Cysts
Disease Mechanism
A cyst is a pathologic cavity filled with fluid, lined by epithelium, and surrounded by a definite connective tissue wall. Cysts occur more often in the jaws than in any other bone because most cysts originate from the numerous rests of odontogenic epithelium that remain after tooth formation. The cystic fluid either is secreted by the cells lining the cavity or is derived from the surrounding tissue fluid. The cyst has a spherical or round shape based on accumulation of fluid within the cavity. Without resistance, for example, within an air space such as the maxillary sinus, the cyst grows in a concentric fashion resulting in a spherical shape, but when growing within bone, its shape is influenced by the resistance of adjacent hard tissue. For instance, a water-filled balloon develops a flat side when placed on a table top; similarly, a cyst reaching a thick segment of cortical bone may develop a flat side.
Clinical Features
The most common clinical features are swelling and lack of pain (unless the cyst becomes secondarily infected or is related to a nonvital tooth). Cysts are often associated with unerupted teeth, especially third molars.
Imaging Features
Location
Cysts may occur centrally (within bone) in any location in the maxilla or mandible but are rare in the condyle and coronoid process. Odontogenic cysts are found most often in the tooth-bearing regions. In the mandible, they originate above the inferior alveolar nerve canal. Odontogenic cysts may grow into the maxillary sinus. Some nonodontogenic cysts also originate within the antrum (see Chapter 26). A few cysts arise in the soft tissues of the orofacial region.
Periphery
Cysts that originate in bone usually have a periphery that is well defined and corticated (characterized by a fairly uniform, thin, radiopaque line). However, a secondary infection or a chronic state can change this appearance into a thicker, more sclerotic boundary or make the cortex less apparent.
Shape
Cysts usually are round or oval, resembling a fluid-filled balloon. Some cysts may have a scalloped boundary.
Internal Structure
Cysts often are totally radiolucent. However, long-standing cysts may have dystrophic calcification, which can give the internal aspect a sparse, particulate appearance. Some cysts have septa, which produce multiple loculations separated by these bony walls or septa. Cysts that have a scalloped periphery may appear to have internal septa. Occasionally, bony ridges produced by the peripheral scalloping are positioned so that their image overlaps the internal aspect of the cyst, giving the false impression of internal septa.
Effects on Surrounding Structure
Cysts grow slowly, sometimes causing displacement and resorption of teeth. The resorbing root often has a sharp, curved border. Cysts can expand the mandible, usually in a smooth, curved manner, and change the buccal or lingual cortical plate into a thin cortical boundary. Cysts may displace the inferior alveolar nerve canal in an inferior direction or expand into the maxillary antrum, maintaining a thin layer of bone separating the internal aspect of the cyst from the antrum.
Odontogenic Cysts
Radicular Cyst
Synonyms
Synonyms for radicular cyst include periapical cyst, apical periodontal cyst, and dental cyst.
Disease Mechanism
A radicular cyst is a cyst that most likely results when rests of epithelial cells (Malassez) in the periodontal ligament are stimulated to proliferate and undergo cystic degeneration by inflammatory products from a nonvital tooth. This cyst is thought to grow by osmotic pressure.
Clinical Features
Radicular cysts are the most common type of cyst in the jaws. They arise from nonvital teeth (i.e., teeth that have necrotic pulps because of extensive caries, large restorations, or previous trauma). Radicular cysts often produce no symptoms unless secondary infection occurs. A cyst that becomes large may cause swelling. On palpation, the swelling may feel bony and hard if the cortex is intact, crepitant as the bone thins, and rubbery and fluctuant if the outer cortex is perforated. The incidence of radicular cysts is greater in the third to sixth decades and shows a slight male predominance.
Imaging Features
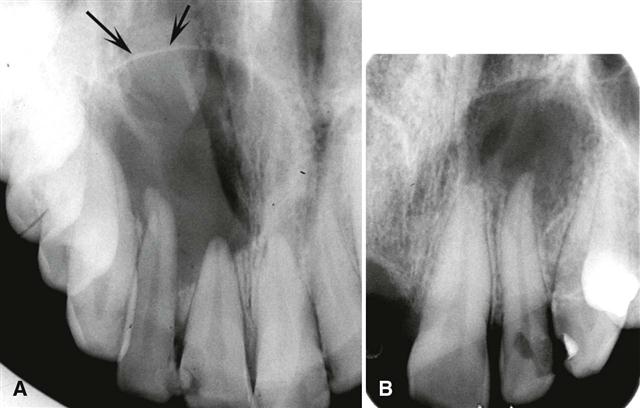
Location.
In most cases, the epicenter of a radicular cyst is located approximately at the apex of a nonvital tooth (Fig. 21-1). It occasionally appears on the mesial or distal surface of a tooth root at the opening of an accessory canal or infrequently in a deep periodontal pocket. Most radicular cysts (60%) are found in the maxilla, especially around incisors and canines. Because of the distal inclination of the root, cysts that arise from the maxillary lateral incisor may expand into or invaginate the antrum. Radicular cysts may also form in relation to a nonvital deciduous molar and be positioned buccal to the developing bicuspid.
Periphery and Shape.
The periphery usually has a well-defined cortical border (Fig. 21-2). If the cyst becomes secondarily infected, the inflammatory reaction of the surrounding bone may result in loss of this cortex (see Fig. 21-1, B) or alteration of the cortex into a more sclerotic border. The outline of a radicular cyst usually is curved or circular, unless it is influenced by surrounding structures such as cortical boundaries.
Internal Structure.
In most cases, the internal structure of radicular cysts is radiolucent. Occasionally, dystrophic calcification may develop in long-standing cysts, appearing as sparsely distributed, small particulate radiopacities.
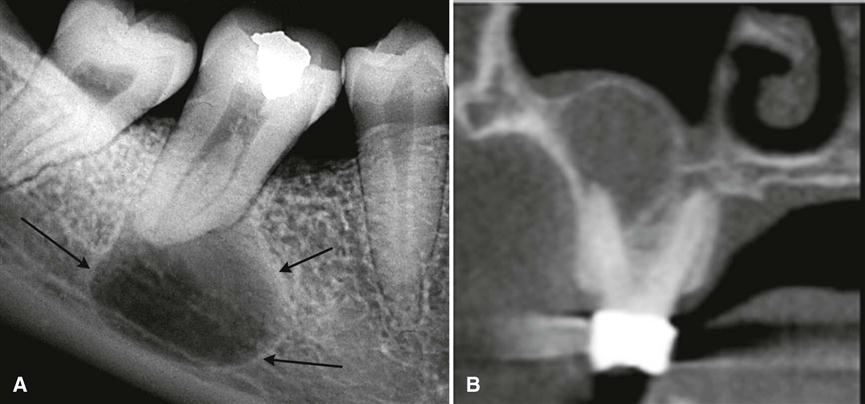
Effects on Surrounding Structures.
If a radicular cyst is large, displacement and resorption of the roots of adjacent teeth may occur. The resorption pattern may have a curved outline. In rare cases, the cyst may resorb the roots of the related nonvital tooth. The cyst may invaginate the sinus, but there typically is evidence of a cortical boundary between the contents of the cyst and the sinus cavity (see Fig. 21-2, B). The outer cortical plates of the maxilla or mandible may expand in a curved or circular shape (Fig. 21-3). Cysts may displace the mandibular alveolar nerve canal in an inferior direction.
Differential Diagnosis
Differentiation of a small radicular cyst from an apical granuloma or a periapical pocket cyst may be difficult or impossible in some cases. A round shape, a well-defined cortical border, and a size greater than 2 cm in diameter are more characteristic of a cyst. Other periapical radiolucencies to consider are an early stage of periapical osseous (cemental) dysplasia and an apical scar or a surgical defect because normal bone may never fill in the defect completely in such cases. The patient’s history helps with the differentiation. Radicular cysts that originate from the maxillary lateral incisor and are positioned between the roots of the lateral incisor and the cuspid may be difficult to differentiate from a keratocystic odontogenic tumor (KOT), also known as odontogenic keratocyst, or a lateral periodontal cyst. The vitality of the involved tooth should be tested. A nonvital tooth may have a larger pulp chamber than neighboring teeth because of the lack of secondary dentin, which normally forms with time in the pulp chamber and canal of a vital tooth (see Fig. 21-1).
A large radicular cyst that has invaginated the maxillary antrum may collapse and start filling in with new bone (Fig. 21-4). With biopsy, the histologic analysis may result in an erroneous diagnosis of ossifying fibroma or a benign fibro-osseous lesion. Radiographically, the important feature is that the new bone always forms first at the periphery of the cyst wall and grows toward the center as the cyst shrinks; this is a different pattern of bone formation than is seen with benign bone-forming lesions.
Management
Treatment of a tooth with a radicular cyst may include extraction, endodontic therapy, and apical surgery. Treatment of a large radicular cyst usually involves surgical removal or marsupialization. The radiographic appearance of the periapical area of an endodontically treated tooth should be checked periodically to ensure that normal healing is occurring (Fig. 21-5). Characteristically, new bone grows into the defect from the periphery, sometimes resulting in a radiating pattern resembling the spokes of a wheel. However, in a few cases, normal bone may not completely fill the defect, especially if there was a secondary infection or a considerable amount of bone destruction, including the buccal and lingual cortical plates. Recurrence of a radicular cyst is unlikely if it has been removed completely.
Residual Cyst
Disease Mechanism
A residual cyst is a cyst that remains after incomplete removal of the original cyst. The term residual is used most often for a radicular cyst that may be left behind, most commonly after extraction of a tooth.
Clinical Features
A residual cyst usually is asymptomatic and often is discovered on radiographic examination of an edentulous area. However, there may be some expansion of the jaw or pain in the case of secondary infection.
Imaging Features
Location.
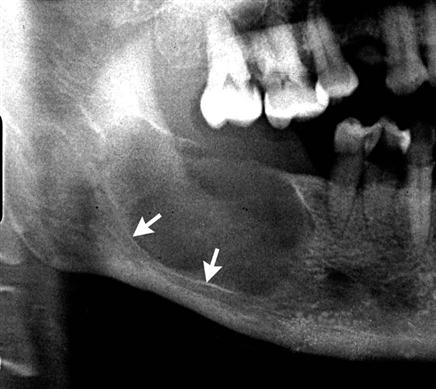
Residual cysts occur in both jaws, although they are found slightly more often in the mandible. The epicenter is positioned in the former periapical region of the involved and missing tooth. In the mandible, the epicenter is always above the inferior alveolar nerve canal (Fig. 21-6).
Periphery and Shape.
A residual cyst has a cortical margin, unless it becomes secondarily infected. Its shape is oval or circular.
Internal Structure.
The internal aspect of a residual cyst typically is radiolucent. Dystrophic calcifications may be present in long-standing cysts.
Effects on Surrounding Structures.
Residual cysts can cause displacement or resorption of teeth, or they may cause expansion of the outer cortical plates of the jaws. The cyst may invaginate into the maxillary antrum or depress the inferior alveolar nerve canal.
Differential Diagnosis
Without the patient’s history and previous radiographs, clinicians may have difficulty determining whether a solitary cyst in the jaws is a residual cyst. Other examples of common solitary cysts include KOTs. A residual cyst has greater potential for expansion compared with a KOT. The epicenter of a Stafne developmental salivary gland defect is located below the mandibular canal (and thus is unlikely to be odontogenic in nature).
Management
The treatment for residual cysts is surgical removal or marsupialization, or both if the cyst is large.
Dentigerous Cyst
Synonym
Follicular cyst is a synonym for dentigerous cyst.
Disease Mechanism
A dentigerous cyst is a cyst that forms around the crown of an unerupted tooth. It begins when fluid accumulates in the layers of reduced enamel epithelium or between the epithelium and the crown of the unerupted tooth. This lesion is usually classified as a developmental cyst, but some evidence suggests that in a few cases inflammation may be the etiology. An eruption cyst is the soft tissue counterpart of a dentigerous cyst.
Clinical Features
Dentigerous cysts are the second most common type of cyst in the jaws. They develop around the crown of an unerupted or supernumerary tooth. The clinical examination reveals a missing tooth or teeth and possibly a hard swelling, occasionally resulting in facial asymmetry. The patient typically has no pain or discomfort. Dentigerous cysts around supernumerary teeth account for about 5% of all dentigerous cysts, most developing around a mesiodens in the anterior maxilla.
Imaging Features
Location.
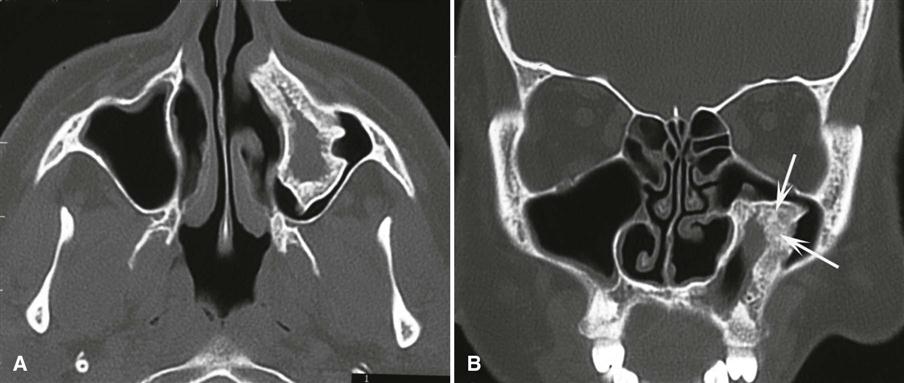
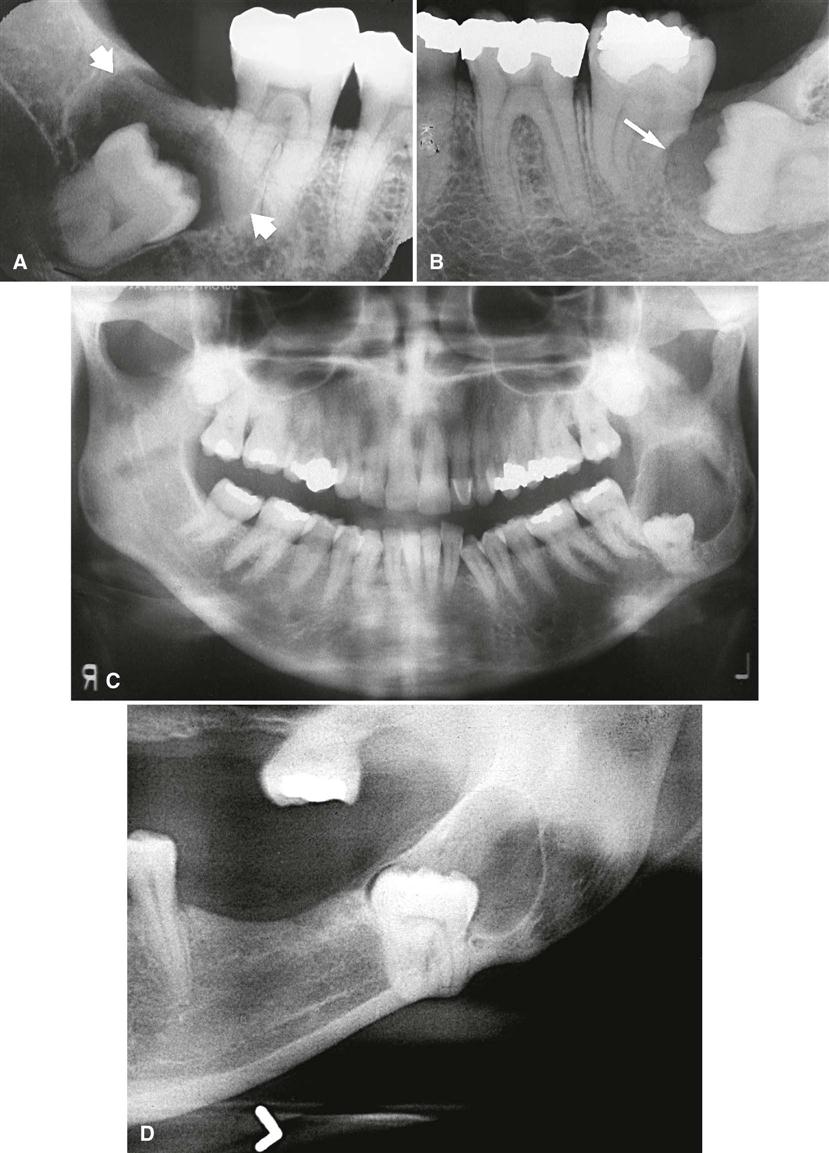
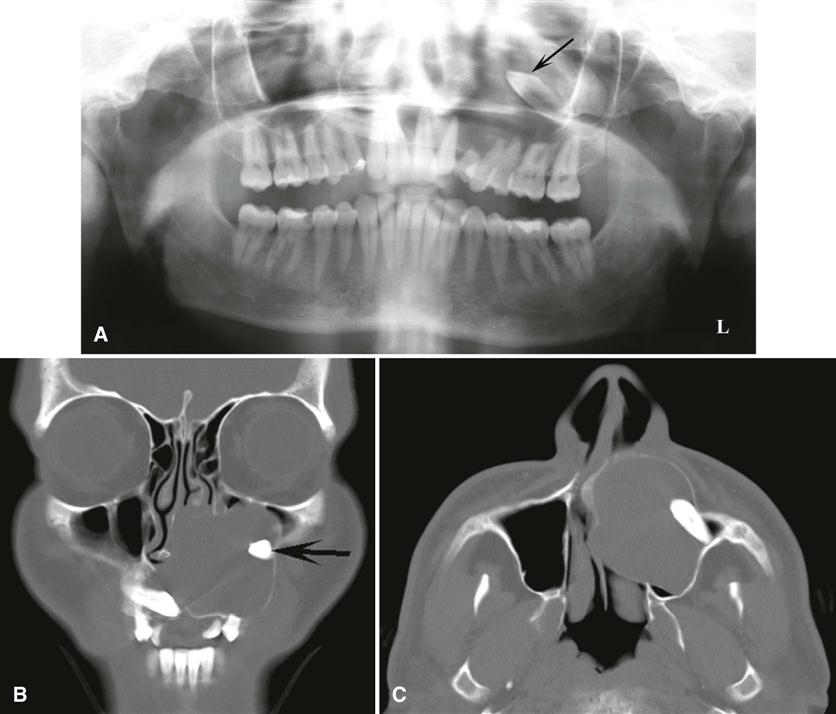
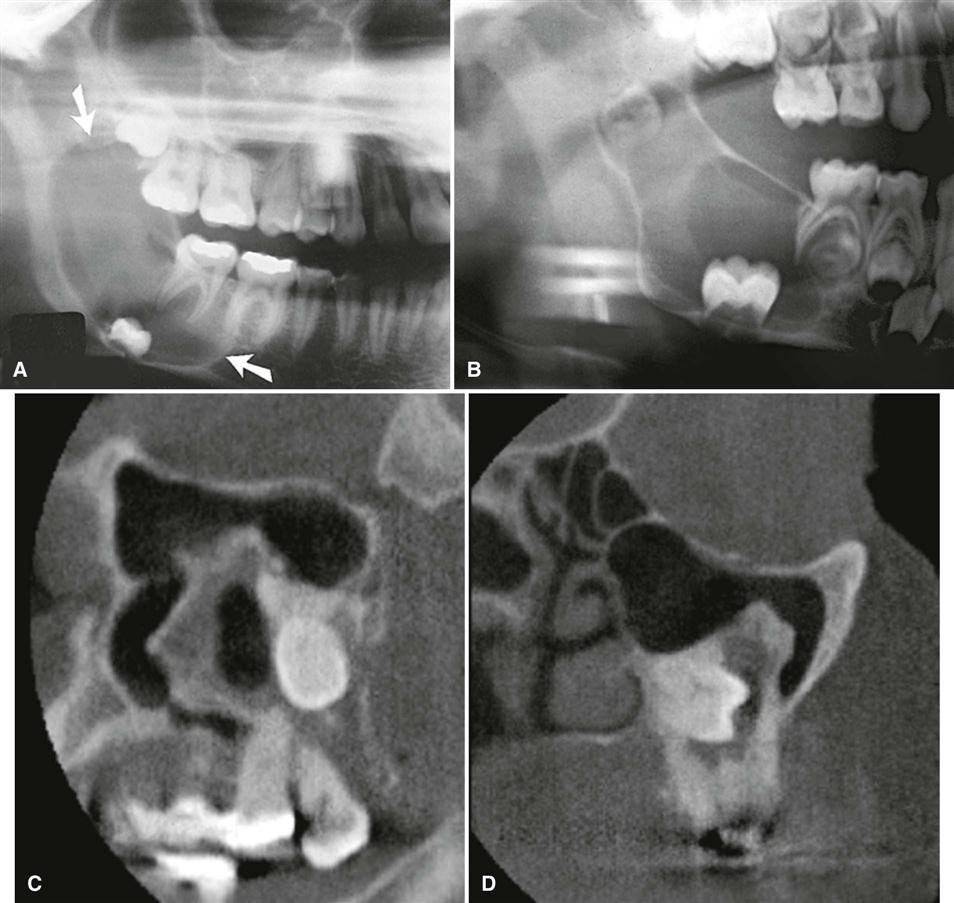
The epicenter of a dentigerous cyst is found just above the crown of the involved tooth, most commonly a mandibular or maxillary third molar or a maxillary canine (Fig. 21-7). An important diagnostic point is that this cyst attaches at the cementoenamel junction. Some dentigerous cysts are eccentric, developing from the lateral aspect of the follicle so that they occupy an area beside the crown instead of above the crown (see Fig. 21-7, D). Cysts related to maxillary third molars often grow into the maxillary antrum and may become quite large before they are discovered. Cysts attached to the crown of mandibular molars may extend a considerable distance into the ramus.
Periphery and Shape.
Dentigerous cysts typically have a well-defined cortex with a curved or circular outline. If infection is present, the cortex may be missing.
Internal Structure.
The internal aspect is completely radiolucent except for the crown of the involved tooth.
Effects on Surrounding Structures.
A dentigerous cyst has a propensity to displace and resorb adjacent teeth (Fig. 21-8; see Fig. 21-7). It commonly displaces the associated tooth in an apical direction (Fig. 21-9). The degree of displacement may be considerable. For instance, maxillary third molars or cuspids may be pushed to the floor of the orbit (see Fig. 21-8), and mandibular third molars may be moved to the condylar or coronoid regions or to the inferior cortex of the mandible. The floor of the maxillary antrum may be displaced as the cyst invaginates the antrum, or a cyst may displace the inferior alveolar nerve canal in an inferior direction (Fig. 21-10). This slow-growing cyst often expands the outer cortical boundary of the involved jaw. As in the case with radicular cysts, dentigerous cysts that invaginate the sinus can drain and collapse with new bone formation at the periphery (see Fig. 21-10, C and D).
Differential Diagnosis
Because the histopathologic appearance of the lining epithelium is not specific, the diagnosis relies on the radiographic and surgical observation of the attachment of the cyst to the cementoenamel junction. However, histopathologic examination must always be done to eliminate other possible lesions in this location.
One of the most difficult differential diagnoses to make is between a small dentigerous cyst and a hyperplastic follicle. A cyst should be considered with any evidence of tooth displacement or considerable expansion of the involved bone. The size of the normal follicular space is 2 to 3 mm. If the follicular space exceeds 5 mm, a dentigerous cyst is more likely. If uncertainty remains, the region should be reexamined in 4 to 6 months to detect any increase in size or any influence on surrounding structures characteristic of cysts.
The differential diagnosis of a dentigerous cyst also may include a KOT, an ameloblastic fibroma, and a cystic ameloblastoma. A KOT does not expand the bone to the same degree as a dentigerous cyst, is less likely to resorb teeth, and may attach further apically on the root instead of at the cementoenamel junction. It may be impossible to differentiate a small ameloblastic fibroma or cystic ameloblastoma from a dentigerous cyst if there is no internal structure. Other rare lesions that may have a similar pericoronal appearance are adenomatoid odontogenic tumors and calcified odontogenic cysts, both of which can surround the crown and root of the involved tooth. Evidence of a radiopaque internal structure is sometimes found in these two lesions. Occasionally, a radicular cyst at the apex of a primary tooth surrounds the crown of the developing permanent tooth positioned apical to it, giving the false impression of a dentigerous cyst associated with the permanent tooth. This occurs most often with the mandibular deciduous molars and the developing bicuspids. In these cases, the clinician should look for extensive caries or large restorations in a primary tooth, an etiology that would support a diagnosis of a radicular cyst.
Management
Dentigerous cysts are treated by surgical removal, which may include the tooth as well. Large cysts may be treated by marsupialization before removal. The cyst lining should be submitted for histologic examination because ameloblastomas have been reported to occur there. In addition, squamous cell carcinoma and mucoepidermoid carcinoma have been reported to arise from the cyst lining of chronically infected cysts.
Buccal Bifurcation Cyst
Synonyms
Synonyms for buccal bifurcation cyst (BBC) include mandibular infected buccal cyst, paradental cyst, and inflammatory paradental cyst.
Disease Mechanism
BBCs probably derive from the epithelial cell rests in the periodontal membrane of the buccal bifurcation of mandibular molars. The histopathologic characteristics of the lining are not distinctive. The etiology of proliferation is unknown; one theory holds that inflammation is the stimulus, but inflammation is not always present. The World Health Organization includes these cysts under inflammatory cysts.
It is possible that the paradental cyst of the third molar and the BBC (associated with first and second molars) are the same entity. The BBC is certainly a distinct clinical entity. An associated enamel extension into the furcation region of third molars with paradental cysts has not been documented with molars involved in a BBC. Also, the inflammatory component associated with paradental cysts is not always present with BBCs.
Clinical Features
A common sign is the lack of or a delay in eruption of a mandibular first or second molar. On clinical examination, the molar may be missing, or the lingual cusp tips may be abnormally protruding through the mucosa, higher than the position of the buccal cusps. The first molar is involved more frequently than the second molar. The teeth are vital. A hard swelling may occur buccal to the involved molar, and if it is secondarily infected, the patient has pain. The age of detection is younger, within the first 2 decades for a BBC, rather than the third decade with a paradental cyst of the third molar.
Imaging Features
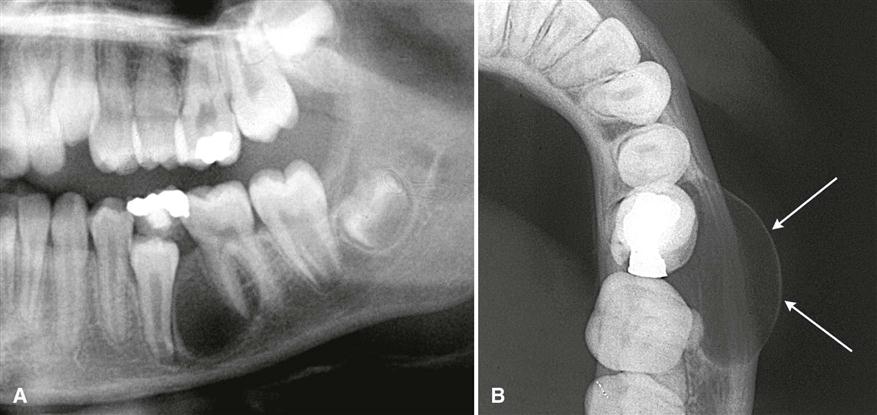
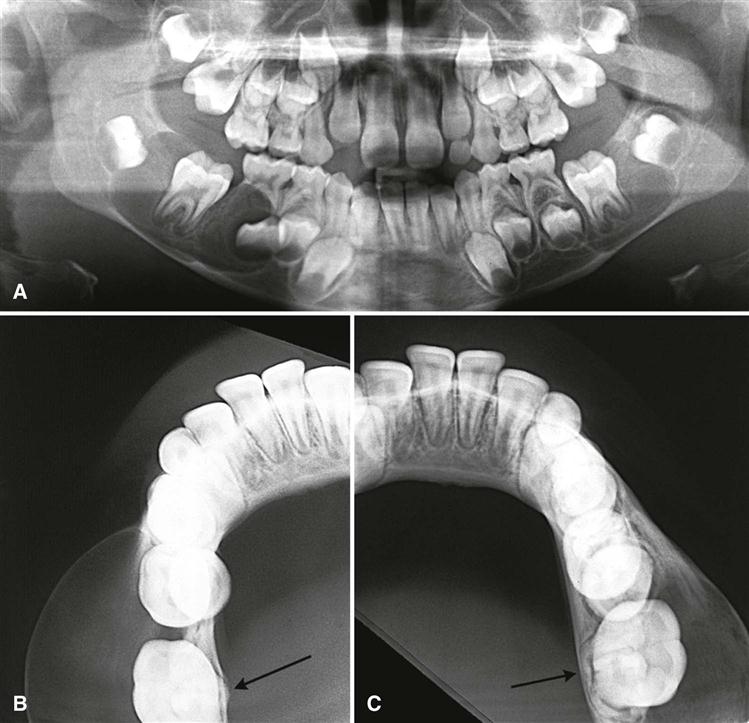
Location.
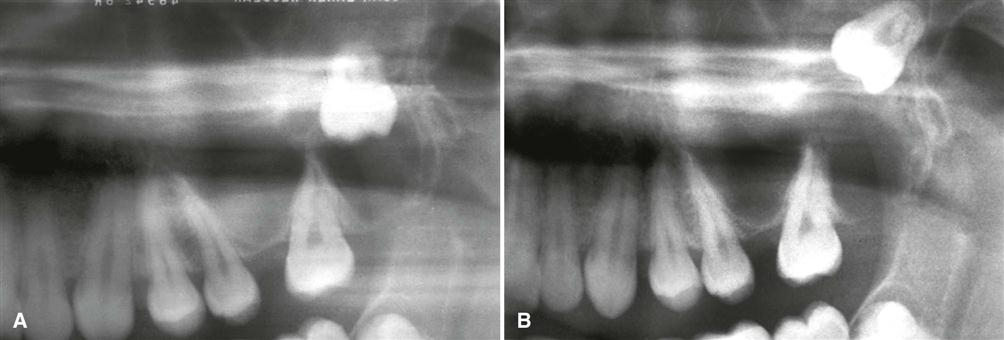
A BBC is most commonly located in association with a mandibular first molar followed by the second molar. The cyst occasionally is bilateral. It is always located in the buccal furcation of the affected molar (Fig. 21-11). On periapical and panoramic films, the lesion may appear to be centered a little distal to the furcation of the involved tooth.
Periphery and Shape.
In some cases, the periphery is not readily apparent, and the lesion may be a very subtle radiolucent region superimposed over the image of the roots of the molar. In other cases, the lesion has a circular shape with a well-defined cortical border. Some cysts can become quite large before they are detected.
Internal Structure.
The internal structure is radiolucent.
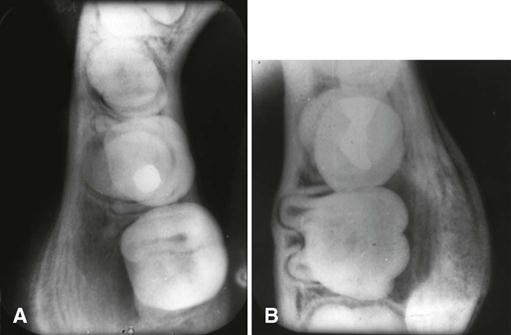
Effects on Surrounding Structures.
The most striking diagnostic characteristic of a BBC is the tipping of the involved molar so that the root tips are pushed into the lingual cortical plate of the mandible (see Fig. 21-11, B and C) and the occlusal surface is tipped toward the buccal aspect of the mandible (see Fig. 21-11, A). This accounts for the lingual cusp tips being positioned higher than the buccal tips. This tipping may be detected in a panoramic or periapical film if the image of the occlusal surface of the affected tooth is apparent and the unaffected teeth are not. The best diagnostic film is the cross-sectional (standard) mandibular occlusal projection, which demonstrates the abnormal position of the tooth roots. If the cyst is large enough, it may displace and resorb the adjacent teeth and cause a considerable amount of smooth expansion of the buccal cortical plate. If the cyst is secondarily infected, periosteal new bone formation is seen on the buccal cortex adjacent to the involved tooth (Fig. 21-12).
Differential Diagnosis
Diagnosis of a BBC relies entirely on clinical and radiographic information. The major differe/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses