Periodontal Diseases
Susanne Perschbacher
Disease Mechanism
Several distinct yet related disorders of the periodontium are collectively known as periodontal diseases. Periodontal diseases are a set of conditions characterized by an inflammatory host response in the periodontal tissues that may lead to localized or generalized alterations in the soft tissues around the teeth, loss of supporting bone, and ultimately loss of the teeth. Periodontal diseases are broadly classified as gingival diseases and periodontitis. Gingival diseases may be dental plaque-induced or non–plaque-induced. Bacterial plaque-associated gingivitis is much more common than non–plaque-induced inflammatory diseases affecting the gingiva, such as viral or fungal infections, mucocutaneous and allergic conditions, and traumatic injuries. Gingivitis manifests as inflammation of the soft tissue surrounding the teeth with gingival swelling, edema, and erythema.
Periodontitis is classified, primarily by the clinical presentation, as chronic, aggressive, and periodontitis as a manifestation of a systemic disease. Other, less common types of periodontal conditions include necrotizing periodontal diseases, periodontal abscesses, and periodontitis associated with endodontic lesions. Periodontitis is distinguished from gingivitis by the clinically detectable destruction of host tissues seen as the loss of soft tissue attachment and supporting bone of the involved teeth. Although periodontitis is always preceded by gingivitis, gingivitis does not always progress to periodontitis.
Dental plaque, which varies greatly in its bacterial composition, plays a primary role in the initiation of periodontitis. Periodontitis-implicated plaque bacteria species, predominantly gram-negative rods and spirochetes, have the ability to colonize on the tooth and root surfaces, spread into the region between the root and the gingival margin, and invade the surrounding tissue in some cases. These bacteria are capable of causing damage to the host tissue either directly, through the release of toxins, or, more significantly, indirectly, by stimulating a host inflammatory reaction. As part of the host response, the release of inflammatory mediators, especially from neutrophils, is responsible for much of the injury to the surrounding soft tissue and stimulation of osteoclastic bone resorption. The resulting inflammatory response causes loss of, and apical migration of, the epithelial attachment, resulting in pocket formation and further enhancing bacterial colonization.
The clinical manifestations of this interplay between bacterial plaque and the host tissues are clinical signs of inflammation. Gingivitis, seen as gingival swelling, edema, and erythema, is the most common first clinical sign. Progression to periodontitis is manifested with pocket formation, the universal presentation of this disease. Other clinical signs include bleeding, purulent exudate, edema, resorption of the alveolar crest, and tooth mobility. Rather than a steady continuous progression from mild to moderate to severe, periodontitis often progresses in bursts. There are cyclic periods of active inflammation and tissue destruction followed by healing and quiescent phases (often years) of no appreciable change. The extent of disease activity is best measured by longitudinal probing of periodontal attachment level. The relative duration of the destructive and quiescent phases depends on the form of periodontitis, the nature of the bacterial pathogens, and the host response. Host factors, such as systemic disease, age, genetic predisposition, immune system status, occlusal trauma, and stress, influence the onset and progression of the disease. Spontaneous remission of the destructive process may occur. The disease usually is painless, and most patients are unaware of its presence. Various forms of therapy are effective, including oral hygiene, scaling, and surgical treatment.
Individuals more prone to periodontal disease include smokers; older individuals; and individuals with poor education, neglected dental care, previous periodontal destruction, and systemic diseases such as diabetes or infection with human immunodeficiency virus (HIV).
The prevalence of periodontal disease in the U.S. population depends on the method of assessment and the threshold used. If loss of attachment by the formation of pockets measuring greater than 4 mm is used, the prevalence is about 23%. The incidence of adult periodontitis increases with age. The prevalence of aggressive periodontitis is less than 1%. Also, it appears that the prevalence of periodontal disease in the United States has declined in the last 30 years, but this may change with an increasing elderly population and an increase in retention of teeth.
Assessment of Periodontal Disease
Contributions of Diagnostic Images
Radiographs play an integral role in the assessment of periodontal disease. They provide unique information about the status of the periodontium and a permanent record of the condition of the bone throughout the course of the disease. Diagnostic images aid the clinician in identifying the extent of destruction of alveolar bone, local contributing factors, and features of the periodontium that influence the prognosis. These images also help in the assessment of the clinical crown-to-root ratio, an important factor that is affected by periodontal bone loss and that influences the prognosis of the tooth and any planned prosthesis. Important features related to periodontal status that may be identified in diagnostic images are listed in Box 19-1.
The clinical and radiologic examinations are complementary. The clinical examination should include periodontal probing, a gingival index, mobility charting, and an evaluation of the amount of attached gingiva. Features that are not well delineated by diagnostic images are most apparent clinically, and features that radiographs best demonstrate are difficult to identify and evaluate clinically. Images are an adjunct to the diagnostic process. Although images can demonstrate advanced periodontal lesions well, other equally important changes in the periodontium may not be seen. Therefore, a complete diagnosis of periodontal disease requires insight from a clinical examination of the patient combined with evidence displayed in the diagnostic image.
Limitations of Intraoral Images
Intraoral images (bitewing and periapical projections) may provide an incomplete presentation of the status of the periodontium. They have the following limitations:
For these reasons, although diagnostic images play an invaluable role in diagnosis and treatment planning, their use must be supplemented by careful clinical examination.
Technical Procedures
The usefulness of intraoral images in the evaluation of periodontal disease can be improved by making images with high technical quality. Interproximal (bitewing), in some cases vertical bitewing, and periapical radiographs are useful for evaluating the periodontium. This material is covered in greater detail in the chapters on projection geometry and intraoral radiographic technique (see Chapters 6 and 7), but the features that are particularly important for imaging the alveolar bone are emphasized here.
Image Receptor Placement and Beam Alignment
The image receptor should be placed parallel with the long axis of the teeth or as near to this ideal position as the size and structure of the mouth permit. The x-ray beam is directed perpendicular to the long axis of the tooth and the plane of the image receptor. These measures result in the best undistorted images of the teeth and periodontal tissues. Interproximal (bitewing) images more accurately record the distance between the CEJ and the crest of the interradicular alveolar bone because the beam is oriented at right angles to the long axis of the teeth with interproximal views, providing an accurate view of the relationship of the height of the alveolar bone to the roots. Periapical views, especially in the posterior maxilla, may present a distorted view of the relationship between the teeth and the height of the alveolar bone because the presence of the hard palate often requires the x-ray tube to be oriented slightly downward toward the posterior teeth to capture the apices of these teeth on the image. In this circumstance, the level of the buccal alveolar bone may be projected near or above the level of the lingual CEJ, making the bone height appear greater than it actually is.
The teeth are depicted in their correct positions relative to the alveolar process when there is (1) no overlapping of the proximal contacts between crowns, (2) no overlapping of roots of adjacent teeth, and (3) overlapping of the buccal and lingual cusps of molars.
In cases where standard interproximal images cannot depict the alveolar crest because of the extent of bone loss, the use of vertical interproximal (vertical bitewing) images may be advantageous. This method uses No. 2 image receptors in a vertical orientation and can be used to cover the molar, premolar, canine, and midline regions. These views can produce the ideal geometry of the interproximal views, while still demonstrating the alveolar bone level when there has been moderate or severe bone loss. Panoramic images are not recommended for evaluation of periodontal disease because the distortion and poor image detail of panoramic views tend to lead the clinician to underestimate minor marginal bone destruction and overestimate major destruction.
For radiography of the alveolar bone, a beam energy of 70 to 80 kVp should be used. Images that are slightly light are more useful for examining cortical margins of bone. A properly collimated beam reduces scattered radiation and improves image contrast.
Special Considerations and Techniques
The dentist must determine the optimal frequency of radiographic examination for patients with periodontal disease. Radiographs of all diseased areas must be available at the beginning of periodontal therapy to aid in diagnosis and allow treatment planning. The extent of continued disease activity, which can be determined clinically, should dictate the frequency of subsequent radiographic examinations.
Computers and image-processing techniques have been used to enhance images to achieve improved detection of alveolar bone loss associated with periodontal disease. The most widely used of these techniques is subtraction radiography (see Chapter 4). The advantage of this method is that it allows better detection of small amounts of bone loss between images made at different times than may be achieved by visual inspection. However, image subtraction is difficult to use because the images must be made with the same orientation of the primary x-ray beam, bone, and image receptor at each examination, which is difficult to accomplish in general practice. The more recent introduction of software programs that can correct for some discrepancies in positioning and alignment in sequential digital images makes subtraction techniques more forgiving. Nonetheless, this diagnostic technique remains primarily a research tool.
Cone-Beam Computed Tomographic Imaging
Current research does not support the use of cone-beam computed tomographic (CBCT) imaging for routine periodontal assessment because it does not offer a significant advantage over conventional imaging techniques when the additional cost and radiation dose are considered. However, the three-dimensional imaging provided by CBCT imaging may allow better visualization of some bony defects that are not well depicted on conventional images. For example, CBCT imaging permits more complete assessment of the architecture of complex vertical defects and craters, furcations, and buccal and lingual plate loss, which are often not seen clearly on interproximal or periapical radiographs (Fig. 19-1). Therefore, CBCT imaging, particularly small-volume and high-resolution scans, may have a role in guiding management of selected lesions, especially when surgery is being considered. The utility of CBCT imaging can be limited by streaking artifacts caused by metallic restorations, which may obscure the details of the bony architecture being examined.
Appearance of Normal Anatomy
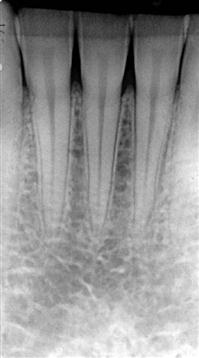
The normal alveolar bone that supports the dentition has a characteristic appearance. A thin layer of opaque cortical bone often covers the alveolar crest. The height of the crest lies at a level approximately 0.5 to 2.0 mm below the level of the CEJs of adjacent teeth. Between posterior teeth, the alveolar crest is parallel to a line connecting adjacent CEJs (Fig. 19-2). Between anterior teeth, the alveolar crest usually is pointed and may have a well-defined cortex (Fig. 19-3). A well-mineralized cortical outline of the alveolar crest indicates the absence of periodontitis activity. However, lack of a well-mineralized alveolar crest may be found in patients with or without periodontitis.
The alveolar crest is continuous with the lamina dura of adjacent teeth. In the absence of disease, this bony junction between the alveolar crest and lamina dura of posterior teeth forms a sharp angle next to the tooth root. The periodontal ligament (PDL) space is often slightly wider around the cervical portion of the tooth root, especially in adolescents with erupting teeth. In this situation, if the lamina dura still forms a sharp, well-defined angle with the alveolar crest, the condition is a variant of normal and is not an indication of disease. The buccal-lingual thickness of alveolar crests varies widely, and it may be very thin coronally. This may appear in a two-dimensional image as an increase in radiolucency toward the crest. These sorts of variations in density alone are not an indication of disease and may be a variation of normal.
Because gingivitis is an inflammatory condition confined to the gingiva, there are no significant changes to the underlying bone, and therefore the appearance of the bone in a diagnostic image is normal.
Imaging Features of Periodontal Disease
For all types of periodontal disease, the changes seen in diagnostic images reflect changes seen with any inflammatory disease of bone. These changes can be divided into changes in the morphology of the supporting alveolar bone and changes to the internal density and trabecular pattern. Changes in morphology become apparent as a result of loss of the interproximal crestal bone and bone overlapping the buccal or lingual aspects of the tooth roots. Changes to the internal aspect of the alveolar bone reflect either a reduction or an increase in bone structure or a mixture of both. A reduction is seen as an increase in radiolucency because of a decrease in number and density of existing trabeculae. An increase in bone is seen as an increase in radiopacity (sclerosis) as the result of an increase primarily in the thickness, density, and number of trabeculae. Similar to all inflammatory lesions of bone, periodontal disease usually has a combination of bone loss and bone formation or sclerosis. However, acute early lesions predominantly display bone loss, whereas chronic lesions have a greater component of bone sclerosis. The following patterns of bone loss may be seen in the diagnostic image as the result of periodontitis.
Changes in Morphology of Alveolar Bone
Early Bone Changes
Early periodontitis appears as areas of localized erosion of the interproximal alveolar bone crest (Fig. 19-4). The anterior regions show blunting of the alveolar crests and slight loss of alveolar bone height. The posterior regions may also show a loss of the normally sharp angle between the lamina dura and alveolar crest. In early periodontal disease, this angle may lose its normal cortical surface (margin) and appear rounded off, havin/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses