Benign Tumors
Disease Mechanism
A benign tumor represents a new uncoordinated growth that generally has the following characteristics. Benign tumors are slowly growing and spread by direct extension and not by metastases. They tend to resemble the tissue of origin histologically. For example, an ameloblastoma, a tumor thought to be derived from odontogenic epithelium, often is composed of cells that resemble ameloblasts. It is thought that benign tumors have unlimited growth potential. Hamartomas often are included in the category of benign tumors. However, hamartomas are overgrowths of disorganized normal tissue that have a limited growth potential. For example, an odontoma is a hamartoma of dental tissue (disorganized enamel, dentin, and pulp tissues) derived from the dental follicle that stops growing at approximately the same time as other normal dental tissues. Included in this chapter are hyperplasias. Hyperplasia refers to a growth formed by an increase in the number of cells of a tissue but differs from a hamartoma in that the tissue is in a normal arrangement. Hyperplasia is generally thought to be a reaction to a stimulus, such as inflammation. Therefore, hyperplasias have limited growth potential and tend to regress when the stimulus is removed.
Clinical Features
Benign tumors typically have an insidious onset and grow slowly. These tumors usually are painless, do not metastasize, and are not life-threatening unless they interfere with a vital organ by direct extension.
Benign tumors are usually detected clinically by enlargement of the jaws or are found during a radiographic examination. Sometimes the radiologic examination is performed to try to discover the reason for the lack of development of a tooth.
Radiologic Examination
Once the clinician has made a preliminary diagnosis of the presence of a tumor, a full radiologic examination should be performed to document the extent and characteristics of the lesion. This examination may entail further images, such as panoramic, intraoral, or occlusal images. For central bone lesions, the addition of computed tomographic (CT) imaging is essential for assessing the three-dimensional characteristics of the entity. If the lesion originates in soft tissue or has extended from bone into the surrounding soft tissue, magnetic resonance imaging (MRI) may be required.
A thorough radiologic examination provides information regarding the extent of the lesion. On one hand, sometimes the characteristics are so specific that a preliminary diagnosis of the type of benign tumor can be made. On the other hand, the imaging characteristics of the lesion may fail to indicate the type of tumor. A thorough workup also indicates the most favorable biopsy site. In most cases, the radiologic examination should be completed before the biopsy procedure.
Imaging Features
The following general features suggest the presence of a benign neoplasm.
Location
Because many tumors have a specific anatomic predilection, the location of a particular neoplasm is important in establishing the differential diagnosis. For example, odontogenic lesions occur in the alveolar processes above the inferior alveolar nerve canal, where tooth formation occurs. Vascular and neural lesions may originate inside the mandibular canal, arising from the neurovascular tissues. Cartilaginous tumors occur in jaw locations where residual cartilaginous cells lie, such as around the mandibular condyle.
Periphery and Shape
Benign tumors enlarge slowly by formation of additional internal tissue and, as a result, the borders of benign tumors appear relatively smooth, well defined, and sometimes corticated. If the tumor produces a calcified product, such as abnormal tooth material or abnormal bone, the most mature part of the tumor is in the central region with the most immature aspect at the periphery. Sometimes a radiolucent band of soft tissue or capsule results at the periphery where the calcified product has not yet formed; this band separates the more mature internal radiopaque portion from the surrounding normal bone.
Internal Structure
The internal structure may be completely radiolucent or radiopaque or may be a mixture of radiolucent and radiopaque tissues. If the lesion contains radiopaque elements, these structures usually represent residual bone, reactive bone formation, or a calcified material that is being produced by the tumor. Curved septa that are characteristic in ameloblastoma represent residual bone trapped inside the tumor that has remodeled into curved septa by internal cystic structures. An ameloblastoma does not produce bone. An osteoblastoma often has an internal granular radiopaque pattern produced by the abnormal bone that is actually being manufactured by the tumor. Often the internal pattern is characteristic for specific types of tumors and may help with the diagnosis. A totally radiolucent internal structure is not as useful as an aid to the diagnosis.
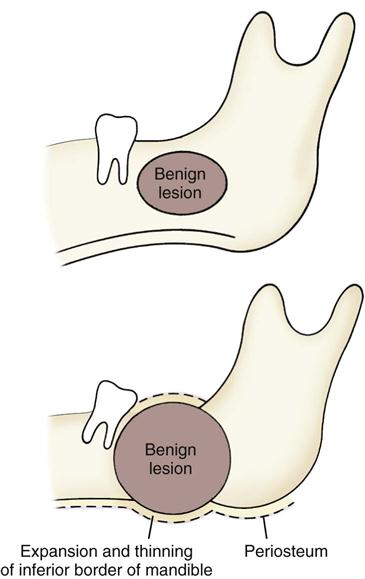
Effects on Surrounding Structures
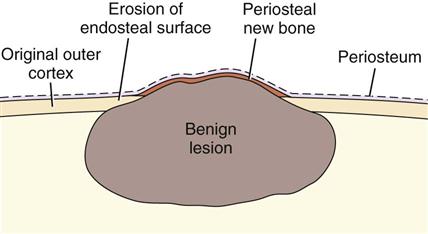
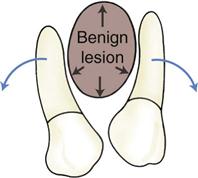
The manner in which a tumor affects adjacent tissues may suggest a benign behavior. For example, a benign tumor exerts pressure on neighboring structures, resulting in the displacement of teeth or bony cortices. If the growth is slow enough, there is adequate time for the outer cortex to remodel in response to the pressure, resulting in an appearance that the cortex has been displaced by the tumor (Fig. 22-1). This appearance is caused by simultaneous resorption of bone along the inner surface (endosteal) of the cortex and deposition of bone along the outer cortical surface by the periosteum (Fig. 22-2). Through this remodeling process, the cortex maintains its integrity and resists perforation, although faster growing tumors may exceed this process resulting in perforation of the cortex. Benign tumors may also cause bodily displacement of nearby teeth (Fig. 22-3). The movement of teeth adjacent to benign tumors is slow because these lesions grow slowly.
The roots of teeth may be resorbed by either benign or malignant tumors, but root resorption more commonly is associated with benign processes. The benign tumors especially likely to resorb roots are ameloblastomas, ossifying fibromas, and central giant cell granulomas. Benign tumors tend to resorb the adjacent root surfaces in a smooth fashion. Bone dysplasias such as fibrous dysplasia do not usually resorb teeth. When root resorption is associated with malignant tumors, the resorption is usually in smaller quantities causing thinning of the root into a “spiked” shape.
Hyperplasias
Disease Mechanism
Bony hyperplasias are included in this chapter but are not considered tumors because of the normal arrangement of the tissue and limited growth potential; in some cases, this growth is in response to a stimulus. Bony hyperplasias are growths of normal new bone that sometimes occur in characteristic locations. In dentistry, the terms exostosis and hyperostosis are both used to describe a bony growth that occurs on the surface of normal bone. In the medical literature, the term exostosis often is used for a surface bony growth with a cartilage cap (osteochondroma). Therefore, the term hyperostosis may be preferred to avoid confusion.
Torus Palatinus
Synonym
A synonym for torus palatinus is palatine torus.
Disease Mechanism
Torus palatinus is a bony protuberance (hyperostosis) that occurs in the middle third of the midline of the hard palate.
Clinical Features
Torus palatinus, the most common hyperostosis, occurs in about 20% of the population, although various studies have shown marked differences in racial groups. It develops about twice as often in women as in men and more often in Native Americans, Eskimos, and Norwegians. Although it may be discovered at any age, it is rare in children. It usually begins developing in young adults before 30 years of age and is thought to arise through interplay of genetic and environmental factors. The base of the bony nodule extends along the central portion of the hard palate, and the bulk reaches downward into the oral cavity. The size and shape of a torus palatinus can vary, and these lesions have been described as flat, lobulated, nodular, or mushroom-like (Fig. 22-4, A). Normal mucosa covers the bony mass and may appear pale and sometimes ulcerated when traumatized. Patients often are unaware of this hyperplasia, and patients who do discover it may insist that it occurred suddenly and has been growing rapidly.
Imaging Features
Location.
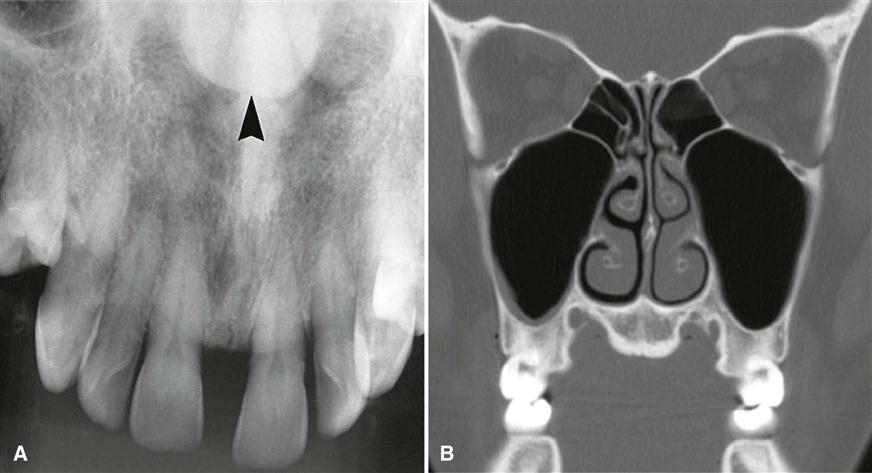
On maxillary periapical or panoramic images, a torus palatinus appears as a dense radiopaque shadow below and attached to the hard palate. It may be superimposed over the apical areas of the maxillary teeth, especially if the torus has developed in the middle or anterior regions of the palate. The image of a palatal torus may project over the roots of the maxillary molars (Fig. 22-4, B), but this image usually moves in its position relative to the roots of the teeth if another film is taken with a different horizontal or vertical angulation of the central ray (Fig. 22-5).
Periphery and Shape.
The border of the radiopaque shadow usually is well defined and may have a convex or a lobulated outline (Fig. 22-6).
Internal Structure.
The internal aspect is homogeneously radiopaque.
Treatment
A torus palatinus usually does not require treatment, although removal may be necessary if a maxillary denture is to be made.
Torus Mandibularis
Synonym
A synonym for torus mandibularis is mandibular torus.
Disease Mechanism
Torus mandibularis is a hyperostosis that protrudes from the lingual aspect of the mandibular alveolar process, usually near the premolar teeth.
Clinical Features
Tori occur less often on the lingual surface of the mandible than on the palate, with the former occurring in about 8% of the population. These tori develop singly or multiply, unilaterally or bilaterally (usually bilaterally), and most often in the premolar region. The size also varies, ranging from an outgrowth that is just palpable to one that contacts a torus on the opposite side. In contrast to torus palatinus, torus mandibularis develops later, being first discovered in middle-aged adults. However, it has the same gender predilection as torus palatinus. In women, the occurrence of torus mandibularis correlates with that of torus palatinus, but this apparently is not the case in men. As with torus palatinus, torus mandibularis may occur more often in individuals of Asian ancestry.
Genetic and environmental factors seem to be involved in the development of torus mandibularis, but masticatory stress is reported as an essential factor underlying its formation. The high prevalence among Eskimos and other subarctic peoples who make extraordinary chewing demands on their teeth seems to support this suggestion. Also, a patient with a torus mandibularis has, on average, more teeth present than a patient without a torus.
Imaging Features
Location.
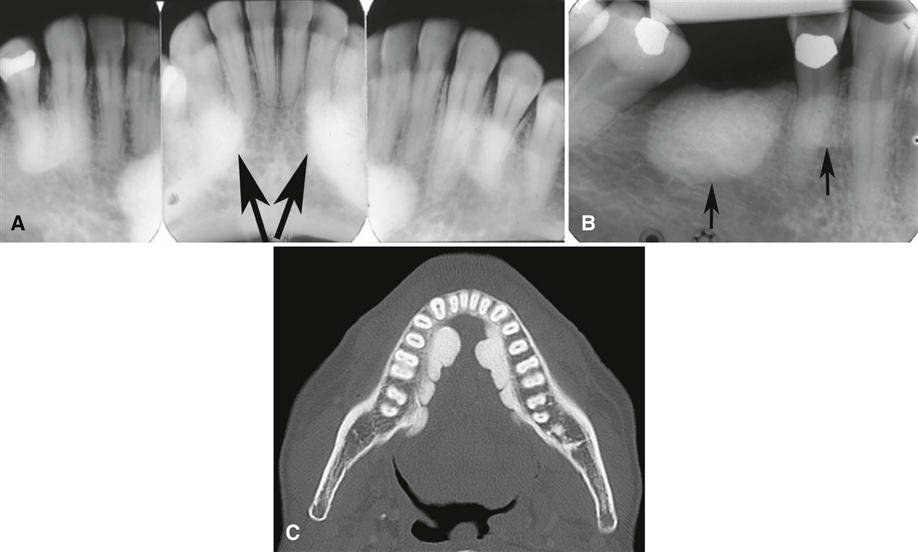
Recognition of mandibular tori relies on their appearance and location. Their presence bilaterally reinforces this impression, although they can occur unilaterally. On mandibular periapical images, a torus mandibularis appears as a radiopaque shadow, usually superimposed on the roots of premolars and molars and occasionally over a canine or incisor. It usually is superimposed over about three teeth.
Periphery.
Mandibular tori are sharply demarcated anteriorly on periapical images and are less dense and less well defined as they extend posteriorly (Fig. 22-7). There is no margin between the periphery of the torus and the surface of the mandible because the torus is continuous with the mandibular cortex.
Internal Structure.
On occlusal images, a mandibular torus appears as radiopaque and homogeneous (Fig. 22-8).
Treatment
A torus mandibularis usually does not require treatment, although removal may be necessary if a mandibular denture is planned.
Hyperostosis
Synonym
Exostosis is a synonym for hyperostosis. In the dental literature, the terms hyperostosis and exostosis are equivalent, but in the medical literature the term exostosis is often used as an equivalent term for osteochondroma, which is different from the entity hyperostosis.
Disease Mechanism
In addition to tori, other hyperostoses or exostoses may occur at other sites in the jaws. These are usually small regions of osseous hyperplasia of cortical bone and occasionally internal cancellous bone and usually occur on the surface of the alveolar process.
Clinical Features
Hyperostoses may develop most commonly on the buccal surface of the maxillary alveolar process, usually in the canine or molar area. They may also occur on the palatal surface or crest and less commonly on the mandibular alveolar process. Occasionally, they grow on the crest under a pontic of a fixed bridge. They are less common than mandibular or palatine tori, may attain a large size, and may be solitary or multiple. They are nodular, pedunculated, or flat prominences on the surface of the bone. They are covered with a normal mucosa and are bony hard on palpation. Published studies suggest a male predominance and an increase in frequency with age. As with the tori described previously, they appear to be more prevalent in Native Americans.
Imaging Features
Location.
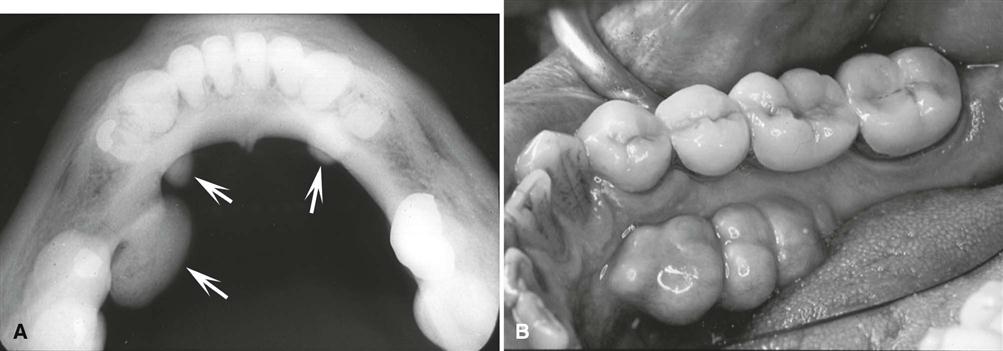
The maxillary alveolar process is the most common location, and usually the image overlaps the roots of the adjacent teeth.
Periphery.
The periphery of a hyperostosis is usually well defined and smoothly contoured with a curved border (Fig. 22-9). However, some may have poorly defined borders that blend into the surrounding normal bone.
Internal Structure.
The internal aspect of a hyperostosis usually is homogeneous and radiopaque. Although large hyperostoses can have an internal cancellous bone pattern, they most often consist only of cortical bone.
Treatment
Hyperostoses usually do not require treatment.
Dense Bone Island
Synonyms
Enostosis and periapical idiopathic osteosclerosis are synonyms for dense bone island (DBI).
Disease Mechanism
DBIs are the internal counterparts of exostoses. They are localized growths of compact bone that develop within the cancellous bone.
Clinical Features
DBIs are asymptomatic.
Imaging Features
Location.
DBIs are more common in the mandible than in the maxilla. They occur most often in the premolar-molar area (Fig. 22-10), although their existence does not correlate with the presence or absence of teeth.
Periphery.
The periphery is usually well defined but occasionally blends with the trabeculae of the surrounding bone. There is no trace of a radiolucent margin or capsule as the radiopaque DBI abuts directly against normal bone.
Internal Structure.
The internal aspect of DBIs usually is uniformly radiopaque without any characteristic pattern, but sometimes there may be patches of more radiolucent areas depending on form and thickness.
Effects on Surrounding Structures.
Rarely, a DBI is located periapical to a tooth root and is associated with external root resorption (see Fig. 22-10, C). The tooth most often involved is the mandibular first molar. In all circumstances, the tooth is vital, and the root resorption appears to be self-limiting. In very rare cases, DBIs can inhibit the eruption of a tooth and even displace a tooth.
Differential Diagnosis
Several radiopaque entities must be considered in forming a differential diagnosis. Periapical osseous dysplasia (POD) can be differentiated by the presence of its radiolucent periphery. When a DBI is located at the root apex, it may resemble periapical sclerosing osteitis. However, in periapical osteitis, there is an associated widening of the periapical portion of the periodontal membrane space. Also, periapical osteitis should be centered on the root apex of the tooth and extend in a more symmetric form in every direction. Finally, an inflammatory lesion may have an apparent etiology, such as a large restoration or carious lesion. There may be some similarity to hypercementosis or a benign cementoblastoma, but in both cases there should be a soft tissue (radiolucent) capsule at the periphery. DBIs are often static but may increase in size, especially when there is active growth of the jaws. If five or more DBIs are present, familial adenomatous polyposis (e.g., Gardner’s syndrome) should be considered.
Treatment
DBI does not require treatment. If multiple DBIs are present, the patient’s family history should be reviewed for incidences of cancer of the intestine.
Benign Tumors
Benign neoplasias are separated into two major groups: (1) odontogenic tumors and (2) nonodontogenic tumors.
Odontogenic Tumors
Disease Mechanism
Odontogenic tumors arise from the tissues of the odontogenic apparatus. According to the World Health Organization (WHO), these tumors can be classified into three categories depending on the type of tissue that makes up each tumor: (1) tumors composed of odontogenic epithelium, (2) mixed tumors composed of both odontogenic epithelium and odontogenic ectomesenchyme (connective tissue), and (3) tumors composed of primarily ectomesenchyme. Odontogenic tumors account for 1.3% to 15% of all oral tumors. Benign jaw tumors are presented in this chapter according to their tissues of origin. This format should assist the reader in learning to correlate the radiographic appearance of tumors with the underlying pathologic basis of the disease process.
Odontogenic Epithelial Tumors
Ameloblastoma
Synonyms.
Synonyms for ameloblastoma include adamantinoma, adamantoblastoma, and epithelial odontoma.
Disease Mechanism.
Ameloblastoma, a true neoplasm of odontogenic epithelium, is a persistent and locally invasive tumor; it has aggressive but benign growth characteristics. Ameloblastomas are by far the most common odontogenic tumor. Ameloblastoma is an aggressive neoplasm that arises from remnants of the dental lamina and dental organ (odontogenic epithelium). Malignant forms of this neoplasm exist, and these are discussed in Chapter 24. Ameloblastomas may be divided into solid/multicystic type, unicystic type, and desmoplastic type. The unicystic variant may develop as a single entity or may form from the epithelial lining of a dentigerous cyst; this is called a mural (within the wall) ameloblastoma. The existence of peripheral (soft tissue location) forms of this neoplasm is well documented.
Clinical Features.
There is a slight predilection for this lesion to occur in men, and it develops more often in African Americans. Although it may be found in young children (3 years) and in individuals older than 80 years, most patients are between 20 and 50 years of age, with the average age at discovery about 40 years.
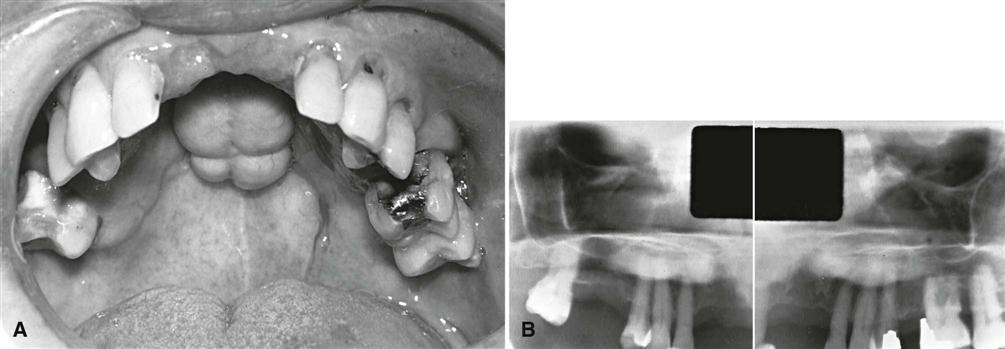
Ameloblastomas grow slowly, and few, if any, symptoms occur in the early stages. The tumor is frequently discovered during a routine dental examination. Usually the patient eventually notices gradually increasing facial asymmetry. Swelling of the cheek, gingiva, or hard palate has been reported as the chief complaint in 95% of untreated maxillary ameloblastomas. The mucosa over the mass is normal, but teeth in the involved region may be displaced and become mobile. In most cases, patients with ameloblastomas do not have pain, paresthesia, fistula, ulcer formation, or tooth mobility. As the tumor enlarges, palpation may elicit a bony hard sensation or crepitus as the bone thins. If the lesion destroys overlying bone, the swelling may feel firm or fluctuant. As it grows, this tumor can cause bony expansion and sometimes erosion through the adjacent cortical plate with subsequent invasion of the adjacent soft tissues.
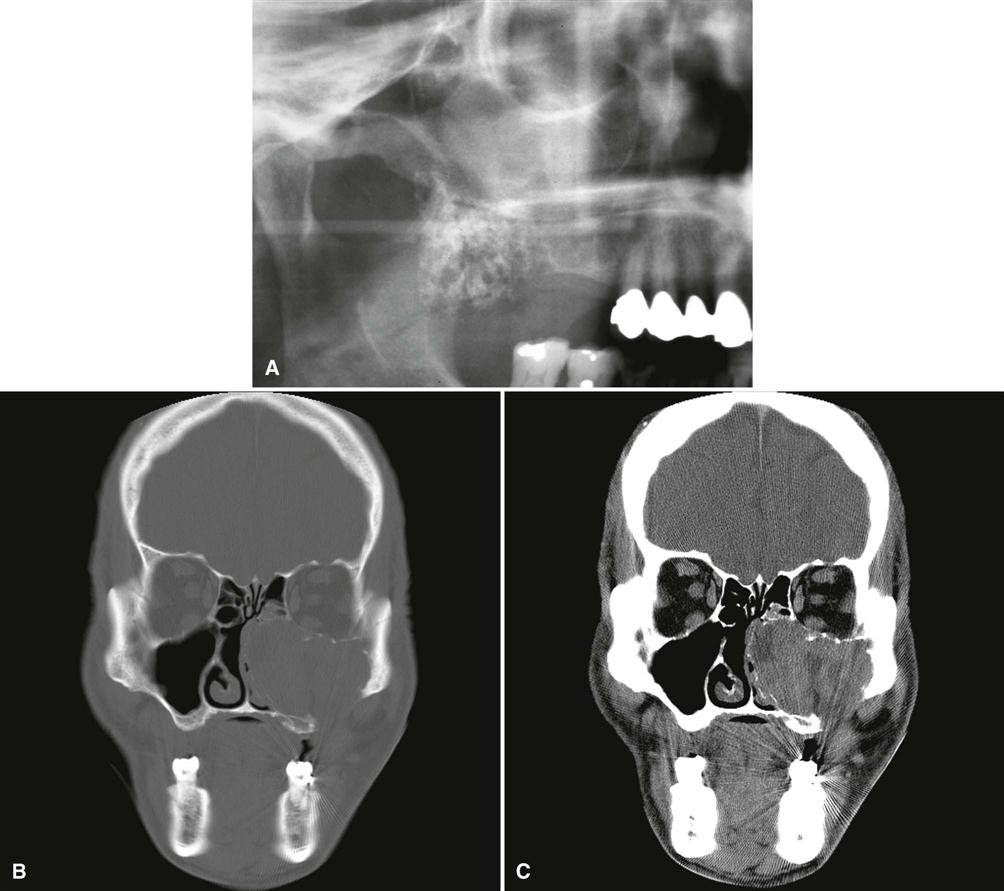
An untreated tumor may grow to a great size and is more of a concern in the maxilla, where it can extend into vital structures and reach into the cranial base. Tumors that develop in the maxilla may extend into the paranasal sinuses, orbit, nasopharynx, or vital structures at the base of the skull. Recurrence rates are higher in older patients and in patients with multilocular lesions. As seen with other jaw tumors, local recurrence, whether detected radiographically or histologically, may have a more aggressive character than the original tumor.
Imaging Features
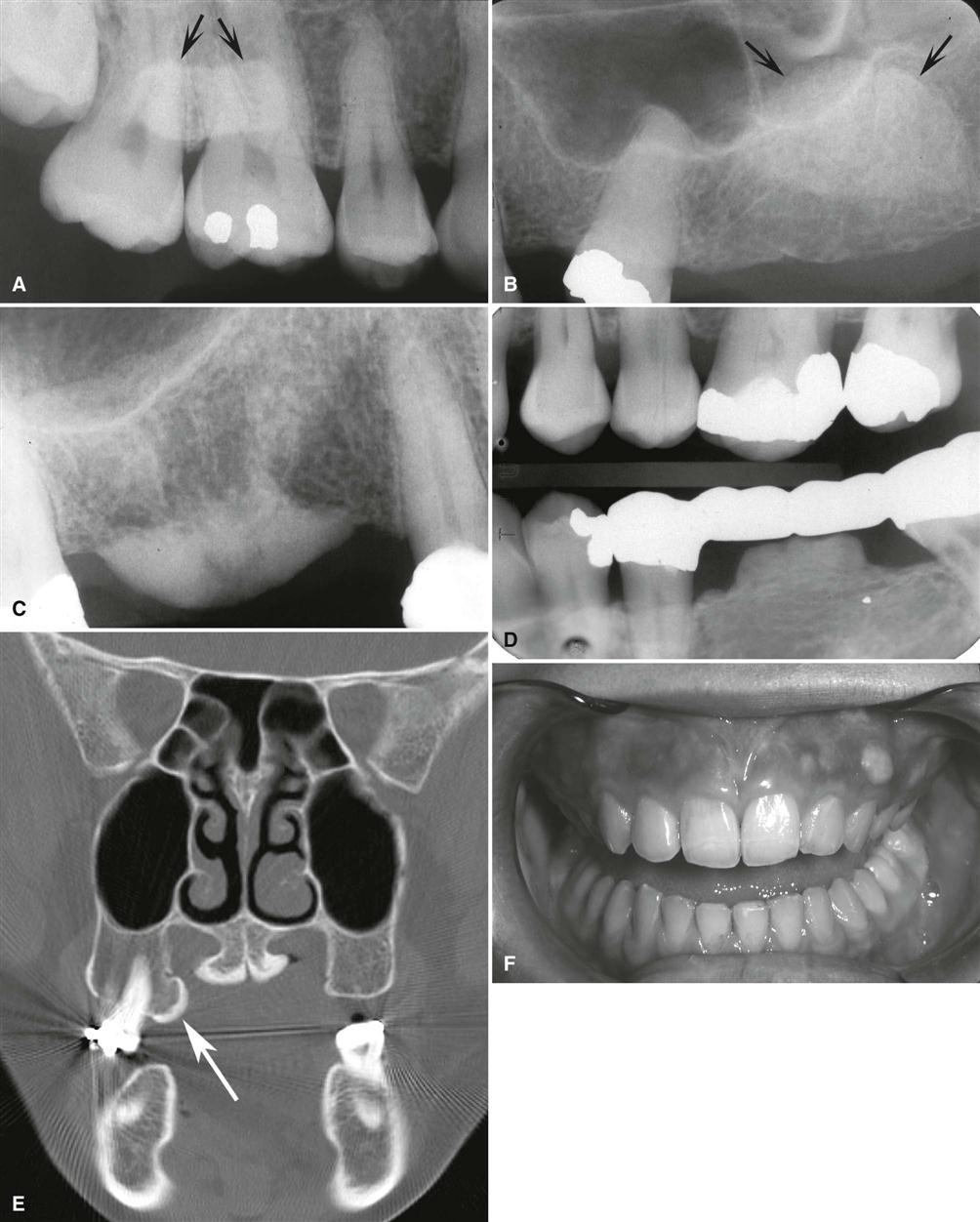
Location.
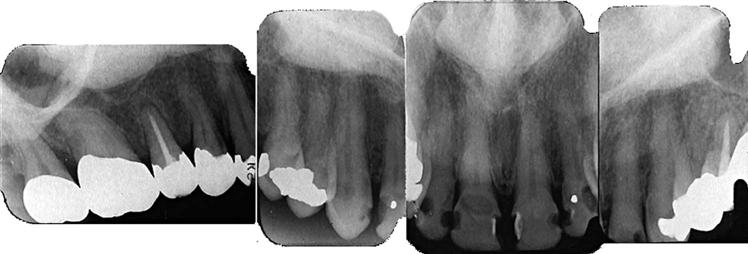
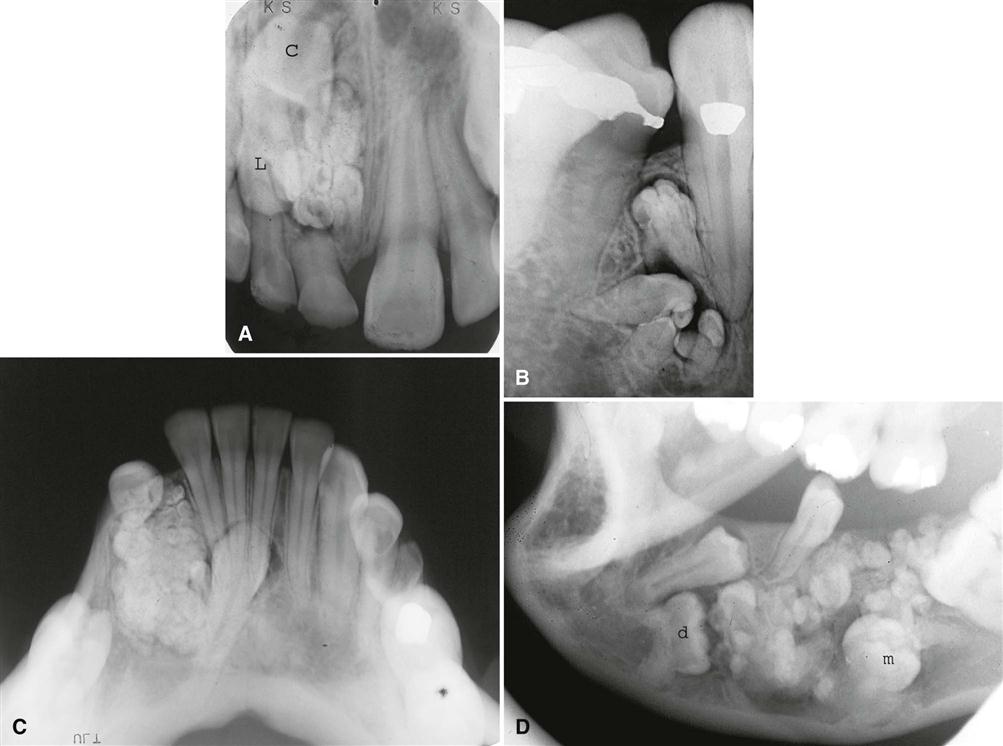
Most ameloblastomas (80%) develop in the molar-ramus region of the mandible, but they may extend to the symphyseal area. Most lesions that occur in the maxilla are in the third molar area and extend into the maxillary sinus and nasal floor. In either jaw, this tumor can originate in an occlusal position to a developing tooth (Fig. 22-11).
Periphery.
An ameloblastoma is usually well defined and frequently delineated by a cortical border. The border is often curved, and in small lesions the border and shape may be indistinguishable from a cyst (Fig. 22-12). The periphery of lesions in the maxilla is usually more ill defined.
Internal Structure.
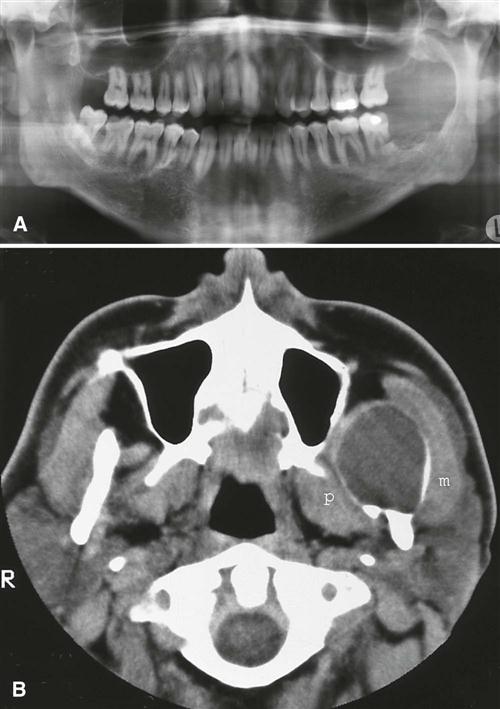
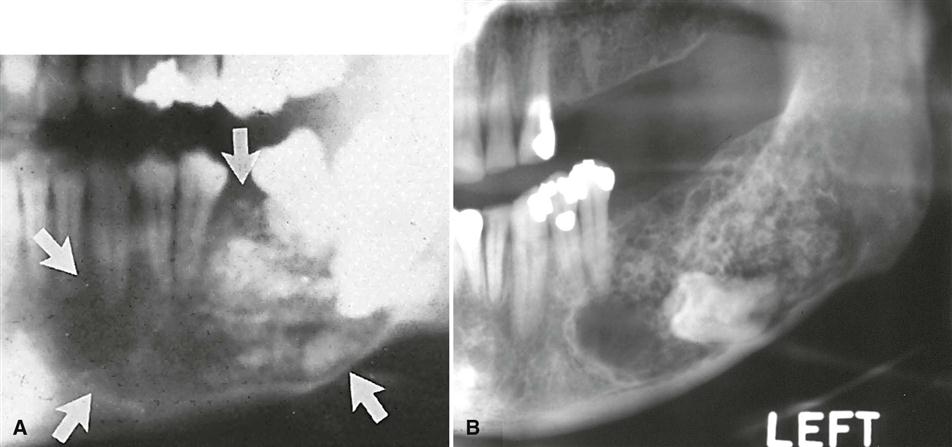
The internal structure varies from totally radiolucent (see Fig. 22-11) to mixed with the presence of bony septa creating internal compartments. These septa can be straight but are more commonly coarse and curved and originate from normal bone that has been trapped within the tumor. Because this tumor frequently has internal cystic components, these septa are often remodeled into curved shapes providing honeycomb (numerous small compartments or loculations) or soap bubble (larger compartments of variable size) patterns (see Fig. 22-12). Generally, the loculations are larger in the posterior mandible and smaller in the anterior mandible. In the desmoplastic variety, the internal structure can be composed of very irregular sclerotic bone resembling a bone dysplasia or bone-forming tumor (Fig. 22-13).
Effects on Surrounding Structures.
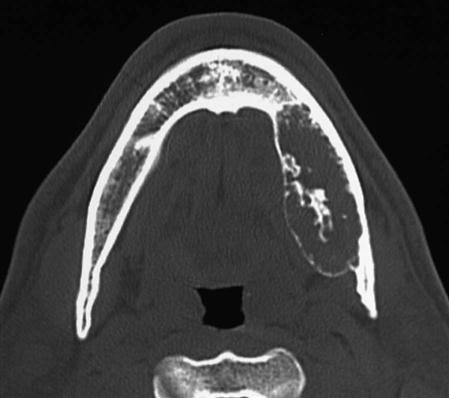
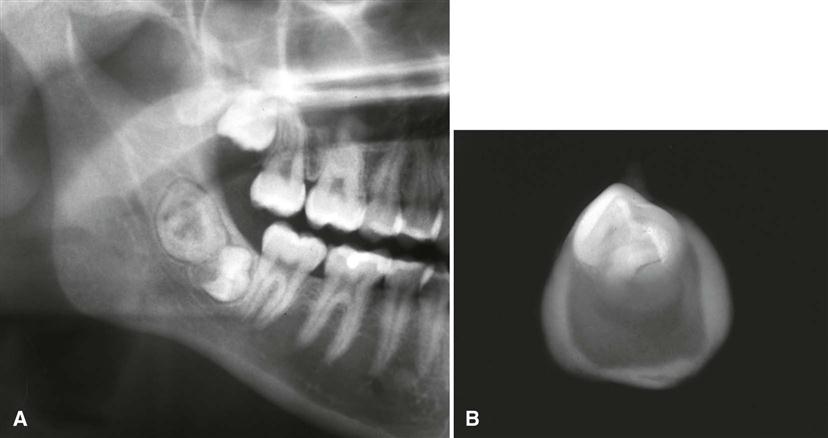
There is a pronounced tendency for ameloblastomas to cause extensive root resorption (Fig. 22-14). Tooth displacement is common. Because a common point of origin is occlusal to a tooth, some teeth may be displaced apically. An occlusal radiograph may demonstrate cystlike expansion and thinning of an adjacent cortical plate leaving a thin “eggshell” of bone (Fig. 22-15). CT images often reveal regions of perforation of the expanded cortical plate owing to the inability of the production of periosteal new bone to keep up with the rate of growth of the expanding ameloblastoma (Fig. 22-16). Unicystic types of ameloblastoma may cause extreme expansion of the mandibular ramus, and often the anterior border of the ramus is no longer visible in the panoramic image (Fig. 22-17).
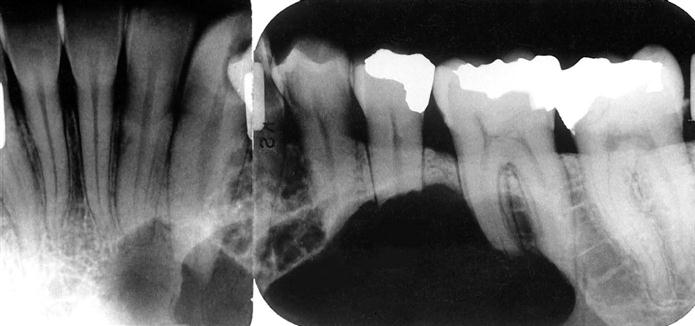
Recurrent Ameloblastoma.
Ameloblastomas may recur when the initial surgical procedure inadequately removes the entire tumor. Recurrent tumor has a characteristic appearance of multiple small cystlike structures with very coarse sclerotic cortical margins (Fig. 22-18) and sometimes separated by normal bone.
Additional Imaging.
If a preliminary diagnosis of ameloblastoma is made, multidetector CT (MDCT) imaging is highly recommended. MDCT imaging not only can confirm the diagnosis but also accurately demonstrates the anatomic extent of the tumor (see Fig. 22-16). In this regard, MDCT imaging has an advantage over cone-beam CT imaging in that it can display soft tissue structures (soft tissue algorithm) and can detect perforation of the outer cortex and invasion into the surrounding soft tissues. If soft tissue invasion is extensive, an MRI can provide superior images of the nature and extent of the invasion. CT examination is essential in the postsurgical follow-up assessment of ameloblastoma.
Differential Diagnosis.
Small unilocular ameloblastomas that are located around the crown of an unerupted tooth often cannot be differentiated from a dentigerous cyst. Because the appearance of the internal bony septa is important for the identification of ameloblastoma, other types of lesions that also have internal septa, such as odontogenic keratocyst, giant cell granuloma, odontogenic myxoma, and ossifying fibroma, may have a similar appearance. An odontogenic keratocyst may contain curved septa, but usually the keratocyst tends to grow along the bone without marked expansion, which is characteristic of ameloblastomas. Giant cell granulomas occur in a younger age group and have more granular or wispy ill-defined septa. Odontogenic myxomas may have similar-appearing septa; however, there are usually one or two thin sharp, straight septa, which is characteristic of the myxoma. The presence of even one such septum may indicate a myxoma. Also, myxomas are not as expansile as ameloblastomas and tend to grow along the bone. The septa in ossifying fibroma are usually wide, granular, and ill defined, and often there are small, irregular trabeculae.
Treatment.
The most common treatment is surgical resection. The surgical procedure should take into account the tendency of the neoplasm to invade adjacent bone beyond its apparent radiographic margins. MDCT imaging and MRI are useful in determining the exact extent of the tumor. If the ameloblastoma is relatively small, it may be removed completely by an intraoral approach, and larger lesions may require resection of the jaw. The maxilla is usually treated more aggressively because of the tendency of ameloblastoma to invade adjacent vital structures. Radiation therapy may be used for inoperable tumors, especially tumors in the posterior maxilla.
Calcifying Epithelial Odontogenic Tumor
Synonyms.
Synonyms for calcifying epithelial odontogenic tumor (CEOT) include Pindborg tumor and ameloblastoma of unusual type with calcification.
Disease Mechanism.
CEOTs are rare neoplasms. They account for about 1% of odontogenic tumors. These tumors usually are located within bone and produce a mineralized substance within amyloid-like material and contain strands or sheets of polyhedral epithelial cells in fibrous stroma.
Clinical Features.
A CEOT is less aggressive than an ameloblastoma and is found in about the same age group. Rarely this tumor may have an extraosseous location. The neoplasm is more common in men, and patients range in age from 8 to 92 years, with an average age of about 42 years (average age is considerably younger in men and older in women). Jaw expansion is a regular feature and usually the only symptom. Palpation of the swelling reveals a hard tumor.
Imaging Features
Location.
Similar to ameloblastomas, CEOTs have a definite predilection for the mandible, with a ratio of at least 2 : 1, and most develop in the premolar-molar area, with a 52% association with an unerupted or impacted tooth. In about half of cases, radiographs taken early in the development of these tumors reveal a radiolucent area around the crown of a mature, unerupted tooth.
Periphery.
The border may have a well-defined cystlike cortex. In some tumors, the boundary may be irregular and ill defined.
Internal Structure.
The internal aspect may appear unilocular or multilocular with numerous scattered, radiopaque foci of varying size and density. Some radiopaque elements may have a crescent shape or a doughnut shape with a radiolucent center. The most characteristic and diagnostic finding is the appearance of radiopacities close to the crown of the embedded tooth (Fig. 22-19). In addition, small, thin, opaque trabeculae may cross the radiolucency in many directions.
Effects on Surrounding Structures.
CEOTs may displace a developing tooth or prevent its eruption. Associated expansion of the jaw with maintenance of a cortical boundary may also occur.
Differential Diagnosis.
Lesions with a completely radiolucent internal structure may mimic dentigerous cysts or ameloblastomas. Other lesions with radiopaque foci, including adenomatoid odontogenic tumor, ameloblastic fibro-odontoma, and calcifying odontogenic cyst, may have similar appearances. However, the prominent location of the CEOT and the age of the patient help in the differential diagnosis.
Treatment.
The treatment of a CEOT is more conservative than treatment of an ameloblastoma, with local resection.
Mixed Odontogenic Tumors
Odontoma
Synonyms.
Compound odontoma, compound composite odontoma, complex odontoma, complex composite odontoma, odontogenic hamartoma, calcified mixed odontoma, and cystic odontoma are synonyms for odontoma.
Disease Mechanism.
The term odontoma is used to identify a tumor that is characterized by the production of mature enamel, dentin, cementum, and pulp tissue. These components are seen in various states of histodifferentiation and morphodifferentiation. Because of its limited and slow growth and well-differentiated tooth tissue, this lesion is considered to be a hamartoma and not a true tumor.
The structural relationship of the component tissues may vary from nondescript masses of dental tissue referred to as a complex odontoma to multiple well-formed teeth (denticles) of a compound odontoma. A dilated odontoma has been described as another type of odontoma; however, this is a single structure that actually may be the most severe expression of a dens in dentes.
Clinical Features.
Odontomas are the most common odontogenic tumor. They often interfere with the eruption of permanent teeth (Fig. 22-20). The lesion shows no gender predilection, and most begin forming while the normal dentition is developing. Odontomas develop and mature while the corresponding teeth are forming and cease development when the associated teeth complete development. Most odontomas occur in the second decade of life and many times are found during investigation of delayed eruption of adjacent teeth or retained primary teeth. In rare cases, odontomas are associated with primary teeth. They persist if left untreated, although they do not continue to increase in size and may be detected later in life. Compound odontomas are about twice as common as the complex type. Although the compound variety forms equally between men and women, 60% of complex odontomas occur in women. In rare circumstances, a compound odontoma may erupt into the oral cavity of a child.
Imaging Features
Location.
More of the compound type (62%) occurs in the anterior maxilla in association with the crown of an unerupted canine. In contrast, 70% of complex odontomas are found in the mandibular first and second molar area.
Periphery.
The borders of odontomas are well defined and may be smooth or irregular. These lesions have a cortical border, and immediately inside and adjacent to the cortical border is a soft tissue capsule.
Internal Structure.
The contents of these lesions are largely radiopaque. Compound odontomas have a number of toothlike structures or denticles that look like deformed teeth (Fig. 22-21). Complex odontomas contain an irregular mass of calcified tissue (see Fig. 22-20). The degree of radiopacity is equivalent to or exceeds adjacent tooth structure and may vary in the degree of radiopacity from one region to another, reflecting variations in amount and type of hard tissue that has been formed. A dilated odontoma has a single calcified structure with a more radiolucent central portion that has an overall form similar to a doughnut (Fig. 22-22).
Effects on Surrounding Structures.
Odontomas can interfere with the normal eruption of teeth. Most odontomas (70%) are associated with abnormalities, such as impaction, malpositioning, diastema, aplasia, malformation, and devitalization of adjacent teeth. Large complex odontomas may cause expansion of the jaw with maintenance of the cortical boundary.
Differential Diagnosis.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses