Chapter 2
Basic Physiology and Anatomy: A Whistle-stop Tour
Aim
The aim of this chapter is to outline the basic principles of physiology and anatomy which are relevant to conscious sedation.
Outcomes
After reading this chapter you should have an understanding of:
-
relevant respiratory and cardiovascular physiology
-
airway obstruction
-
anatomy of commonly used venepuncture sites
-
differences between adult and paediatric patients.
Introduction
To understand fully the principles of safe sedation practice, it is necessary to review certain aspects of physiology, in particular, those relating to the respiratory and cardiovascular systems. A knowledge of the anatomy of the upper airway assists in airway management. Familiarity with the pattern of veins in the antecubital fossa and on the dorsum of the hand is essential for the administration of intravenous sedation.
Respiratory Physiology
The major function of the respiratory system is to ensure continuous effective gas exchange so that oxygen enters the bloodstream and carbon dioxide is removed.
Mechanics, volumes, capacities and flow rates
Quiet breathing is characterised by the rhythmic expansion and relaxation of the lungs and thorax. The diaphragm is the most important muscle of respiration but the intercostal muscles contribute to the increase in the volume of the thorax during inspiration. The accessory muscles of inspiration are not used during quiet breathing. Expiration is normally a passive process resulting from the elastic recoil of the lungs. Active expiration, primarily involving the muscles of the anterior abdominal wall and the intercostal muscles, is seen during exercise and hyperventilation.
The size of the thorax and lungs determines the lung capacities whilst lung volumes are determined by inspiratory and expiratory effort (Fig 2-1). Tidal volume (Vt) is the volume of gas inhaled during a normal inspiration. A fit adult patient at rest normally has a tidal volume of approximately 500 ml. The residual volume (RV) is the volume of air remaining in the lungs at the end of a maximal expiratory effort. RV increases with age and with any decrease in elastic recoil of the lungs. Vital capacity (VC) is the volume of gas entering the lungs following a maximal inspiratory effort. Functional residual capacity (FRC) is the volume of the gas remaining in the lungs at the end of a normal expiration. Functional residual capacity is important because it is a measure of oxygen reserve.
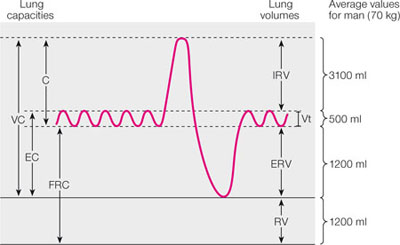
Fig 2-1 Lung volumes and capacities.VC, vital capacity; IC, inspiratory capacity; EC expiratory capacity; FRC, functional residual capacity; IRV, inspiratory reserve volume; ERV, expiratory reserve volume, RV, residual volume; Vt, tidal volume.
Minute volume is the product of the tidal volume and the respiratory rate. A normal adult at rest breathes approximately 12 times per minute. Thus, the minute volume for an adult is usually about 6 litres. These figures provide the sedationist with a physiological basis for estimating the initial fresh gas flow required when using inhalational sedation techniques.
The dead space volume refers to the portion of the airways which is not available for the exchange of gases. Dead space increases with age and reduction in cardiac output. The term alveolar ventilation is used to describe the volume of gas entering the alveoli each minute and taking part in gas exchange. It is important to recognise that a patient who has very shallow breathing (where the tidal volume is less than the dead space volume) is effectively not breathing at all. Hypoventilation is common following the administration of central nervous system (CNS) depressant drugs such as benzodiazepines and opioids.
Pulmonary gas exchange
Gas exchange occurs at the alveolar-capillary membrane, where only two or three cells separate alveolar gas from the bloodstream. Oxygen and carbon dioxide cross the alveolar membrane by diffusion. The rate of diffusion depends upon the:
-
concentration gradient of each gas across the alveolar membrane
-
area available for diffusion
-
rate of removal of oxygen and carbon dioxide.
Oxygen is removed by capillary blood and its rate of transfer is also dependent upon the rate of its chemical combination with haemoglobin. The rate of diffusion of carbon dioxide from capillary blood into the alveolus is 20 times more rapid than that of oxygen in the reverse direction.
Most of the oxygen is transported to the periphery of the body in combination with haemoglobin. Only a very small amount of oxygen is transported dissolved in plasma. Normal adult haemoglobin consists of four protein chains with a haem group attached. The bonding between the chains determines the shape of the haemoglobin molecule which, in turn, influences the affinity of the haemoglobin molecule for oxygen. The affinity of haemoglobin for oxygen is also affected by other variables, e.g. body temperature and pH.
Oxygen combines loosely and reversibly with haemoglobin. Each molecule of haemoglobin can combine with four atoms of oxygen, but the association of each atom alters the affinity of the haemoglobin molecule for subsequent oxygen atoms. This results in the characteristic sigmoid shape of the oxygen dissociation curve (Fig 2-2). The shape of the curve means that large amounts of oxygen are released to the tissues in response to relatively small falls in alveolar oxygen tension, thus maintaining optimum oxygenation of the tissues.
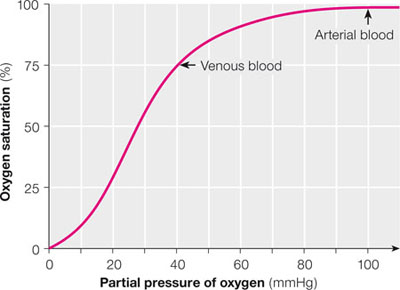
Fig 2-2 Oxygen-haemoglobin dissociation curve.
The oxygen dissociation curve shows the oxygen saturation of haemoglobin on the y-axis and the partial pressure of oxygen (oxygen tension) on the x-axis. The plateau at the top of the curve results from the saturation of the binding sites with oxygen. This provides a potential reserve of oxygen when the partial pressure of oxygen falls. The steep vertical section of the curve allows for optimum loading and unloading of oxygen.
During sedation a pulse oximeter is used to estimate the patient’s arterial oxygen saturation (the y-axis on the oxygen dissociation curve). However, the unremitting hunger of all the cells of the body for oxygen is only satisfied by a continuous supply and adequate partial pressure of oxygen (the x-axis on the curve). The shape of the dissociation curve determines the precise relationship of the axes and thus the relationship between the displayed arterial oxygen saturation (SaO2) and the quantity of oxygen available for cellular respiration. Careful consideration of the curve and the underlying biochemistry will demonstrate the significance of the recommendation that the SaO2 must be maintained above 90% throughout sedation and the immediate recovery period.
Carbon dioxide is carried in the blood in solution, in the form of bicarbonate and attached to protein as carbamino compounds. Carbon dioxide is much more soluble than oxygen and so the quantity of carbon dioxide carried in solution is significant. Most of the carbon dioxide carried in the blood is present in the form of bicarbonate. Bicarbonate is formed as a result of the hydration of carbon dioxide with the production of carbonic acid which, in turn, is ionised to form a hydrogen ion and a bicarbonate ion:

Control of Respiration
Respiration is an automatic process under the control of the brain’s respiratory centre (Fig 2-3). The respiratory centre receives a large number of inputs, including those from the central and periph/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


