar maturation of hypertrophic and keloid scars.39–44 Although a barrier, silicone sheets do allow the passage of oxygen. It has been shown in an animal model that silicone sheets cause hydration of keratinocytes within the stratum corneum of the epidermis, which has a suppressive effect on the metabolism of underlying fibroblasts and results in decreased capillary activity, hyperemia, and collagen deposition, and therefore decreases dermal thickness and subsequent scar hypertrophy.45 Oxygen tension, pressure, or silicone leakage into dermis, however, has not been shown to be mechanisms for silicone effectiveness.46–49 Furthermore, silicone sheets have been found to improve pigmentation, vascularity, and reduce the height of scars after 3 months of postoperative use.50,51 Reduction of pain and pruritus has also been demonstrated to be a benefit of silicone sheets, but these benefits are not seen until after 6 months of use.52 In a study that used the Vancouver Scar Scale to assess the effects of silicone gel, silicone gel sheets, and allantoin in improving postburn scarring less than 6 months from injury, the investigators found no significant difference in the silicone gel and gel sheet group, but there was a significant difference in improvement when comparing the allantoin groups with the silicone sheet and silicone gels group.53 All three groups showed a significant improvement 6 months from baseline. The effects of silicone sheet use have been shown to last up to 6 months after removal; therefore, their benefits are maintained once they are discontinued54 Onion extract, another popular topical treatment for scars, has shown only to improve scar color while not having an effect on scar height.55
Preoperative Consultation
Detailed explanation of possible and realistic outcomes at the initial encounter will help circumvent any unreasonable expectations that the patient might have and prepare the patient for the reality that further procedures will be needed. Although the surgeon may have a good idea of which scar revision procedure the patient will need at the time of initial repair, it may not be until weeks to months later, after scar maturation occurs, that the surgeon will be able to formulate a definitive treatment plan. Depressed scars tend to contract initially and then relax as they mature, whereas hypertrophic scars and keloids will often grow as the patient ages. On follow-up examination, the surgeon should note scar tension and adjacent tissue laxity of the scar while attempting to predict the outcome of tissue rearrangement. In addition, the patient’s medical history should be revisited because much may be left out in the emergent setting. Hereditary, vascular, metabolic, and immune deficiencies may be detrimental to wound healing. Finally, the patient must be compliant with postoperative care. This not only includes local care to the wound, but maintaining proper nutrition, because vitamin and trace mineral deficiencies such as deficiencies of vitamin A, C, E, zinc, and iron can be detrimental to wound healing.31,56
Scar Analysis
The purpose of scar analysis is to use a reliable and valid measure for quick and efficient scar assessment, which requires that the surgeon have a firm understanding of scar terminology (Table 22-1).57 Documentation of a standardized assessment is necessary for developing a treatment plan and for serial evaluations. Photographic assessment using standardized lighting, spacing, positioning, camera settings, and background is beneficial for initially assessing and serially tracking the progress of the scar maturation.58–65 Imaging software can be used to analyze, measure, and follow scars and can aid in surgical planning by almost performing the surgery before the actual procedure.66 Immediate preoperative and postoperative photographs should be taken.67 It is useful to review photographs after the patient has left. It is then that the surgeon will often notice subtle abnormalities that could affect the management of the scar. Also, photographs will document changes in following appointments often overlooked by the patient and surgeon.
TABLE 22-1
| Scar Classification | Features |
| Mature scar | A light-colored, flat scar. |
| Immature scar | A red, sometimes itchy or painful, and slightly elevated scar in the process of remodeling. Many of these will mature normally over time, become flat, and assume a pigmentation that is similar to the surrounding skin, although they can be paler or slightly darker. |
| Linear hypertrophic (e.g., surgical or traumatic) scar | A red, raised, sometimes itchy scar confined to the border of the original surgical incision. This usually occurs within weeks after surgery. These scars may increase in size rapidly for 3-6 mo and then, after a static phase, begin to regress. They generally mature to have an elevated, slightly ropelike appearance with increased width, which is variable. The full maturation process may take up to 2 yr. |
| Widespread hypertrophic (e.g., burn) scar | A widespread, red, raised, sometimes itchy scar that remains within the borders of the burn injury. |
| Minor keloid | A focally raised itchy scar extending over normal tissue. This may develop up to 1 yr after injury and does not regress on its own. Simple surgical excision is often followed by recurrence. There may be a genetic abnormality involved in keloid scarring. Typical sites include earlobes. |
| Major keloid | A large, raised (>0.5 cm) scar, possibly painful or pruritic and extending over normal tissue. This often results from minor trauma and can continue to spread over years. |
Adapted from Mustoe TA, Cooter RD, Gold MH, et al: International clinical recommendations on scar management. Plast Reconstr Surg 110:560–571, 2002.
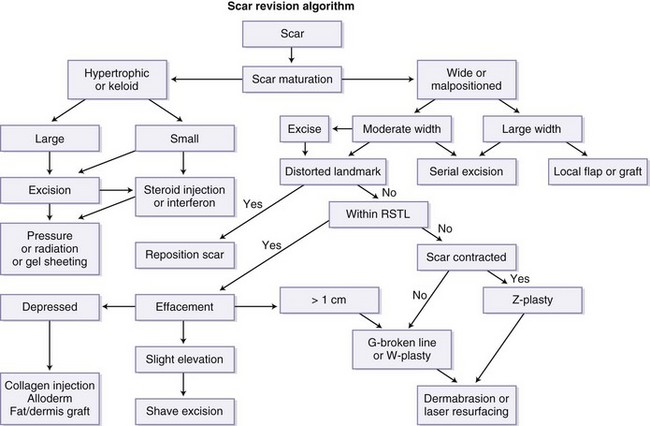
Several factors must be considered when developing a treatment plan for scar revision, such as scar width, length, relationship to relaxed skin tension lines (RSTLs), neighboring anatomic landmark distortion, tissue loss, scar type, patient age and race, scar location (visible versus nonvisible with clothing), skin type (Fitzpatrick), tissue tension and laxity, and local tissue reservoirs (Box 22-1). Figure 22-5 illustrates a basic template for the surgeon to use for scar revision, but this must be tailored to the specific patient and scar.
The most widely used scarring index is the Vancouver Scar Scale, which gives the surgeon an objective measure of burn scars and assists in prognosis and management. Although some have described it as a valid research tool with good interrater reliability (Table 22-2),68 others have not.69 Another scale, the patient and observer scar assessment, has an objective component comparable to the Vancouver scale, but relies on patient opinion (Table 22-3).70 A number of other subjective and objective assessment tools and devices have been reported in the literature.71–76 Most indices include the clinical assessment of vascularization, pigmentation, thickness, surface, pliability, size, reflection, distortion, texture, functional deficits, and pain. These characteristics are often a clue to the cause of the scar. For example, postinflammatory hyperpigmentation is often seen in scars associated with acne, inherited and acquired diseases, temperature extremes, sites of allergic reaction, radiation, and sun exposure.77 Hypopigmentation often has iatrogenic causes, such as chemical peel, dermabrasion, laser resurfacing or, with burns, trauma and infection.78,79
TABLE 22-2
| Scar Characteristic | Rating |
| Vascularity | |
| Normal | 0 |
| Pink | 1 |
| Red | 2 |
| Purple | 3 |
| Pigmentation | |
| Normal | 0 |
| Hypopigmentation | 1 |
| Mixed | 2 |
| Hyperpigmentation | 3 |
| Pliability | |
| Normal | 0 |
| Supple | 1 |
| Yielding | 2 |
| Firm | 3 |
| Ropes | 4 |
| Contracture | 5 |
| Height | |
| Flat | 0 |
| <2 mm | 1 |
| 2-5 mm | 2 |
| <5 mm | 3 |
TABLE 22-3
Patient and Observer Scar Assessment Scale
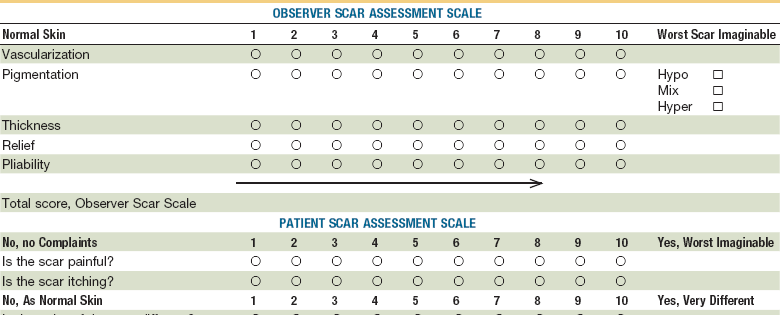
Adapted from Draaijers LJ, Tempelman FR, Botman YA, et al: The patient and observer scar assessment scale: A reliable and feasible tool for scar evaluation. Plast Reconstr Surg 113:1960–1965, 2004.
Scar contour exists on a continuum, from the depressed scar to the hypertrophic scar and keloid. Hypertrophic scars typically remain confined to the borders of the inciting injury and usually retain their shape, whereas keloids are defined as scars that extend beyond the borders of the original wound, do not regress spontaneously, and tend to recur following excision.80 Keloids present a special problem in treatment (see later). Scar depression often results from excessive tension across the wound. Scar texture and reflection are mainly concerns of aesthetics. Scar contracture may have functional and aesthetic ramifications in the head and neck. Pertinent to the craniomaxillofacial skeleton, scar tethering to underlying fascia, muscle, or bone may occur, resulting in aesthetic and functional deficits, mainly the failure to animate or move the face and neck.
Painful scars, especially those associated with burns, can severely debilitate the patient. The patient may present with allodynia, hyperesthesia, hypoesthesia, or dysesthesia, often caused by tissue adhesion, surround soft tissue damage, underlying skeletal damage, or neuroma or perineural scar formation. An increase in nociceptive nerve fibers following burn injury is associated with increased cutaneous innervation and increased density of certain neuropeptides, and may be responsible for chronic pain in patients with burns.81–83 Excision of this tissue, in addition to reconstruction using local, regional, or distant flaps, may relieve pain in some patients. Scars in the midline are less likely to produce pain, but may cause more scarring because of increased tension.84
Incision Placement
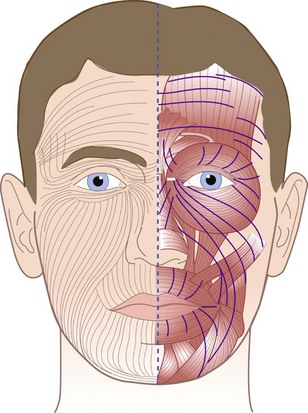
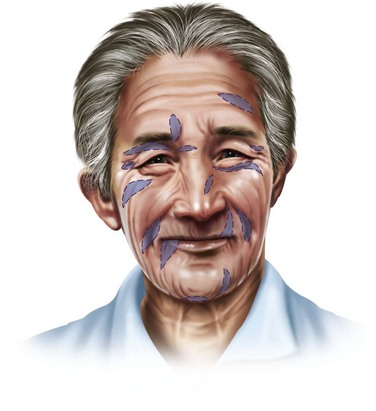
Understanding of the natural lines of tension of the head and neck is imperative for proper placement of skin incisions and to optimize final scar appearance (Fig. 22-6). Dupuytren first observed that an oval wound was created when a round instrument punctured the skin.85 Karl Langer, an anatomist, further studied this change in facial skin configuration in cadavers in rigor mortis and postulated that intrinsic skin tension occurred along predictable lines of cleavage.86 Later called Langer’s lines, these lines of tension became the basis for elective facial skin incisions for the next century. Langer’s studies were, however, limited because they were performed in cadavers, showing the effects of rigor mortis. Kraissl et al preferred lines perpendicular to the action of the underlying muscle.87–89 Borges has studied this concept in vivo and distinguished lines that follow furrows when the skin is relaxed from those that are produced by pinching the skin, and found that these lines are distinct from wrinkles, creases, and Langer’s lines and that the number of lines and spacing varies among individuals.90,91 Numerous other lines of tension have been described in the past by Cox, Webster, Stark, and Ogilvie, Kocher, and Kazanjian, among others.87,92 These lines of tension would be called Borges’ lines, or RSTLs. They follow furrows formed on relaxed skin. It has been demonstrated that placing incisions in the direction of RSTLs will produce more aesthetic outcomes with minimal scarring. RSTLs and wrinkles caused by aging may not be in the same location. Wrinkles are the change in overlying skin as a result of muscle pull over time. Conversely, RSTLs of the face often run perpendicular to the underlying muscle and, in the neck, they usually run perpendicular to areas of flexion (i.e., RSTLs run horizontally on the forehead, perpendicular to the vertical frontalis muscle). Examples of wrinkles that do not coincide with RSTLs include glabellar lines, crow’s feet, and bunny lines. An exception to this rule is in the area of the circular orbicularis oculi underlying the eyelids, where RSTLs run horizontal and parallel to the muscle because of the rigid scaffold of the tarsal plate. In older patients, RSTLs often run parallel with the natural creases and wrinkles of the face. RSTLs are determined by having the patient go through a series of facial expressions (e.g., smile, frown, laugh, squint) and then pinching the skin. The line where the longest straightest line results is the RSTL.93 RSTLS should be determined prior to administration of local anesthesia.
The lines of maximum extensibility (LMEs), also known as antitension lines (ATLs), run perpendicular to RSTLs. When incisions are placed perpendicular to RSTLs, an S-shaped scar will develop. Pinching the skin perpendicular to RSTLs produces humps; incisions parallel to this plane should be avoided. When the areas is too distorted for assessment, the contralateral side may be used.94 Incisions made parallel to the RSTL will produce a narrow scar under minimal tension, as opposed to those placed parallel to the LME or ATL, which will be under maximum tension and will have a significant propensity to widen and produce broad unsightly scars. A major factor in deciding to undertake scar revision is whether scars are located perpendicular to RSTLs or in ATLs. Note that the ultimate goal of scar revision is to orient the scar parallel to RSTLs.
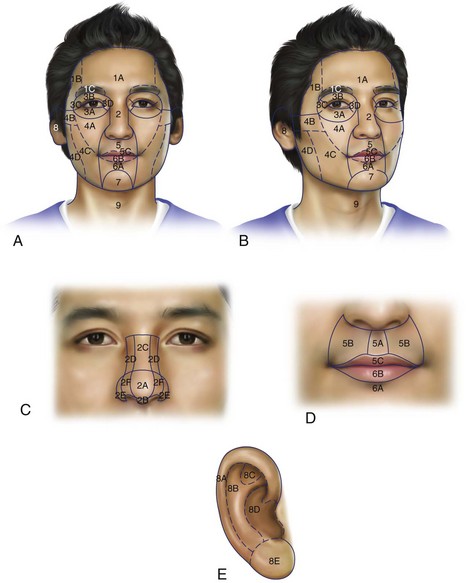
Facial Aesthetic Units
In trauma and reconstructive facial surgery, the face can be divided into facial aesthetic units.95 Gonzales-Ulloa initially described 14 aesthetic units.96–99 These include the forehead, right and left cheeks, nose, right and left upper lids, right and left lower lids, right and left ears, upper lip, lower lip, mental region, and the neck (Fig. 22-7). These aesthetic units can be further classified into subunits based on skin thickness, color, elasticity, and underlying structural support. Additional subunits within each facial unit have been described that delineate natural break lines that allow the surgeon to conceal a scar or skin graft placement100 (Fig. 22-7). For example, the nose can be broken down into the nasal bridge, sidewall, tip, ala, soft triangle, and columella.101 The upper lip is divided into the philtrum column, nostril sill, alar base, and nasolabial crease102 Placement of incisions at the seams of these units or subunits, or at facial midline will produce the least perceivable scars.
When planning excisional scar revision, care should be taken to limit the revision to within one facial unit. For example, when revising a scar of the cheek, the revised procedure should not encroach on the upper lip or lower eyelid unit. Facial units are important in oncologic skin resection and in regard to tissue avulsion in trauma, when it is important to remove the entire unit or subunit, even if extension of the incision is necessary. The subsequent reconstruction, whether it be local or regional flaps or free tissue transfer, should span the entire facial unit or subunit. When the avulsed or excised area of tissue encompasses an entire unit and subunit, the final outcome blends with surrounding tissues and is less conspicuous.1,102
Scar Type, Pattern, and Color
It is important for the surgeon to consider the type and pattern of scar when considering surgical revision, which also may give an indication about the type and extent of injury. For example, flat, linear, or curved scars often result from low-energy injuries and are more easily treated than depressed scars and scars resulting from high-energy avulsive tissue loss. Wide scars caused by increased wound tension or tissue loss are often flat and faded and are difficult to treat because of a texture mismatch with surrounding tissues. These scars often need reexcision and closure. Some hypertrophic scars or keloids may benefit from excision or other nonsurgical treatment such as intralesional steroid injection, chemotherapy, cryotherapy, radiation, laser, or silicone sheet treatment.80 Atrophic or volume-depleted scars often result from wounds not closed primarily, in stellate scars, with inappropriate approximation of wound edges in primary closure, or in deep abrasions. These scars often require dermal fillers, including autogenous materials such as fat transfer103,104 and synthetic fillers.1
Scar camouflage is difficult in widened scars because of their smooth shiny surface, which reflects light differently than adjacent tissues. Similarly, scars that cross multiple facial units and subunits are challenging to treat because they are usually have varying skin texture, thickness, and histologic makeup. For example, nasal skin is different than skin of surrounding facial subunits containing a thicker dermis and higher density of sebaceous glands; therefore, the nearest skin is the best donor for reconstruction.101
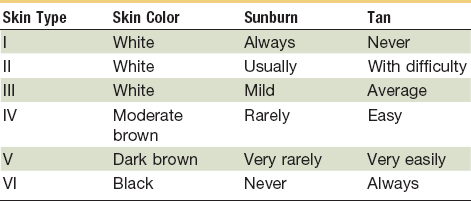
Sun-Reactive Skin Type Classification
Fitzpatrick developed the sun-reactive skin type classification to describe the degree of skin reaction after sun exposure105–107 (Table 22-4). Although developed as a guide for the treatment of skin rejuvenation procedures, this classification scheme is useful when choosing the correct management of the traumatic scar. Patients with a higher classification will often experience inflammatory changes such as dyspigmentation after soft tissue injury. Although hyperpigmentation is usually temporary, hypopigmentation is often the permanent result of a mature scar. Furthermore, patients with a very fair skin (Fitzpatrick classification type I or II) will often respond better to laser resurfacing, whereas patients with very dark skin (Fitzpatrick type IV or V) may benefit from more conservative treatment, such as superficial chemical peels and scar excision.108,109
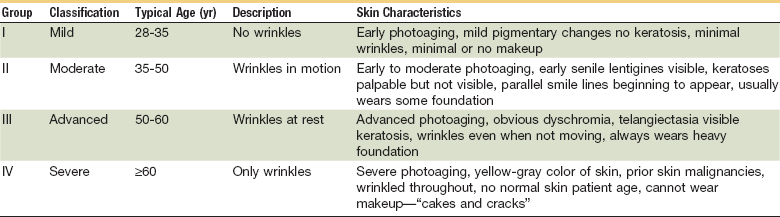
Skin and Aging
A patient’s age will often guide the surgeon to the timing and type of treatment chosen for scar revision. Older patients should be evaluated for the risks versus benefit in any surgical procedure in the context of complex medical comorbidities. Glogau has developed a classification for skin wrinkling related to aging as a guide to treatment for each skin type (Table 22-5). This should be taken into consideration before undertaking scar revision procedures, because skin resurfacing techniques can be chosen to match the depth of wrinkles and degree of wrinkling.110
It has been recommended that children have a higher tendency for scar widening than adults and should undergo scar revision after puberty because of a prolonged and exuberant inflammatory response, increased skin tension, diminished skin and dermal thickness, and higher concentration of collagen and elastin,.111 Children past the age of puberty are more likely to cooperate with treatment and postoperative care than their younger counterparts. Severe psychological or functional impairment secondary to scar formation, however, may warrant earlier treatment.
Timing of Scar Revision
Experience has shown that in general, the appearance of most scars tends to improve spontaneously after a period of maturation during the first year after injury, after which time the appearance of the scar stabilizes and surgical revision may be considered.112,113 However, scars oriented perpendicular to RSTLs or those associated with functional impairment may be revised earlier than 1 year on an individualized basis.114,115
Early scar revision may be undertaken as early as 4 weeks when there is severe functional impairment, such as salivary and lacrimal gland obstruction, lip incompetence, or lagophthalmos with corneal exposure. Early scar revision may also be advisable in well-localized scars sustained from low-energy injuries in which adjacent skin damage is minimal. Although a delay in scar revision of at least 6 months is generally recommended for most adult scars, high-energy injuries may continue to remodel and mature over a longer period of time, and delay for 12 months may be advisable.116
Interventions such as dermabrasion and shave excision may be performed as soon as 4 weeks from the initial wound repair, based on the high level of fibroblastic activity during this period. Because dermabrasion itself causes erythema, early intervention may overlap with erythema from initial repair, leading to less total time of erythema for the patient. For hypertrophic scars and keloids, steroid injections may be considered as early as 3 weeks and may be given at the time of scar revision. Cigarette smoking, isotretinoin, and vitamin E use are injurious to wounds and scar revision should be delayed until they have been discontinued.117
Surgical Options
Scar revision can be broken down into three different treatment modalities—scar excision, tissue rearrangement, and surface treatment (Box 22-2). The selection of treatment should be based on the individual scar and on the needs and expectations of the patient. For example, conservative treatment may be warranted for a demanding patient with unrealistic expectations. Narrow scars parallel to RSTLs may have distracting features such as surface discoloration and texture irregularities. These scars will often benefit from surface treatments. Longer scars, which vary more than 35 degree from neighboring RSTLs and have a local tissue reservoir, may be improved with tissue rearrangement such as W-plasty or geometric broken line excision and closure (GBLC). Z-plasty, local or regional flaps, or free tissue transfer may be indicated if neighboring tissue reservoirs are deficient or if anatomic structures and landmarks would be distorted by closure.
General Principles of Linear Scar Revision
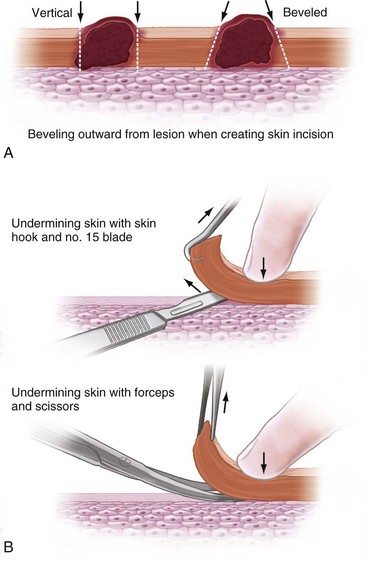
Most facial incisions may be made with a no. 15 or no. 11 blade on a no. 9 knife handle. The no. 11 blade is the most useful for straight cuts; these should be made perpendicular to the skin in a sawing-type motion, with the tip of the blade used to make initial incision. The handle of the blade is then brought down toward the skin so that the belly of the blade cuts the middle part of the incision. Finally, the blade handle is brought up again so that the tip finishes the incision. This technique ensures that skin and subcutaneous layers are incised evenly throughout the entire incision. If incising a scar, the blade should be beveled outward (Fig. 22-8A). This aids in creating a plane for undermining skin, allowing eversion of the wound edges and minimizing scar depression. The skin at the ends and sides of the incision should then be undermined with a no. 15 blade or curved scissors at least 2 cm in the subdermal plane to avoid motor nerves of the face (see Fig. 22-8B). Undermining the scalp will not aid in closure because of the tensile strength of the galea aponeurosis. Galeotomies, however, may assist with mobilization and eversion of scalp tissue.
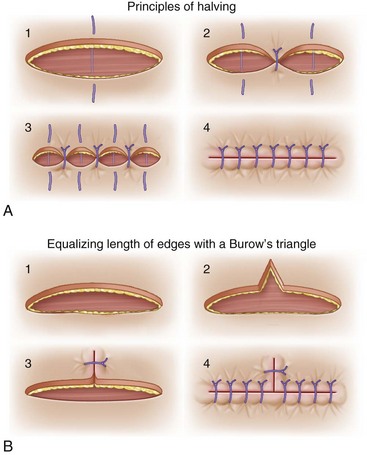
Primary closure should be achieved, whenever possible. Healing by secondary intention may be advisable in some cases, however, such as the lateral canthi of the eyes, where skin is thin and well-contoured and is subject to constant motion because of lid closure. To avoid bunching (dog ear) at wound edges, the principle of halving should be used, whereby the first suture is placed at the center of the incision and the next two are placed at the center of the remaining halves (Fig. 22-9A). Continuing this down the length of the skin margins will close the wound with equal tension and eversion throughout. When incisions are not of equal length and shape, the principle of equalizing edges should be used (see Fig. 22-9B). In this technique, a Burow’s triangle is removed from the longer skin flap and closed primarily to make the two primary skin flaps equal in length.
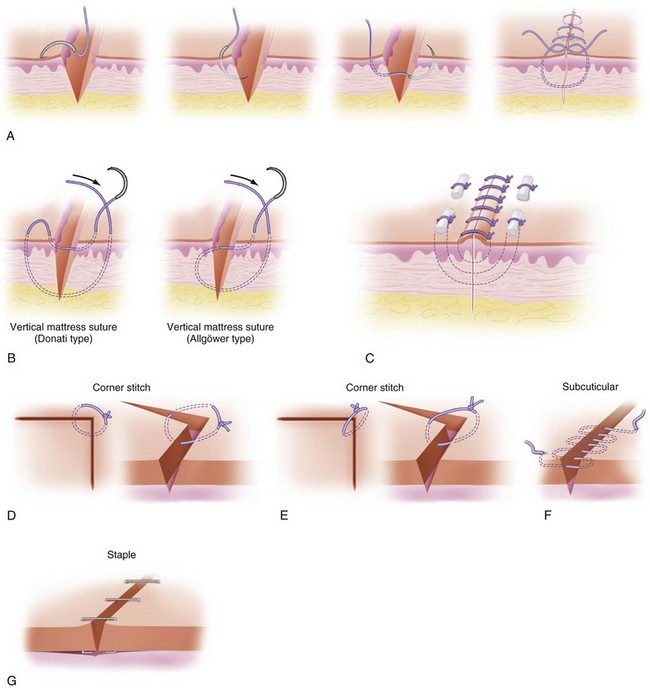
Meticulous attention to proper suturing technique is important for successful outcomes. A simple stitch provides minimal wound eversion and scant relief of wound tension, and should be avoided in the face. Alternatively, a mattress suturing technique is best for ensuring a tension-free wound closure, with eversion of the skin edges. The suture needle should be angled outward from the skin edge and the knot tied as far as possible from the wound (Fig. 22-10A). The vertical mattress suture is performed by placing the innermost suture first while holding up the wound edge, causing eversion of the skin flap. The wide suture should be thrown next. There are two types of vertical mattress sutures, the Donati and Allgower types (see Fig. 22-10B). Bolsters of silicone tubing or swabs may be placed under the knots of the vertical mattress to minimize tension (see Fig. 22-10C). A simple interrupted (see Fig. 22-10D) or, preferably, a Gilles half- buried corner stitch should be used (see Fig. 22-10E) for tacking wound corners, The Gilles half- buried stich is performed by placing a subcutaneous suture in the corner flap, finishing transcutaneously in the opposing skin edge. The most useful stitch for relieving skin tension and everting wound edges, however, is the running buried subcuticular stich. However, care must be taken to avoid tension and skin edge vascular compromise ( see Fig. 22-10F). It should be noted that a running subcuticular suture does not relieve tension from wound edges like a simple subcuticular stich. Preferably, a monofilament absorbable suture on a small half-curved reverse cutting needle should be used. The stich should be placed while everting the skin edge with a skin hook at the middle finger of the surgeon and reaching the suture back under the dermis 2 to 3 mm from the wound edge. The knot should be buried. The skin should then be closed with fast-absorbing gut or monofilament to align the depth of the two skin flaps. Skin staples provide wound eversion, are positioned above the level of the skin when placed, and are useful for scalp and neck defect closure (see Fig. 22-10G).
Procedures
Scar Excision
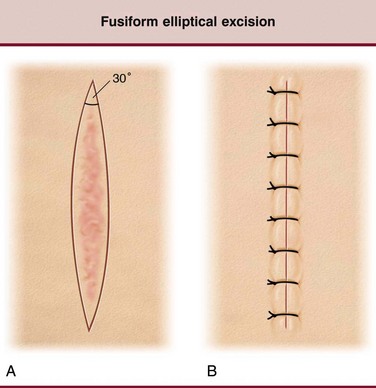
The fusiform, or elliptical, incision is the most common incision used in the head and neck. It should be placed within the RSTL, with a length-to-width ratio of 2.5 : 1 to 3 : 1 to limit dog ears (Fig. 22-11). It may be straight or crescent-shaped, but should always follow a long axis parallel to RSTLs and be limited to scars shorter than 2 cm.115,118,119 The only exception to this is the lower eyelid, where a crescent-shaped incision may leave an unsightly scar. It should be used for short anti-RSTL scars, achieving a more favorable reorientation of the lesion, or for short but widened or depressed scars. Internal angles of the planned excision may not exceed 30 degrees (Fig. 22-12).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses