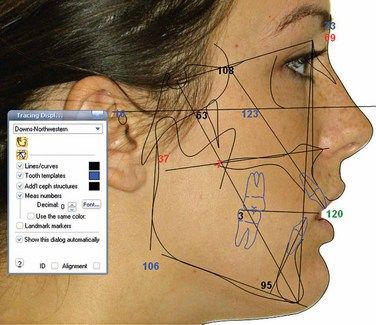
Digital imaging in orthodontics
Imaging is a key tool in the practise of orthodontics, providing clinicians with a documented view of craniofacial and dental structures before, during and after treatment. Photography and dentistry are forever bonded in history by Alexander Wolcott, a New York City dentist who invented the camera in 1839 (Fig 2.1). In 1840, he opened the world’s first commercial photography studio, and this was also the year the world’s first dental journal was printed (Fig 2.2). In 1850, this same journal – the American Journal of Dental Science – published before-and-after photographs of a dental procedure, marking the birth of a new frontier in diagnosis and treatment planning1 (Fig 2.3A and B). The introduction of X-rays in 1895 further revolutionized orthodontics by allowing the visualization of hidden anatomy.
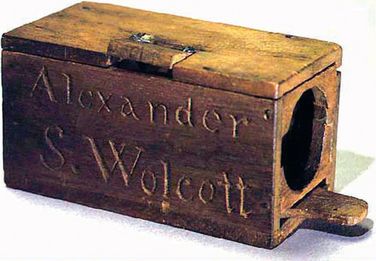
Figure 2.1 Alexander S. Wolcott’s patent model for a daguerreotype camera with concave reflector was the first US patent for a photographic invention. Image courtesy: National Museum of American History (http://historywired.si.edu/object.cfm?ID=462#)
Figure 2.2 The world’s first dental journal, The American Journal of Dental Sciences, published under the auspices of the American Society of Dental Surgeons. Image courtesy: The University of Michigan Dental Library
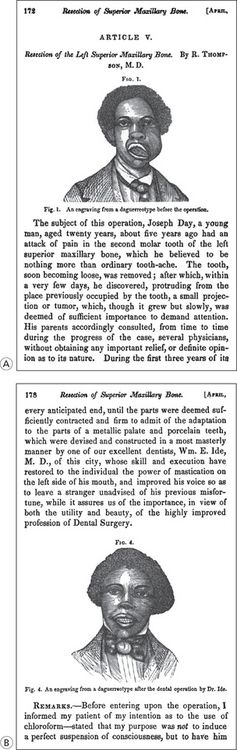
Figure 2.3 The very first before-and-after photographs of a dental procedure to be published: Article V, Resection of the left superior maxillary bone, by R. Thompson, M.D., Vol. X. 1849–50; 172–179. Image courtesy: The University of Michigan Dental Library
One hundred years later, digital imaging technology would resolve the limitations of film photo and radiograph records while paving the way for the three-dimensional (3D) data sets that are revolutionizing the practise of orthodontics. The digital format offers exponential benefits in terms of diagnostics and treatment planning capabilities: the ability to manipulate and enhance data, collect and collate data for the purpose of establishing norms, integrate with other digital data to create a composite patient profile and store, organize and share records instantly are some obvious advantages of digital imaging in comparison to film. Digital technology continues to advance at an alarming rate. In this chapter, we explore the applications of digital photography and radiography in orthodontics, and what this technology holds for the future.
Digital clinical photography
An advantage of digital photographs over traditional film is the ability to take countless photos at no extra cost. This is especially significant when taking clinical photos at the initial exam, given that multiple choices of angles and poses give the clinician more information for evaluation. The other advantages of digital photos include immediate viewing of the images with an option for deletion, image integrity not compromised with age, dust or scratches, zero film processing costs and easy storage, retrieval, duplication and transmission.2 Staff can routinely take a standard set of facial and intraoral photographs in mere minutes. The images can then be reviewed on a computer monitor and, using simple image management software, can be quickly edited, cropped, aligned, rotated, saved and printed in only a few minutes3 (Fig 2.4).
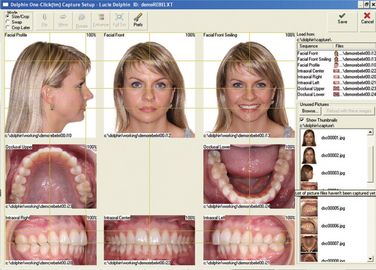
Figure 2.4 Image management software allows the clinician to quickly review, edit, align and otherwise manipulate images on the computer screen for diagnosis and record-keeping. Image courtesy: http://www.dolphinimaging.com
Most current digital cameras will interface nicely with the third-party image management software. There exists software packages designed especially for the dental professional, which offer image organization and patient search capabilities while also integrating with other technologies commonly found in an orthodontic office.
A typical digital imaging system for standard clinical photography consists of a camera, computer, image management software and a colour printer (Fig 2.5). Colour inkjet technology is preferred over laser because of superior colour replication.4 Most 3-megapixel cameras work well for viewing images on a computer screen or monitor, enlarging up to 4 by 5′, which is suitable for various needs including presentations, lectures and printing. Digital cameras can be easily purchased through retailers online. Packages are also available from specialized camera dental supply companies that offer technical and setup assistance, as well as accessories such as intraoral mirrors and lip retractors3.

Figure 2.5 Modern digital imaging system includes a digital camera, a computer, a colour printer and an image management software. Image courtesy: http://www.dolphinimaging.com
Tips for capturing the perfect digital clinical photograph
Quality digital photos are contingent on the protocol of capturing a set of images. It is advised to experiment with different camera settings, document the findings and refine them over time. The basic settings that should be experimented with are aperture, lens speed, zoom factor, capture distance, flash lighting and ambient lighting. Other factors to be considered when designing a photo capture protocol are as follows:
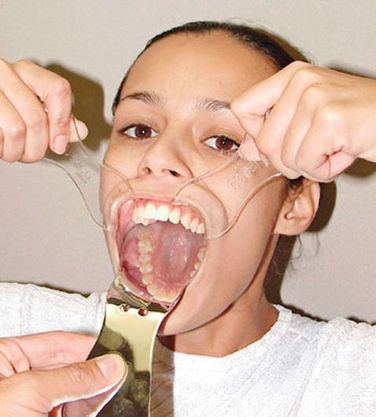
Figure 2.6 Utilizing cheek retractors and occlusal mirrors helps increase visibility of crucial anatomy when taking intraorals. Image courtesy: http://www.dolphinimaging.com
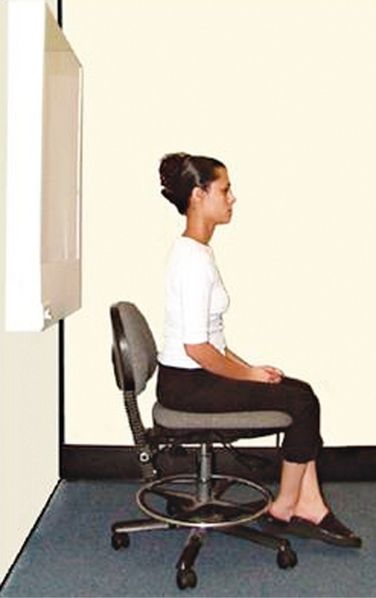
Figure 2.7 A pure background and an adjustable chair that rotates will assist in uniformity among clinical photos. Image courtesy: http://www.dolphinimaging.com

Figure 2.8 Modern digital camera with ring flash. Image courtesy: http://www.dolphinimaging.com
The American Board of Orthodontics has dictated and documented detailed photograph requirements for case report submissions of both facial and intraoral photographs1. Standards for capturing digital dental photos have been developed by entities such as Olympus America and the American Academy of Cosmetic Dentistry. Because the protocols have been rigorously tested and refined, these standards provide an excellent guide for orthodontic staff and laboratory technicians5. Ideally, a customized protocol should be developed by the individual practise to accommodate the specific needs of that practise and then followed uniformly for each patient’s photo sequence.4
Communication: case presentation, patient education and marketing
The inherent versatility of digital images allows for a single image to have multiple uses. An image stored in a patient’s record, for example, can also be placed in a communication to a referring doctor (Fig 2.9), emailed, printed and given to the patient to take home or placed in a presentation program such as PowerPoint or Keynote. This ability to improve communication through visualization empowers the clinician in his r elationships with both patients and colleagues. It has been proven that patients more readily accept treatment when they understand their conditions6 (Fig 2.10).
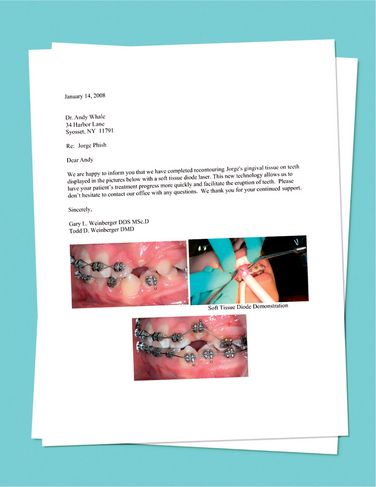
Figure 2.9 Digital records can easily be dropped into letters to patients and referrals for enhanced communication. Image courtesy: Dr Gary and Dr Todd Weinberger, Plainview, New York

Figure 2.10 Easy visualization offered by digital technology allows the orthodontist to easily convey conditions and treatment to patients and parents. Image courtesy: Chang Orthodontics, Los Alamitos, California
Pretreatment and posttreatment images can serve as powerful marketing tools. The ability to create an electronic presentation of your most attractive treatment outcomes to loop on a monitor as a patient waits in the lobby or consultation room is a productive use of otherwise empty time.7 Further, these same images can be used to create advertisements for placement in local media such as newspapers, magazines or even television spots to promote your practise.
Computerized cephalometry: tracing, superimposition and treatment planning
Cephalometry is the system of measuring the bones of the cranium for purposes of scientific analyses.
Introduced in 1931 by B.H. Broadbent (Fig 2.11), cephalometry has been a vital tool in orthodontics. Practitioners rely on this system to diagnose, plan treatment and monitor changes resulting from treatment and growth.8 Because each cephalometric measurement is primarily based on distances, angles and ratios among established landmarks within the cranium, the precise – and consistent – identification of these landmarks is of great value to the practitioner.
Figure 2.11 B.H. Broadbent, father of cephalometrics. Image courtesy: Journal of Clinical Orthodontics
Tracing and analysis
The accuracy of hand-traced cephalometry is contingent on many variables (Fig 2.12).
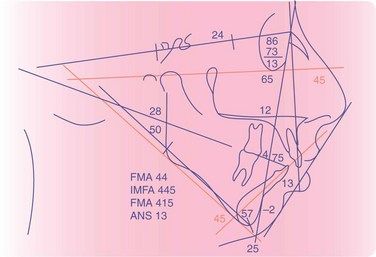
Figure 2.12 Traditional cephalometric tracing done by hand. Source: Reprinted with permission from eMedicine.com, 2009 (http://emedicine.medscape.com/article/839645-overview)
Exposure settings and developing techniques can affect the integrity of the cephalogram and subsequently the quality of the tracing. The ability to digitally enhance and correct for chemical or exposure errors immediately renders the cephalogram viable for tracing while also eliminating the need for a second exposure.9
The manual performance of a single cephalometric tracing and analysis is time consuming. Cephalometric computer programs often contain hundreds of analyses, any number of which can be performed simultaneously under the direction of the operator. This instantaneous access to such a large spectrum of data enhances the clinician’s ability to make a more accurate diagnosis while also saving countless hours of labour10 (Fig 2.13).
Superimposition and treatment planning
The process of superimposing cephalometric tracings inherently contains a margin of variability when aligning traced structures. This error correlates to the consistency and quality of each cephalogram, augmented by the skill of the operator in detecting key structures. Although a fine-tuned X-ray capture protocol and years of practise on the part of the operator greatly reduce this phenomenon, the margin of error still remains. Further accuracy can be improved with digital technology by using specialized software on imported digital versions of the radiographs. This method greatly improves the user’s ability to uniformly orient the images and their structures in a series of time points. Using this combination of technology greatly minimizes the need for additional exposure of X-ray.11
Growth and treatment prediction and visual treatment objective
Establishing a visual treatment objective (VTO) serves multiple purposes for the orthodontist. Fundamentally, its purpose is to forecast both the patient’s growth, when applicable, and the anticipated influence of treatment to create an estimated outcome. The VTO allows the orthodontist to plan the treatment more effectively by keeping his goal in sight and also helps him commu/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses