Occlusion
Learning Objectives
• Define and pronounce the key terms in this chapter.
• Outline Angle’s classification of malocclusion and how it relates to patient care.
New Key Terms
Balancing interference (bruk-sizm)
Bracing (bruk-sizm)
Bruxism (bruk-sizm)
Canine rise (kay-nine)
Centric relation, stops (dis-tl)
Clenching (dis-tl)
Crossbite (dis-tl)
Curve of Spee, Wilson (dis-tl)
Distal step (dis-tl)
End-to-end bite (nath-ick)
Flush terminal plane (nath-ick)
Gnathic index (nath-ick)
Group function (in-ter-lay-be-al)
Interlabial gap (in-ter-lay-be-al)
Interocclusal clearance (in-ter- ah-kloo-zhal)
Leeway space (mal-ah-kloo-zhun): Angle’s classification of, Class I, Class II (division I, division II), Class III
Malocclusion (mal-ah-kloo-zhun): Angle’s classification of, Class I, Class II (division I, division II), Class III
Mesial/ step (me-ze-il)
Mesognathic (me-so-nath-ik)
Occlusal trauma (ah-klooz-l)
Occlusion (ah-kloozh-n): centric, lateral, primary, protrusive
Open bite (my-oh-funk-shun-al), therapy
Orofacial myofunctional disorders (my-oh-funk-shun-al), therapy
Orofacial myology (my-ol-oh-je)
Overbite (pare-ah-funk-shun-al)
Overjet (pare-ah-funk-shun-al)
Parafunctional habits (pare-ah-funk-shun-al)
Premature contacts (prog-nath-ik)
Prognathic (prog-nath-ik)
Range of motion (ret-row-nath-ik)
Retrognathic (ret-row-nath-ik)
Resting posture (kusp)
Side: balancing, working (kusp)
Supporting cusps (kusp)
Terminal plane
Tongue thrusting
Underbite
Occlusion
Occlusion is the contact relationship between the maxillary teeth and mandibular teeth when the jaws are in a fully closed (occluded) position, as well as the relationship between the teeth in the same arch. Many patterns of tooth contact are possible; part of the reason for the variety is the substantial range of movement of the mandibular condyle within the temporomandibular joint (TMJ) (see Figure 19-9).
Occlusion develops in a child as the primary teeth erupt. During this time, oral motor behaviors develop and the masticatory skills are acquired. The deglutition skills to accommodate the mastication process begin to develop in utero, and are modified on a developmental continuum as the primary dentition erupts. Occlusion of the erupting permanent dentition is dependent on the primary teeth shedding, with the exception of the permanent molars, as these erupt distal to the primary dentition.
Interrelated factors are involved in the development of the occlusion, such as the associated musculature, neuromuscular patterns, TMJ functioning (see Chapter 19), tongue functioning and posturing, orofacial behaviors, and habit patterns. Thus, occlusion is only one aspect of an entire developing orofacial masticatory and deglutition system that includes many other factors and variables. The teeth, in proper alignment, are relatively self-cleansing by action of the cheek and lip musculature, with the neutralizing flow of saliva over the smooth tooth surfaces.
When the teeth in the dentition are not aligned properly, or there are orofacial myofunctional imbalances and/or parafunctional habit patterns present, they lose the ability to self cleanse. More importantly, when teeth of either dentition are not occluding properly, the teeth and periodontium may not be able to perform the functions for which they were designed. Unnatural occlusal stress is then placed on the dentition, which often results in occlusal disharmony. Occlusal disharmony may then lead to occlusal trauma.The dentition and the periodontium are able to withstand many of these daily stresses; however, these stresses are often excessive, such as with incorrect tongue, lip, and/or mandibular resting posture patterns and/or parafunctional habits (discussed later). Microscopic changes within the periodontium can occur with occlusal trauma (see Figures 14-33 and 14-34).
Dental professionals must remember that occlusal trauma does not directly cause bacterial- based periodontal disease, but may create an overriding adverse force factor in initiating or contributing to an already weakened and diseased periodontium. It also may be associated, on an acute basis, with the production of a cracked tooth from masticatory impact on a hard object, and fracture of the restoration margin may also occur. Occlusal trauma can usually be stopped if the etiological factors are eliminated, or if the involved teeth are protected from these stresses.
Unfortunately, the effects of occlusal trauma are often irreversible, if not intercepted early enough. These occlusal disharmonies, orofacial myofunctional patterns, and parafunctional habits should be controlled or eliminated during dental treatment and preventive maintenance therapy before initiating occlusal therapy (see later discussion). Signs or symptoms indicating abnormal patterns and habits must be addressed to eliminate the harmful occlusal disharmonies on a long-term basis. The effects on a patient’s occlusion must also be kept in mind during all phases of dental treatment, especially during restorative treatment or when treating a temporomandibular disorder (TMD) (see Chapter 19).
Normal Occlusion
An ideal occlusion rarely exists, but the concept of a normal occlusion provides a basis for treatment. The optimum 138 occlusal contacts for the permanent dentition in the closure of 32 teeth are seldom, if ever, achieved. When occlusion is considered, the position of the dentition in centric occlusion serves as the basis for reference (discussed next). Thus, centric occlusion serves as the standard for describing a normal occlusion. Ideally, a normal centric resting posture of the tongue, lips, and mandible is also present (discussed later). To prevent occlusal disharmony, all patients should have an occlusal evaluation before and after completion of their dental treatment plan, with reevaluation occurring on a regular basis (see the Workbook for Illustrated Dental Embryology, Histology, and Anatomy for guidelines and techniques).
Centric Occlusion
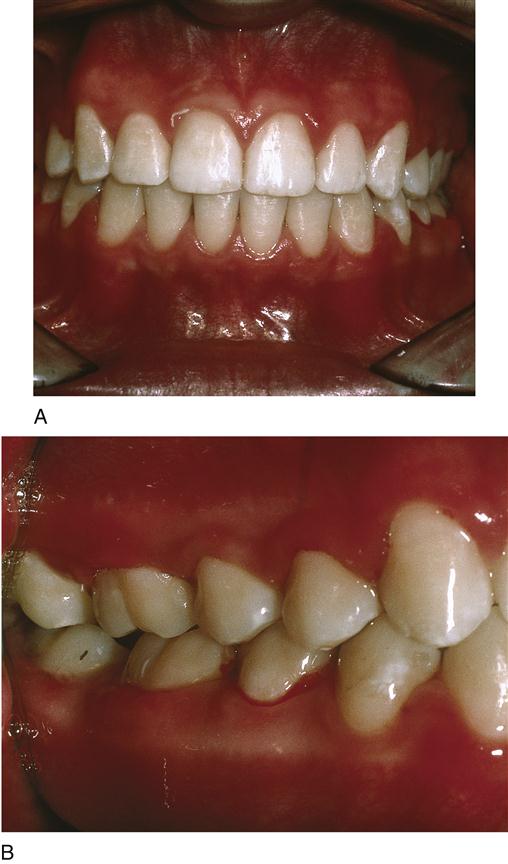
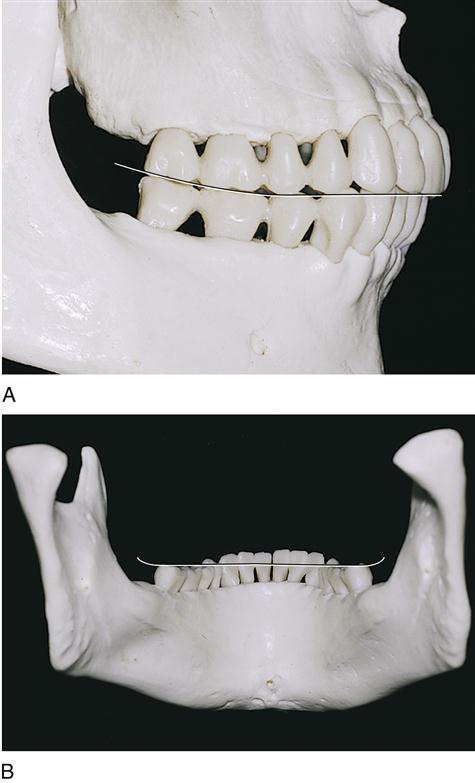
Centric occlusion (CO),or habitual occlusion, is the voluntary position of the dentition that allows the maximum contact when the teeth occlude (Figure 20-1). It is the centered contact position of the occlusal surfaces of mandibular teeth on the occlusal surface of the maxillary teeth. CO is related to the functioning of the dentition. However, even when the teeth are in full closure, discrepancy between the relationships of the mandible, TMJs, and/or the maxilla may be significant (skeletal discrepancies are discussed later).
When the teeth of a normal occlusion are in the position of CO, each tooth of one arch is in occlusion with two others in the opposing arch, except for the mandibular central incisors and maxillary third molars. This structure serves to equalize the forces of impact in occlusion. Another benefit of this arrangement is that if a tooth is lost in one jaw, the alignment of the opposing jaw is not immediately disturbed or impaired. One antagonist remains until adequate restorative treatment can be performed.
If a tooth is lost for a longer period, the neighboring teeth usually tip in an effort to fill the edentulous space. The teeth become inclined, malaligned, and supereruption of the tooth opposing the space then occurs (see Figures 17-43 and 17-55). Thus, loss of one tooth disturbs the contact relationships in that area, as well as those teeth in the opposing arch, their antagonist(s), possibly causing changes in the occlusion of the entire dentition. Patients must understand when discussing tooth replacement that teeth are like building blocks: Pull one out of the construction, and they all fall down, possibly resulting in occlusal disharmonies.
In addition to tooth loss, abnormal pressure or force of movement from the tongue, such as in tongue thrusting or an incorrect resting posture of the tongue, may create occlusal disharmony. An open mouth resting posture of the lips or chronic mouth breathing result in inadequate closure of the lips needed to maintain an equilibrium between the lips and teeth as well as the surrounding orofacial structures. This most often leads to the teeth not being retained in a normal arch shape and thus malocclusion occurs (discussed later).
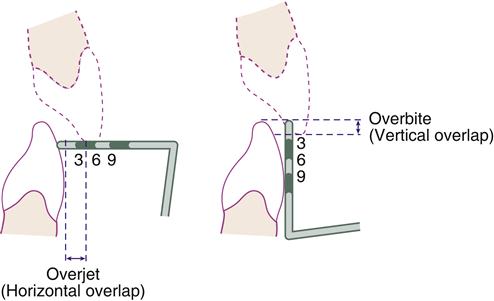
When the teeth normally occlude in CO, the maxillary arch horizontally overlaps the mandibular arch, a position called overjet (Figure 20-2). This normal amount of horizontal overlap, usually 1 to 3 mm, between the anterior segment of the two arches associated with the overjet allows extensions in the movement of the range of motion (ROM) of the mandible, and assists in keeping the soft tissue of the oral cavity out of the way during mastication. The ROM is a normal physiological and functional reciprocal ROM for opening or closure of the mandible.
Overjet is measured in millimeters with the tip of a periodontal probe, once a patient is in centric occlusion. The probe is placed at a right angle to the labial surface of a mandibular incisor at the base of the incisal edge of a maxillary incisor. The measurement is taken from the labial surface of the mandibular incisor to the lingual surface of the maxillary incisor. Note that the labiolingual width of the maxillary incisor is not included in the measurement.
In centric occlusion, the maxillary arch also vertically overlaps the mandibular arch, a position called overbite (see Figure 20-2). This normal amount of vertical overlap, normally 2 to 5 mm between the anterior segment of the two arches allows contact between the posterior teeth during mastication. It is usually expressed as a percentage at around 20-30%. Excessive amounts of either overjet or overbite are classified as a malocclusion (discussed later, see Figures 20-21, A and 20-22, A).
Overbite is measured in millimeters with the tip of a periodontal probe after a patient is placed in CO. The probe is placed on the incisal edge of the maxillary incisor at right angles to the mandibular incisor. As patients open their mouths or depress their jaws, the probe is then placed vertically against the mandibular incisor to measure the distance to the incisal edge of the mandibular incisor.
Studies show that overjet measurements were equally distributed among women and men, but overbite was noted more often in women. However, neither measurement was predictably associated with any particular craniofacial pattern. Both overjet and overbite tend to diminish with age, initially because of mandibular growth and later overbite due to incisal wear. When the reverse is the case, and the mandibular arch extends forward beyond the maxillary arch, the condition is referred to as an underbite (or retrognathia) (see Figure 20-26, B).
Within each dental arch, the teeth also create contact areas as they contact their same-arch neighbors on their proximal surfaces; the exception is the last tooth in each arch of each dentition, which lacks a distal contact (see Chapters 16 and 17). This contact between neighboring teeth serves two purposes: It protects the interdental papillae and stabilizes each tooth in the dental arch.
Open contacts allow areas of food impaction from opposing cusps, called plunging cusps, resulting in trauma to the interdental gingiva. Open contacts also do not allow mesiodistal stability between the teeth. Correct restorative treatment should not allow any open contacts, unless tooth position and tooth loss make this impossible. Although the practice is controversial, periodontal splints are often placed in the mouth lingually with tooth-colored resins and wires to simulate this stability needed for the teeth within the dental arch. All prosthetic treatment within the mouth, including the placement of bridges, implants, and removable dentures, is an attempt to simulate this stability.
Certain topics must be considered when studying CO: arch form and its development, dental curvatures and angulations, centric stops, centric relation, lateral and protrusive occlusion, mandibular rest position, and chewing patterns.
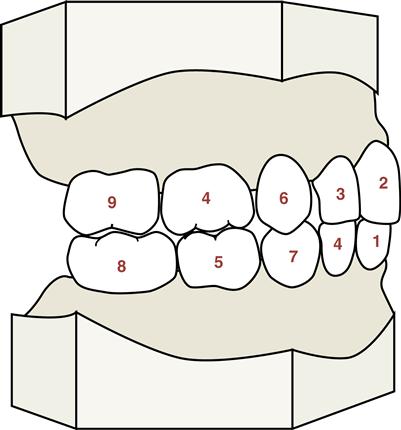
Arch Form
Each dental arch of the permanent dentition is divided into three segments when describing arch form: anterior, middle, and posterior (see Figure 20-1). The anterior segment includes the anterior teeth, the middle segment includes the premolars, and the posterior segment includes the molars. The concept of arch segments allows the arches to overlap slightly so that canines and first molars are cooperating in more than one segment. This arrangement serves to indicate that the canines and first molars function as anchor supports for both arches.
The anterior segment of each dental arch is curved and ends at the labial ridges of the canines. The middle segment is straight and extends from the distal part of the canines to the buccal cervical ridge of the mesiobuccal cusp of the first molar in each arch. The posterior segment creates a straight line, starting from the buccal cusps of the first molars and remaining in contact with the buccal surfaces of the second and third molars.
Phases of Arch Development
Each dental arch goes through phases of development as the permanent teeth erupt and the primary teeth are being shed (see Figure 6-22 for chronological timetable). During this time, the ramus and body of the jaw develops and undergoes lengthening and horizontal growth to achieve its mature form and accommodate the larger permanent teeth.
Phase one occurs when the permanent first molars erupt (see Figure 18-17). These teeth add dramatically to chewing efficiency and jaw development during a period of rapid growth of the child. They help support the jaws while the primary anterior teeth are being shed and the other permanent teeth are erupting. The primate spaces in the primary dentition are still present to allow future space for the permanent teeth (see Chapter 18).
Phase two occurs with eruption of the permanent anterior teeth near the midline of the oral cavity. First, the centrals, then the laterals generally erupt lingually to the primary anterior roots. However, shedding of the primary teeth and jaw growth finally place them labial to the position of the primary teeth they replaced (see Figures 6-26 and 18-17).
In addition, the permanent location of the anteriors is not established until the development of the arch form is complete. Thus, some degree of transient anterior crowding may occur between 8 to 9 years of age and persist until the emergence of the canines, when the space for the teeth is adequate again. However, incisor crowding that persists into a permanent dentition is considered a type of malocclusion (discussed later).
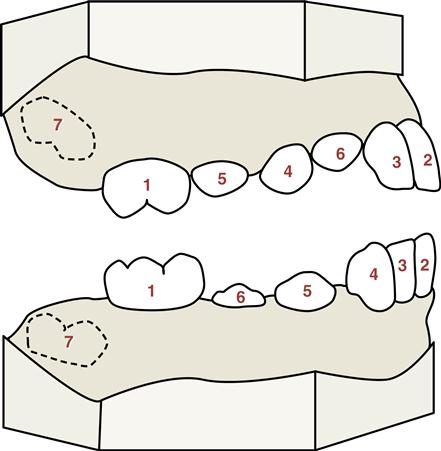
Phase three in the development of the form of the dental arches begins when the premolars erupt anterior to the permanent molars (see Figures 6-27 and 6-28). Developmentally, this is quite significant because the premolars are so much smaller than the primary molars they replace. This difference in size, mesiodistally between the two types of teeth, is called the leeway space (Figure 20-3). The contour of the bone covering the narrower roots of the premolars, in addition to the state of flux of the bone formation in this area, furnishes adjustment for dental arch measurements, making the middle segment of the arches important architecturally. Thus, this space allows the future forward movement of the permanent molars, which is discussed later with regard to the occlusion of the primary teeth.
However, if there is early loss of the primary second molars and impaction of the second premolar, leeway space can become compromised. Also, if permanent second molars erupt before the premolars, the arch perimeter is significantly shortened and occlusal disharmony is likely to occur, as is malocclusion (discussed later), because the second premolar is also unable to erupt. A fixed or removable space maintainer may be used to save this leeway space from the shed primary molars for the permanent premolars (Figure 20-4).
Phase four begins when the canines wedge themselves between the lateral incisors and the first premolars. Contact relations between the teeth are established, and the arch is complete from the permanent first molar forward. Simultaneously, the second molars are due to emerge distally to the first molars and support them during the wedging activity of the canines.
Phase five is the final phase of the development of the final dental arch form and consists of eruption of the third molars. Often the jaw length is not sufficient for eruption of these last teeth and dental treatment plans changes need to be considered (see Chapter 17).
Thus, the usual sequence for eruption of both the primary and permanent dentition is favorable to the development of the arches (Figures 20-5 and 20-6). Keeping this sequence in mind for each dentition is part of the treatment to prevent disruption in patients with primary and mixed dentition. Disruption of this sequence, with overlong retention or too-early loss of primary teeth, may allow complications to occur with the eruption of the permanent dentition. Proper treatment of these cases of disruption in the eruption sequence, and early orthodontic interceptive therapy, increases the chances for a normal occlusion. Panoramic radiographs of the mixed dentition are important in order to monitor tooth eruption sequence and arch development (see Figure 6-27, A).
It is important to note that attrition of the proximal surfaces also reduces the mesial-distal dimensions of the teeth and significantly reduces arch length over a lifetime, which causes crowding or spacing problems after age 40.
Dental Curvatures and Angulations
A common mistake is to assume that the forces of occlusion act on squared and flat teeth in straight lines or planes and that the axes of the teeth are at right angles to their masticatory surfaces. Many dental curvatures and angulations are present in normal occlusion and must be considered.
If imaginary planes are placed on the masticatory surfaces of each dental arch, the arches do not conform to these flat planes; the maxillary arch is convex occlusally, and the mandibular arch is concave (Figure 20-7A). Thus, when the maxillary and mandibular teeth come into centric occlusion, they align along anteroposterior and lateral curves. This anteroposterior curvature is called the curve of Spee, which is produced by the curved alignment of all the teeth and is especially evident when viewing the posterior teeth from the buccal view.
Another curve of the dentition is the curve of Wilson (see Figure 20-7B). This lateral curve results when a frontal section is visually compared to each/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses